AO Posters - PowerPoint PPT Presentation
Title:
AO Posters
Description:
Affects of Dysphagia and Gastrostomy Feeding on Quality of Life for People with Motor Neurone Disease L. Doylea & K. McElligottb aDepartment of Speech & Language ... – PowerPoint PPT presentation
Number of Views:44
Avg rating:3.0/5.0
Title: AO Posters
1
Affects of Dysphagia and Gastrostomy Feeding on
Quality of Life for People with Motor Neurone
Disease L. Doylea K. McElligottb aDepartment of
Speech Language Therapy, bDepartment of
Nutrition Dietetics, Beaumont Hospital,
Dublin, Ireland
INTRODUCTION Motor Neurone Disease (MND), is a
fatal, progressive, neurodegenerative disease of
unknown aetiology, characterised by death of both
upper and lower motor neurones1. Reduced oral
intake frequently occurs in this patient group
due to factors including dysphagia, poor
appetite, extended meal times, reduced ability to
self-feed, low mood and changes in taste. This
often leads to weight loss, malnutrition and
dehydration which may aggravate muscle weakness,
contribute to respiratory weakness, and perhaps
shorten life span2. The EFNS Task Force3
recommend that people with MND should be referred
to a dietitian as soon as dysphagia appears.
Intervention by a Speech and Language Therapist
is also indicated to suggest alternative
food/fluid consistencies and swallowing
techniques. Initial nutritional interventions may
include food fortification and nutritional
supplementation. Gastrostomy insertion is also a
routinely considered management option for this
patient group. While the evidence for prolonged
survival post-gastrostomy is weakly positive , a
limited number of studies to date suggest that
gastrostomy insertion has a possible positive
effect on QOL4,5.
OBJECTIVE To investigate to what extent dysphagia
and gastrostomy feeding impacts on QOL for people
with MND.
METHOD Over an eighteen month period, people with
MND who were scheduled for gastrostomy insertion
in Beaumont Hospital completed a questionnaire at
three stages. Prior to tube insertion (stage
1), participants (n14) completed the SWAL-QOL,
which is a validated questionnaire regarding the
effects of dysphagia on QOL. This was repeated at
approximately six weeks (stage 2) and six months
(stage 3) following insertion. At stages 2 and
3, participants also completed the RIG-QOL (a
questionnaire devised by the researchers to
examine changes in wellbeing relating to
gastrostomy feeding based on the format of the
SWAL-QOL).
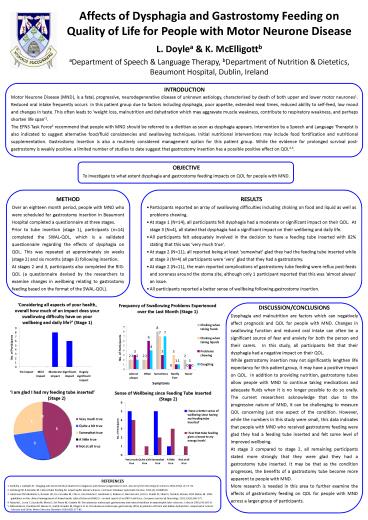
- RESULTS
- Participants reported an array of swallowing
difficulties including choking on food and liquid
as well as problems chewing. - At stage 1 (N14), all participants felt
dysphagia had a moderate or significant impact on
their QOL. At stage 3 (N4), all stated that
dysphagia had a significant impact on their
wellbeing and daily life. - All participants felt adequately involved in the
decision to have a feeding tube inserted with 82
stating that this was very much true. - At stage 2 (N11), all reported being at least
somewhat glad they had the feeding tube
inserted while at stage 3 (N4) all participants
were very glad that they had a gastrostomy. - At stage 2 (N11), the main reported
complications of gastrostomy tube feeding were
reflux post-feeds and soreness around the stoma
site, although only 1 participant reported that
this was almost always an issue. - All participants reported a better sense of
wellbeing following gastrostomy insertion.
Considering all aspects of your health, overall
how much of an impact does your swallowing
difficulty have on your wellbeing and daily
life? (Stage 1)
DISCUSSION/CONCLUSIONS Dysphagia and malnutrition
are factors which can negatively affect prognosis
and QOL for people with MND. Changes in
swallowing function and reduced oral intake can
often be a significant source of fear and anxiety
for both the person and their carers. In this
study, all participants felt that their dysphagia
had a negative impact on their QOL. While
gastrostomy insertion may not significantly
lengthen life expectancy for this patient group,
it may have a positive impact on QOL. In
addition to providing nutrition, gastrostomy
tubes allow people with MND to continue taking
medications and adequate fluids when it is no
longer possible to do so orally. The current
researchers acknowledge that due to the
progressive nature of MND, it can be challenging
to measure QOL concerning just one aspect of the
condition. However, while the numbers in this
study were small, this data indicates that people
with MND who received gastrostomy feeding were
glad they had a feeding tube inserted and felt
some level of improved wellbeing. At stage 3
compared to stage 2, all remaining participants
stated more strongly that they were glad they had
a gastrostomy tube inserted. It may be that as
the condition progresses, the benefits of a
gastrostomy tube become more apparent to people
with MND. More research is needed in this area to
further examine the affects of gastrostomy
feeding on QOL for people with MND across a
larger group of participants.
REFERENCES 1. Karitzky J, Ludolph AC. Imaging and
neurochemical markers for diagnosis and disease
progression in ALS. Journal of the Neurological
Sciences 2001191(1-2)3541. 2. Katzberg HD
Benatar M. Enteral tube feeding for amyotrophic
lateral sclerosis. Cochrane Database Systematic
Review, 2011(1)CD004030. 3. Anderson PM
Abrahams S, Borasio GD, De Carvalho M, Chio A,
Van Damme P, Hardiman O, Kollewe K, Morrison KE,
Petri S, Pradat PF, Silani V, Tomik B, Wasner M
Weber M. EFNS guidelines on the clinical
management of Amyotrophic Lateral Sclerosis
(MALS) revised report of an ENFS task force.
European Journal of Neurology. 201219(3)360-375.
4. Mazzini L, Corra T, Zaccala M, Mora G, Del
Piano M, Galante M. Percutaneous endoscopic
gastrostomy and enteral nutrition in amyotrophic
later sclerosis. J Neurol 1995242695-8. 5.
Mitsumoto H, Davidson M, Moore D, Gad N, Brandis
M, Ringel S et al. Percutaneous endoscopic
gastrostomy (PEG) in patients with ALS and bulbar
dysfunction. Amyotrophic Lateral Sclerosis and
Other Motor Neurone Disorders 20034(3)177-85.