HYPONATREMIAINDUCED OSTEOPOROSIS - PowerPoint PPT Presentation
1 / 1
Title:
HYPONATREMIAINDUCED OSTEOPOROSIS
Description:
Findings in rat models of chronic hyponatremia demonstrated that lowering ... subcutaneously implanted mini-pumps (Alzet Model 2004) releasing DDAVP at a rate ... – PowerPoint PPT presentation
Number of Views:109
Avg rating:3.0/5.0
Title: HYPONATREMIAINDUCED OSTEOPOROSIS
1
HYPONATREMIA-INDUCED OSTEOPOROSIS J Barsony1, M
Manigrasso1, H Tam1, Q Xu1, Y Sugimura1, Y Tian1,
DJ Adams2, EA Carter3, HE Resnick3, JG
Verbalis1 1Division of Endocrinology
Metabolism, Georgetown University, 232 Building
D, 4000 Reservoir Road NW, Washington, DC 20007
USA 2Dept. Orthopedic Surgery, New England
Musculoskeletal Institute, University of
Connecticut Health Center, Farmington, CT 06034
USA 3Dept. Epidemiology and Statistics, MedStar
Research Institute, 6495 New Hampshire Avenue,
Hyattsville, MD 20783 USA
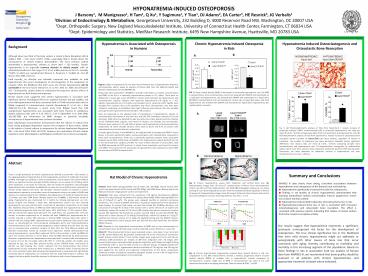
Hyponatremia Is Associated with Osteoporosis in
Humans
Chronic Hyponatremia Induced Osteopenia in Rats
Hyponatremia Induced Osteoclastogenesis and
Osteoclastic Bone Resorption
Background
B
A
Although about one third of the body sodium is
stored in bone (Bergstrom WH Wallace WM. J
Clin Invest 33857, 1954), surprisingly little is
known about the consequences of sodium balance
abnormalities. The most common sodium abnormality
is hyponatremia, defined as serum Na mmol/L. Chronic hyponatremia is an especially
common disorder in elderly people, with an
estimated prevalence in the range of 3.2 to 6.1
million persons in the U.S. annually, 75-80 of
which was asymptomatic (Boscoe A, Paramore C,
Verbalis JG. Cost Eff Resour Alloc 2006, 410-21
). Until recently, no effective and tolerable
treatment was available for mild hyponatremia.
The recent development of oral antagonists of the
vasopressin V2 receptor offers the likelihood
that both acute and chronic hyponatremia will be
correctable in the near future (Annane D. et al.
Am J Med Sci. 2009, Jan337(1)28-36).
Consequently, studies aimed to understand the
long-term adverse effects of hyponatremia are
both timely and important. Recent reports have
suggested that chronic hyponatremia is associated
with significant adverse neurological effects on
cognitive function and gait stability, and even
mild hyponatremia has been associated with a
67-fold increased odds ratio for falling compared
to normonatremic controls (Renneboog B. et al. Am
J Med 2006,11971e.1-8). Moreover, a recent study
from Belgian found that mild asymptomatic
hyponatremia was associated with bone fracture in
ambulatory elderly (adjusted odds ratio of 4.16,
95 CI 2.24-7.71)(Gankam et al. QJM 2008,
101583-588), but information on BMD changes or
potential metabolic consequences of hyponatremia
have yet been described. Early radioisotope
measurements demonstrated that the release of
sodium from bone during prolonged deprivation
requires the resorption of bone matrix, similar
to the release of stored calcium to compensate
for calcium deprivation (Bergstrom WH. J Clin
Invest 1954, 33(6) 867-873). However, the
mechanisms of bone sodium regulation under
physiological or pathological conditions has not
been investigated.
Figure 1 Odds of osteoporosis for the total hip
and femoral neck in hyponatremic relative to
normonatremic adults, based on analysis of human
data from the National Health and Nutrition
Examination Survey (NHANES III). Along with
other parameters, NHANES III provides information
on sodium concentrations and BMD of the hip in a
nationally representative sample of U.S. adults.
There were no differences in mean age, serum
25(OH)D or calcium levels between the
hyponatremic and normonatremic subjects. Subjects
with hypo-and hypercalcemia (mg/dL), hypo-albuminuria (serum creatinine (4.0 mg/dL) were excluded from
analyses due to the possibility that these
characteristics may have been related to
underlying co-morbidities that might influence
bone density. We also excluded participants with
hypernatremia (serum Na 145 mmol/L) Data are
expressed as the adjusted odds of osteoporosis in
hyponatremic, relative to normonatremic
participants at the two sites, with the 95
confidence interval (CI) for the estimates. Odds
ratios are adjusted for age, sex, body mass
index, physical activity, smoking, serum 25(OH)D3
levels (ng/mL), and history of diuretic use
(thiazide and non-thiazide). Diuretics were used
by 11.1 and 6.8 of persons with hyponatremia
and normonatremia, respectively. Of these,
thiazide diuretics were used by 10.5 and 4.7 of
persons with hyponatremia and normonatremia,
respectively. In adults aged 50 years in the
NHANES III, the adjusted odds of osteoporosis
(BMD T-scores below -2.5) were significantly
higher among participants with hyponatremia
compared to those with normonatremia. There was a
statistically significant positive linear
association between serum Na and femoral neck
BMD in the hyponatremic subjects (pin the normonatremic subjects (p0.99). For every
mmol/L decrease in serum Na, total hip BMD
decreased by 0.037 gm/cm2. A similar linear
association was found for femoral neck BMD. The
p-values for the association of hyponatremia with
osteoporosis were 0.043 for total hip and 0.003
for femoral neck.
FIG. 2. Bone mineral density (BMD) is decreased
in chronically hyponatremic rats. (A) BMD in
excised femurs from normonatremic control rats
(treated with DDAVP and maintained on a solid
diet) and hyponatremic rats (treated with DDAVP
and maintained on a liquid diet). (B) BMD in
excised femora from normonatremic control rats on
liquid diet alone, and from hyponatremic rats
(treated with DDAVP and maintained on liquid
diet). Hyponatremia was maintained for 3 months.
A
Fig. 5. (A) Histomorphometric analysis of tibia
from Experiment 1 reveals increase of osteoclast
numbers (TRAP multinucleated cells) in
chronically hyponatremic rats. Data are mean
S.E.M., pnormonatremic and hyponatremic rats. (B)
Histomorphometric analysis of tibia from
Experiment 2 reveals increase of osteoclastic
bone resorption marker (number of osteoclasts per
bone surface), regardless of vitamin D treatment.
The number of osteoclasts per bone perimeter
indicated similar, significant differences (not
shown). Data are mean S.E.M., psamples from normonatremic and hyponatremic rats.
(C) Representative micrographs of undecalcified
lumbar spine 5-µm thick sections show osteoclasts
marked by positive TRAP staining (red).
Osteoclasts are more abundant on trabecular
surfaces in hyponatremic rats than normonatremic
rats. Bars 200 µm.
B
Abstract
Summary and Conclusions
There is a high prevalence of chronic
hyponatremia, defined as serum Na in the aging population, frequently due to the
inappropriate secretion of antidiuretic hormone
(SIADH). Although this condition is often
asymptomatic, recent reports have shown adverse
effects on cognitive function and gait stability,
leading to an increased risk of falling, which
alone represents a risk factor for fractures.
Here we tested the hypothesis that prolonged
hyponatremia also contributes metabolically to
bone loss by activating bone resorption to
release stored sodium from bone. We therefore
initiated studies to evaluate if chronic
hyponatremia represents a secondary cause of
osteoporosis using a rat model of SIADH and
analysis of a representative human database. We
adapted our rat model of hyponatremia to 22
months old male F344 Brown Norway hybrid rats
(F344BN), a well-known model of aging.
Hyponatremia was maintained for 3 months by
infusing desmopressin via mini-pumps (5ng/h) and
feeding a liquid diet. Normonatremic control rats
also received desmopressin, but were pair-fed
with a solid diet of equivalent composition to
the liquid diet. Biweekly measurements of BMD by
DXA demonstrated that hyponatremia induced more
profound progressive bone loss (AP spine -20,
total femur -17.5, proximal tibia -20 per
month) than aging alone (AP spine -3, total
femur -2, proximal tibia -0.7 per month). In
another experiment on 12 months old male F344BN
rats, hyponatremia for 3 months induced a similar
30 decrease in femoral BMD, whereas liquid diet
alone in controls did not change BMD.
Hyponatremia caused severe trabecular and
cortical bone losses, as documented by
micro-computed tomography (µCT), and
histomorphometry. Histomorphometry and in vitro
osteoclastogenesis studies indicted that the bone
loss was due to increased bone resorption.
Analysis of data from the Third National Health
and Nutrition Examination Survey by multiple
linear regression models demonstrated that among
hyponatremics, serum Na explained 14.7 of the
variation in total hip BMD for every one mmol/L
decrease in serum Na, total hip BMD decreased
by 0.037 gm/cm2. Moreover, hyponatremia was
independently associated with increased odds of
osteoporosis (T-scoresratio2.85 95 CI 1.03-7.86, pwere adjusted for age, sex, race, BMI, physical
activity, serum 25(OH)D levels, and history of
diuretic use and smoking. Our results represent
the first demonstration that chronic hyponatremia
causes substantial bone mineral loss, a metabolic
effect increasing fracture risk. Cross-sectional
human data showing that hyponatremia is
associated with significantly increased odds of
osteoporosis are consistent with the experimental
data in rodents, and suggest that bone quality
should be assessed in all patients with chronic
hyponatremia.
Rat Model of Chronic Hyponatremia
Fig. 3. Chronic hyponatremia causes both
trabecular and cortical bone loss. (A)
Representative images from 3D micro-CT
reconstruction of femurs from normonatremic
control rats (7) and from hyponatremic rats
(14). (B) Histological analyses by von Kossa
staining of 5-µm thick longitudinal sections from
the undecalcified distal epiphysis of femora of
young rats. Representative images show thinning
of trabecular bone (arrows) and cortical bone
(arrowheads) in sections from hyponatremic rats.
Bars 1 mm.
- NHANES III data clearly show strong, consistent
associations between hyponatremia and
osteoporosis at the femoral neck and total hip. - Hyponatremia significantly increased the odds
for osteoporosis. - Findings in rat models of chronic hyponatremia
demonstrated that lowering extracellular sodium
concentration induces progressive, severe loss of
bone mineral content. - Hyponatremia induced both trabecular and
cortical bone loss in rats. - Hyponatremia-induced bone loss in rats is
associated with increased osteoclastogenesis and
osteoclastic bone resorption. This effect is
consistent with previous reports indicating that
release of stored sodium from bone requires
resorptive activity.
Animals Male albino Sprague-Dawley rats (6 weeks
old, 250-300g Taconic Farms) were used in two
experiments and 22-month old (500-550g) male F344
Brown Norway hybrid rats (National Institute of
Aging) were used in one experiment. Treatment
Rats were infused with the vasopressin V2R
agonist desmopressin (DDAVP, Aventis) via
subcutaneously implanted mini-pumps (Alzet Model
2004) releasing DDAVP at a rate of 0.25µL/h (5
ng/h). The pumps were replaced monthly to
maintain continuous antidiuresis. This infusion
of DDAVP alone does not produce hyponatremia in
the absence of water loading. To increase fluid
intake, rats were fed a liquid diet (F5400sp,
Bio-Serv) rats consumed on average 45 mL/day of
this solution with a caloric density of 1.6
kcal/mL (72 kcal/d/rat), vitamin D3 content of
3.2 IU/mL (144 IU/d/rat) and calcium content of 2
mg/mL calcium (90 mg/d/rat). Normonatremic
animals received 15g/d of solid diet (F5399
Bio-Serve) with a caloric density of 3.6 kcal/g
(54 kcal/d/rat), vitamin D3 content of 5 IU/g (75
IU/d/rat) and calcium content of 5.2 mg/g (78
mg/d/rat) along with the DDAVP infusion. Other
normonatremic control groups were pair fed with
the same liquid diet, but without DDAVP infusion.
DXA Biweekly in vivo longitudinal measurements
of BMD and ex vivo measurements of excised femora
were performed using a small animal DXA scanner
(Piximus II, Lunar, GE). Micro-CT
Ethanol-preserved femora were evaluated using a
cone-beam X-ray instrument (µCT40, Scanco Medical
AG, Bassersdorf, Switzerland) the at the
University of Connecticut Health Science Center
Micro-CT Core Facility. Images were acquired at
55 kV and 145 µA, collecting 1,000 projections
per rotation at 300 msec integration time. 3D
images were reconstructed using a convolution
back-projection algorithms with Shepp and Logan
filtering, and rendered within a 16.4 mm field of
view at a discrete density of 244,140 voxels/mm3
(isometric 16 µm voxels). Segmentation density
thresholds of 710 mg/cm3 and 595 mg/cm3 were
applied for the cortical and trabecular
compartments of the femur, respectively.
Trabecular analysis included the secondary
spongiosa located 1.6 mm (4 of length) from the
growth plate and extending 3.2 mm proximally.
Our results suggest that hyponatremia represents
a significant, previously unrecognized risk
factor for the development of osteoporosis. The
true clinical significance lies in the likelihood
that even mild chronic hyponatremia might act
additively or synergistically with other causes
of bone loss that occur commonly with aging,
thereby contributing to morbidity and mortality
in this increasing segment of the population.
Based on these findings in rats in association
with our analysis of human data from NHANES III,
we recommend that bone quality should be assessed
in all patients with chronic hyponatremia, and
appropriate treatment initiated where indicated.
Fig. 4. Chronic hyponatremia progressively
reduced bone mineral density in old rats.
Longitudinal in vivo DXA measurements showed a
marked, progressive decline of bone mineral
density (BMD) at multiple sites in hyponatremic
animals compared to normonatremic controls.
Slight loss of BMD in normonatremia rats were at
the rate previously described as an ageing
phenotype. Data are means SEM p