Society of Human Resource Management - PowerPoint PPT Presentation
Title:
Society of Human Resource Management
Description:
Insurance Market Reform As of ... Qualifications for Participating Health Plans require qualified health plans participating in the Exchange to meet marketing ... – PowerPoint PPT presentation
Number of Views:180
Avg rating:3.0/5.0
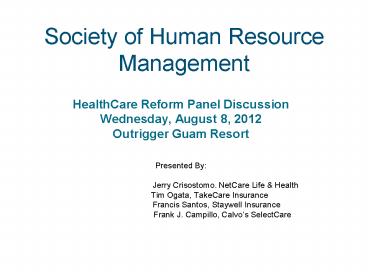
Title: Society of Human Resource Management
1
Society of Human Resource Management
- HealthCare Reform Panel Discussion
- Wednesday, August 8, 2012
- Outrigger Guam Resort
- Presented By
- Jerry Crisostomo. NetCare Life
Health - Tim Ogata, TakeCare Insurance
- Francis Santos,
Staywell Insurance - Frank J.
Campillo, Calvos SelectCare
2
Objective
- Provide a synopsis of and the impact on Health
Plans by the recently upheld Patient Protection
and Affordable Care Act and the Reconciliation
Act (collectively PPACA)
3
AGENDA
- Background on Healthcare Cost
- Overview - Timeline of Reforms
- Insurance Market Reforms
- Expansion of Medicaid
- Premium and Cost-sharing Subsidies
- Tax Changes related to Health Reform
- Employer Requirements
- Individual Mandate
- State Role
- Health Insurance Exchanges
- Medical Loss Ratio Update
- Summary of Impact
4
Health Expenditures for Selected Services
20002015
Projected Projected
TOTAL 2000 2000 2005 2010 2015
Billions 1,353.3 1,353.3 1,987.7 2,879.4 4,031.7
Percent GDP 13.8 13.8 16.0 18.0 20.0
BY TYPE OF SERVICE BY TYPE OF SERVICE BY TYPE OF SERVICE BY TYPE OF SERVICE BY TYPE OF SERVICE BY TYPE OF SERVICE
Hospital care Hospital care 417.0 611.6 882.4 1,230.9
Physician clinical services Physician clinical services 288.6 421.2 610.7 849.8
Other professional services (dental, etc.) Other professional services (dental, etc.) 138.2 200.5 292.6 411.5
Nursing home care Nursing home care 95.3 121.9 160.5 216.8
Home health care Home health care 30.5 47.5 72.3 103.7
Prescription drugs Prescription drugs 120.8 200.7 299.2 446.2
Other medical products Other medical products 49.5 58.1 69.1 83.1
Program admin. net cost of private health insurance Program admin. net cost of private health insurance 81.2 143.0 210.6 289.8
Investment Investment 88.8 126.8 191.3 268.9
Source The Commonwealth Fund Data from A.
Catlin et al., National Health Spending in 2005
The Slowdown Continues, Health Affairs,
Jan./Feb. 2007 26(1)14253 C. Borger et al.,
Health Spending Projections Through 2015
Changes on the Horizon, Health Affairs Web
Exclusive (Feb. 22, 2006)w61w73.
5
U.S. National Healthcare Expenditures
6
(No Transcript)
7
Global Payments
HEALTH SPENDING AS GDP AND PER CAPITA
8
Comparative Cost of ProceduresUSA vs. other
Countries
http//www.washingtonpost.com/wp-srv/special/busin
ess/high-cost-of-medical-procedures-in-the-us/
9
Average Annual Premiums for Single and Family
Coverage, 1999-2011
Estimate is statistically different from
estimate for the previous year shown
(plt.05). Source Kaiser/HRET Survey of
Employer-Sponsored Health Benefits, 1999-2011.
10
PPACA Has Three Basic Goals
- Expands Health Insurance Coverage. 94 of all
Americans covered by 2019 - Strong regulations and oversight of the insurance
industry - Control cost, particularly for Medicare
- __________________________________
- But what is the intended consequence?
- A Single Payer System
11
(No Transcript)
12
12
13
2010 Consumer Focused Provisions
- Grandfathered Plans
- Early Retiree Reinsurance Program
- Online Resources
- Appeals and External Review
- Cancellation of Coverage (Recissions)
- Dependent Coverage up to age 26
- Doctor Choice
- Restriction on Annual Limits and a Ban Lifetime
Limits - Emergency Care
- Prohibition in favor of highly paid individuals
- No pre-existing conditions for members under age
19 - Preventive Care Services without cost share
- Temporary High Risk Pool
- No Unreasonable premium increases
- Small Business Tax Credit
14
2011 Preparing for Future Provisions
- Health Savings Account Distribution Tax Penalty
- Medical Loss Ratio
- -80 for Individual and Small Group
- -85 for Large Group
- Eliminating Medicare Part D Donut Hole
- Over The Counter Drug
- Rate Review Begins
15
2012 Creating Administrative Standards
- Insurers are required to standardize documents
and implement new reporting requirements - Encouraging Integrated Health Systems
- Summary of Benefit and Coverage
- Quality of Care Reporting
- Reducing paperwork and administrative costs
- Patient-Centered Outcome Research Fee
16
2013 Final Preparations
- Focus on the final preparations for the new state
health insurance exchanges. - Flexible Spending Account Limits
- Expanded Authority to Bundle Payments
- Increase Medicare Part A tax on wages by 0.9
- Higher Medicare payroll tax of 2.35 for
individuals making 200K/250K
17
2014 Key Health Reform Provisions Take Effect
- PPACA comes to a cresendo in 2014. Many key
changes will be implemented - Health Benefit Exchanges
- Mandates (Individual, Employer)
- No Pre-existing Conditions for ALL adults
- Clinical Trials
- Guaranteed Availability, Renewability Rating
Variations - Limit on Waiting Periods
- Auto Enrollment Implemented
- Health Care Excise Tax
- Increases access to Medicaid
- No Annual Limits on Coverage
18
2015 Continuing Innovation and Lower Health
Costs
- Establishes an Independent Payment Advisory Board
aimed at extending the solvency of Medicare - Paying Physicians based on Value and not Volume.
A new provision will tie physician payments to
the quality of care they provide.
19
2016 Electronic Standards
- Health Claims Attachments standards for
electronic transmission of health related
documents - Encounter, enrollment, disenrollment, premium
payment and referral certification standards
20
2018 New Tax on Rich Benefits
- PPACA imposes a Cadillac Excise Tax on plans with
rich benefits
21
2020 Medicare Donut Hole
- Donut Hole coverage gap in Medicare prescription
drug benefit is fully phased out. Seniors will
continue to pay the standard 25 of their drug
costs until they reach the threshold for Medicare
Catastrophic coverage
22
2010 - 2011 PPACA REQUIREMENTS
(NetCare's Experience)
Unlimited Lifetime
Max - 1.44
Non-Participating Emergency
Preventive
Services -3.48
Care
3.83
OB/GYN
Services -1.19
Essential Benefits
No Annual Limits - 2.45
Dependent Coverage Up to age 26 - 1.82
Annual Dollar Plan Max
Pre-Existing Coverage
Increase - 3.62
For Dep age lt19
2.31
Preventive Care Coverage
Essential Benefit Coverage - No Annual Limits
Increase in Annual Dollar Plan Max
Pre-Existing Condition Waiver for Dep age lt19
Extended Coverage for Dep age gt26
No Referrals for OB/GYN Services
Emergency Coverage at Non-Participating
Facilities
Unlimited Lifetime Maximum
23
(No Transcript)
24
PPACA Supreme Court Decision
25
Insurance Market Reform Effective Date of
Enactment 03/23/10
- Annual Rate Review (individual group markets)
- Secretary states to establish process for
annual review of unreasonable increases in
premiums for health insurance coverage in the
individual and small group markets. - Insurer must submit prior justification for
unreasonable premium increases and post on
website. - State to provide Secretary with trends on premium
increases and whether particular insurer should
be excluded from Exchange based on pattern or
practice of excessive or unjustified premium
increases.
26
Insurance Market Reform 90 Days of Enactment
06/23/10
- z? State High Risk Pool- Not applicable
territories - z ? Secretary to establish high risk pool for
individuals with pre-existing conditions who
do not have creditable coverage. - z ? Will run through 1/1/14 (when Exchange is up
and running) - z ? If Secretary finds insurer or employer has
encouraged individuals to disenroll in order
to join high risk pool, insurer/employer must
reimburse expenses. - z? Early Retiree Reinsurance- Not applicable to
territories - z ? Secretary to establish temporary retiree
reinsurance program to reimburse claims of
retirees age 55 and older who are not
Medicare-eligible. Program would pay 80 of
eligible claims. - Z ? Plan only may use reimbursement to reduce
costs (premiums, copayments, out-of-pockets
costs, etc.).
27
- Insurance Market Reform
- Six Months from Enactment - 9/23/10
- Annual Lifetime Limits (insured self-funded)
- No annual or lifetime limits on essential
benefits (ok for nonessential benefits). - May have annual limits on certain restricted
benefits set by Secretary, prior to 1/1/14. - No rescissions except for fraud
- Dependent Coverage to age 26 (insured
self-funded) - Not required to cover child of adult child
dependent.
28
- Insurance Market Reform
- Six Months from Enactment 9/23/10
- Prior to 1/1/14, group not required to cover if
dependent is eligible to enroll in
employer-sponsored coverage. - Secretary to issue regulations to define
dependent. - No Pre-existing Condition Exclusion for enrollees
under age 19 (insured self-funded) - Applies to all enrollees as of 1/1/14.
29
- Insurance Market Reform
- Six Months from Enactment 9/23/10
- Preventive Health (insured self-funded)
- Must cover preventive health without cost sharing
- Nondiscrimination Based on Income (insured)
- May not discriminate in favor of highly paid
individuals under IRC105(h) (for insured
coverage already applies to self-funded) - Choice of Providers (insured self-funded)
- Must allow child to designate pediatrician as
primary care provider. - May not require authorization or referral for
participating OB-GYN.
30
Insurance Market Reform Six Months from Enactment
9/23/10
- Emergency (insured self-funded)
- Must cover emergency services without prior
authorization and treat as in-network. - Appeals External Review (insured self-funded)
- Must have internal review process.
- ? Must have external review that either meets
NAIC Uniform External Review Model Act or
standards set by Secretary. Secretary may deem
external review process in operation on date of
enactment as compliant. - Must provide continued coverage pending outcome
of appeals.
31
Insurance Market ReformSix Months from
Enactment 9/23/10
- ANNUAL LIMITS
- Restricted annual limits permitted with respect
to essential health benefits until plan years
beginning on or after January 1, 2010. - Restricted annual limits are applied on a per
person basis - Restricted annual limits are
- For plan or policy years beginning on or after
September 23, 2011 but before September 23, 2012
1.25M - For plan or policy years beginning on or after
September 23, 2012 but before January 1, 2014
2M - For plan or policy years beginning on or after
January 1, 2014 Unlimited
32
Insurance Market ReformSix Months from
Enactment 9/23/10
- ESSENTIAL HEALTH BENEFITS
- The rules defining essential health benefits
have yet to be finalized by each state and
territory based on a benchmark plan. - Until the rules defining essential health
benefits are finalized and benchmark plans are
selected, HHS will take into account good faith
efforts to comply with a reasonable
interpretation of the term essential health
benefits. - For this purpose, a plan or issuer must apply the
definition of essential health benefits
consistently.
33
Insurance Market Reform Two Years from Enactment
- 2012
- Summary Documents (insured self-funded)
- Within 24 months of enactment, insurers must
provide summary of benefits and coverage using a
format issued by HHS (including uniform
definitions). - Limited to 4 pages and must state whether
provides minimumessential coverage and whether
meets 60 actuarial value. - In addition to ERISA SPD requirements.
- Must provide 60-day prospective notice of plan
changes.
34
- Insurance Market Reform
- As of 1/1/14
- No Pre-Existing Condition Exclusions (insured
self-funded) - Applies earlier for enrollees under age 19.
- Limit on Waiting Periods (insured self-funded)
- Waiting period cannot exceed 90 days.
- HIPAA Wellness Reward increased from 20 to 30
(and - Secretary has discretion to increase to 50)
35
- Insurance Market Reform
- As of 1/1/14
- May not discriminate based on health status
(insured self- - funded).
- Cost-sharing limits tied to HSA amounts (5,000
individual / - 10,000 family) (insured self-funded).
- For small group market, deductible limit is
2,000 individual / - 4,000 family (insured).
- Expanded coverage of clinical trials (may not
impose - additional conditions) (insured self-funded).
- Must cover essential benefits (insured /
individual small - group markets only).
36
Insurance Market Reform As of 1/1/14 Insured Only
? Guaranteed Access Renewability ? Rating Restrictions (individual small group markets large group if offered through Exchange) ? May not vary rate except for ? Individual versus family ? Rating Area ? Age (limit of 3 to 1) ? Tobacco Use (limit of 1.5 to 1) ? Guaranteed Access Renewability ? Rating Restrictions (individual small group markets large group if offered through Exchange) ? May not vary rate except for ? Individual versus family ? Rating Area ? Age (limit of 3 to 1) ? Tobacco Use (limit of 1.5 to 1)
37
Expansion of Medicaid
- Expand Medicaid to all non-Medicaid eligible
individuals under age 65 with incomes up to 133
FPL based on modified adjusted gross income - All newly eligible adults will be guaranteed a
benchmark benefit package that meets the
essential health benefits available through the
Exchanges - To finance the coverage for the newly eligible,
states will receive - 100 federal funding for 2014 2016
- 95 federal financing in 2017
- 94 federal financing in 2018
- 93 federal financing in 2019
- 90 federal financing in 2020 and subsequent
years - Increase Medicaid payments in fee-for-service and
managed care for primary care services provided
by primary care doctors to 100 of the Medicare
payment rates for 2013 and 2014
38
Premium and Cost-Sharing Subsidies to Individuals
- Eligibility
- Availability of premium credits and cost-sharing
subsidies through the Exchanges to U.S citizens
and legal immigrants who meet income limits - Premium Credits
- To eligible individuals and families with
incomes between 133-400 FPL to purchase
insurance through the Exchanges - Tied to the second lowest cost silver plan in the
area - Contributions limited to the following
percentages of income for specified income
levels - Up to 133 FPL 2 of income
- 133-155 FPL 3 4 of income
- 150-200 FPL 4 6.3 of income
- 200-250 FPL 6.3 8.05 of income
- 250-300 FPL 8.05 9.5 of income
- 300-400 FPL 9.5 of income
- Increase the premium contributions for those
receiving subsidies annually - Provisions related to the premium and
cost-sharing subsidies are effective January 1,
2014
39
Premium and Cost-Sharing Subsidies to Individuals
- Cost-sharing subsidies
- To eligible individuals and families
- Reduce cost-sharing amounts and annual
cost-sharing limits - Have the effect of increasing the actuarial value
of the basic benefit plan to the following
percentages of the full value of the plan for the
specified income level - 100-150 FPL 94
- 150-200 FPL 87 of income
- 200-250 FPL 73 of income
- 250-300 FPL 70 of income
- Verification
- Required for both income and citizenship status
in determining eligibility for the federal
premium credits - Subsidies and abortion coverage
- Ensure that federal premium or cost-sharing
subsidies are not used to purchase coverage for
abortion if coverage extends beyond saving the
life of the woman or cases of rape or incest.
40
Premium and Cost-Sharing Subsidies to Employers
- Small business tax credits
- Phase I (2010 2013),
- Provide a tax credit of up to 35 of employers
contribution toward employees health insurance
premium if employer contributes at least 50 of
the total premium cost or 50 of a benchmark
premium - Full credit will be available to employers with
10 or fewer employees and average annual wages of
less than 25,000. - Phase II (2014 and later)
- For eligible small business that purchase
coverage through the state Exchange, provide a
tax credit of up to 50 of the employers
contribution toward employees health insurance
premium if the employer contributes at least 50
of the total premium cost. - Credit will be available for two years
- Full credit will be available to employers with
10 or fewer employees and average annual wages of
less than 25,000. - Reinsurance program
- Created temporarily for employers providing
health insurance coverage to retirees over age 55
who are not eligible for Medicare - Will reimburse employers or insures for 80 of
retire claims between 15,000 and 90,000 - Payments from the reinsurance program will be
used to lower the costs for enrollees in the
employer plan - Effective 90 days following the enactment through
January 1, 2014
41
TAX CHANGES
- W-2 reporting of value of employer-sponsored
health - benefits, effective in 2011
- ? Employee salary reduction contributions to
FSAs limited - to 2,500, indexed to CPI-U, effective 2013
- Restrictions on the reimbursement of
over-the-counter - (OTC) drugs from FSA, HSA, or HRA, effective
in 2011 - Exemption for prescribed OTC drugs difficult to
- administer
- Increase additional tax on distributions from
HSAs that are not used for qualifying
medical expenses from 10 - to 20 of the distribution, effective in 2011
42
TAX CHANGES - Individuals
- Additional Taxes on High Income Individuals
- Additional HI payroll tax of 0.9 for wages
- in excess of 250,000 (joint filers) and
- 200,000 (all others)
- Effective for remuneration received after
- December 31, 2012
- Also 3.8 tax on same filers on investment income
43
TAX CHANGES - Individuals
- Itemized deduction for medical expenses
- Floor for claiming goes from 7.5 to 10 of AGI
- Effective tax years beginning after December 31,
2012 - o ? Delayed effective date to 2017 for those age
65 or - over
- Tax on indoor tanning services
- 10 of amount paid
- Effective for services performed after July 1,
2010
44
TAX CHANGES Others
- New fees on health care companies beginning in
2011 - Pharmaceutical manufacturing companies
- 2014 -- 8 billion 2015, 2016 -- 11.3 billion
2017 -- 13.7 billion 2018 -- 14.3 billion - Medical device manufacturers
- ? 2.9 tax on sale of medical device after
12/31/12 - Health insurance companies (certain nonprofits
exempted) - ? 2014 -- 8 billion 2015 -- 11.3 billion
2016 -- 11.3 - billion 2017 -- 13.9 billion 2018 -
14.3 billion - Thereafter indexed to medical cost
growth - Fee is allocated based on market share
- Fee expected to be passed on to consumers as
higher health care costs
45
- TAX CHANGES
- Others
- Health Insurance Company Compensation
- Denial of deduction for compensation in excess of
- 500,000 for health insurance providers
- Applies to deferred compensation also
- No performance-based compensation exception
- Applies to more than top-5 executives
- Officer, director or employee
- Anyone who provides services to insurer
- What does this mean for doctors?
46
Employer Requirements Currently unknown if
applicable to territories
- ? Applies to employers who employed an average
of at least 50 full- time employees on business
days during the preceding calendar year
(full-time employee average of 30 hours per
week). - Must pay a fee if coverage IS NOT offered to
full-time employees AND any full-time employee
receives premium assistance from federal
government. - 2,000 annual fee for each full-time employee
employed (minus the first 30 employees) - Must pay a fee if coverage IS offered to full
time employees BUT any full-time employee still
receives premium assistance from federal
government. - the lesser of 3,000 annual fee for each employee
receiving premium assistance OR 2,000 annual fee
per employee for each full-time employee employed
(minus the first 30 employees) - Generally effective beginning in 2014.
47
Employer Requirements Other Provisions Currently
unknown if applicable to territories
- Automatic Enrollment
- Employers with more than 200 employees that offer
coverage - must automatically enroll new full-time employees
in - coverage with the opportunity to opt-out.
- Notification To Employees Regarding Exchange
(effective 3/1/13) - Cafeteria Plan
- Exchange coverage is considered qualified under
a cafeteria plan only for qualified employers
that are permitted to offer a choice of Exchange
plans to their employees. - W-2 Reporting
- Employers must report, for information purposes,
the - aggregate cost of employer-sponsored coverage on
an - employee's W-2.
48
Employer Requirements Other Provisions Currently
not known if applicable to territories
- Automatic Enrollment
- Employers with more than 200 employees that offer
coverage - must automatically enroll new full-time employees
in - coverage with the opportunity to opt-out.
- Notification To Employees Regarding Exchange
(effective 3/1/13) - Cafeteria Plan
- Exchange coverage is considered qualified under
a cafeteria - plan only for qualified employers that are
permitted to offer a - choice of Exchange plans to their employees.
- W-2 Reporting
- Employers must report, for information purposes,
the - aggregate cost of employer-sponsored coverage on
an - employee's W-2.
49
Employer Requirements Vouchers Currently not
known if applicable to territories
- ? Free Choice Voucher Used by "Qualified
Employees" to purchase qualified health plan
coverage through the Exchange. - Qualified employees those whose required
contribution for minimum essential coverage
through the employers plan exceeds 8 but is
less than 9.5 of the employees taxable income
for the year, whose household income is less than
400 FPL and who do not participate in a health
plan offered by the employer. - Amount The most generous amount the employer
would have contributed for self-only (or family,
if applicable) coverage under the employers
plan. - Employers may deduct the amount paid in vouchers
as an amount paid for personal services. - Employees that receive free choice vouchers do
not trigger the fee on employers who have
employees receive coverage through an Exchange.
50
Individual Mandate Penalty Currently not known
if applicable to territories
- ? Individuals are required to maintain "minimum
essential coverage" for each month beginning in
2014. Failure to maintain coverage for the entire
year will result in a penalty. The monthly
penalty is 1/12thof the greater of - For 2014, 95 per uninsured adult in the
household or 1 of household income over the
filing threshold, - For 2015, 325 per uninsured adult in the
household or 2 of household income over the
filing threshold, and - For 2016 and beyond, 695 per uninsured adult in
the household or 2.5 of household income over
the filing threshold. - ? The penalty will be one-half of the amounts
listed above for individuals under 18. - ? The total household penalty may not exceed
(i) 300 percent of the per adult penalty or (ii)
the national average annual premium for bronze
level health coverage offered through the
Exchange.
51
Individual Mandate - Exceptions
- Exceptions to the individual responsibility
requirement - religious exemptions,
- individuals not lawfully present in the United
States, - incarcerated individuals,
- those who cannot afford coverage (required
contributions - toward coverage exceed 8 of household income),
- taxpayers with income under 100 percent of the
poverty - level,
- those who have received a hardship waiver, and
- those who were not covered for a period of less
than three - months during the year.
52
- STATE ROLE
- Create an American Health Benefit Exchange and a
Small Business Health Options Program (SHOP)
Exchange for individuals and small businesses and
provide oversight of health plans with regard to
the new insurance market regulations, consumer
protections, rate reviews, solvency, reserve fund
requirements, premium taxes, and to define rating
areas. - Enroll newly eligible Medicaid beneficiaries
into the Medicaid program no later than January
2014. - Establish an office of health insurance consumer
assistance or an ombudsman program to serve as an
advocate for people with private coverage in the
individual and small group markets. - Permit states to create a Basic Health Plan for
uninsured individuals with incomes between 133
and 200 FPL in lieu of these individuals
receiving premium subsidies to purchase coverage
in the Exchanges.
53
- HEALTH INSURANCE EXCHANGES
- Create state-based American Health Benefit
Exchanges and Small Business Health Options
Program (SHOP) Exchanges - Administered by a governmental agency or
non-profit organization - Individuals and small businesses with up to 100
employees can purchase qualified coverage. Permit
states to allow businesses with more than 100
employees to purchase coverage in the SHOP
Exchange beginning in 2017. - (Funding available to states to establish
Exchanges until 2015). - Public Plan Option Require the Office of
Personnel Management (OPM) to contract with
insurers to offer at least two multi-state plans
in each Exchange. At least one plan must be
offered by a non-profit entity and at least one
plan must not provide coverage for abortions
beyond those permitted by federal law.
54
- HEALTH INSURANCE EXCHANGES
- Four benefit categories of plans plus a separate
catastrophic plan to be offered through the
Exchange in the individual and small group
markets - Bronze Plan represents minimum creditable
coverage and provides the essential health
benefits (EHB), cover 60 of the benefit costs of
the plan with an out of pocket limit equal to the
Health Savings Account current law limit - Silver Plan provides the EHBs, covers 70 of the
benefits costs of the plan, with the HSA out of
pocket limits - Gold Plan provides the EHBs, covers 80 of the
benefits costs of the plan with the HSA out of
pocket limits - Platinum Plan provides the EHBs, covers 90 of
the benefits costs of the plan with HSA out of
pocket limits - Catastrophic Plan available to those up to age 30
or to those who are exempt from the mandate to
purchase coverage
55
- HEALTH INSURANCE EXCHANGES
- Insurance Market and Rating rules
- require guarantee issue and renewability and
allow rating variation based only on age, premium
rating area, family composition, and tobacco use
in the individual and small group market - require risk adjustment in the individual and
small group markets and in the Exchange
(effective January 1, 2014) - Qualifications for Participating Health Plans
- require qualified health plans participating in
the Exchange to meet marketing requirements, have
adequate provider networks, contract with
essential community providers, be accredited with
respect to performance on quality measures, use a
uniform enrollment form and standard format to
present plan information - require qualified health plans to report
information on claims payment policies,
enrollment, disenrollment, number of claims
denied, cost-sharing requirements, out of network
policies and enrollee rights in plain language
56
Medical Loss Ratio Update 2012
57
Calculations Based on Aggregation Set
- How are rebates determined?
- MLR calculation will be performed for each
Aggregation Set - Aggregation sets are based on policyholder
groupings as determined by a legal entity, by
state of issue and segment (Individual, Small
Group or Large Group) - Group policies placed into the appropriate state
based on - contract issuance state situs where policy is
issued - Rebates are calculated based on the MLR of the
Aggregation Set as a whole - NOT solely on the experience of the individual
group policy - NOT solely on the claim experience of individual
members - Rebates are based on the experience of the
Aggregation Set, not on the claim experience of a
specific employer or individual.
58
Rebate Calculation
Incurred claims plus expenses for activities that
improve health care quality and credibility
adjustments Premium revenue less Federal State
taxes, premium taxes, licensing regulatory fees
and adjustments for state and federal high risk
pools, I any.
Medical (numerator) Premium (denominator)
Quality Improvement Activities (examples)
- Included
- Case Disease Management, Discharge Planning
- Nurse line
- Fraud Abuse (lesser of expenses and recoveries)
- Certain Wellness Expenses
- Prospective Utilization Review
- HIT Expense for Quality
- Some ICD-10 Implementation Costs
- Excluded
- HIPAA Implementation Costs
- Concurrent Retrospective Utilization Review
- Provider Credentialing
- Provider Contracting / Network Management
- Claims Adjustment Expensesexcluded from medical
59
Distribution of Rebates
- Are there restrictions on how a group
policyholder can use the - rebate payment received from the health
insurer? - Yes, restrictions depend on whether the plan is a
federal government plan, a non-federal government
plan, a plan governed by ERISA or a plan that is
neither a government plan nor governed by ERISA.
The requirements are outlined below.
Group Policyholder PlanCategories Requirements on Group Policyholders for Use and Distribution of Rebates
ERISA plans Most businesses are ERISA including employee welfare benefit plans. These are plans sponsored by private sector employers, unions or associations. Most private sector plans are governed by ERISA. ERISA plans are subject to the jurisdiction of the Department of Labor (DOL), which has provided guidance to assist plan sponsors in determining how MLR rebates may be used. There are very specific rules for ERISA plans around return of premium. DOL Technical Release 2011-04 (December 2, 2011).
Federal Governmental plans (like FEHBP) The use of the rebate dollars would be governed by the legal requirements under federal law applicable to the government agency.
60
Distribution of Rebates
Group Policyholder PlanCategories Requirements on Group Policyholders for Use and Distribution of Rebates
Non-Federal Governmental Plans (states, counties, municipalities, public schools) Group policyholder must use the amount of the rebate that is proportionate to the total amount of premium paid by all subscribers under the group health plan option for which the rebate applies, in one of the following ways Used to reduce the premium for the subsequent policy year (2013), for all subscribers (2012), who are covered at the time the rebate is received by the policyholder. Used to reduce the premium for the subsequent policy year (2013), for all subscribers under the group health plan option for which the rebate is issued, who are covered at the time the rebate is received by the policyholder. A cash refund to subscribers enrolled in the group health plan option. With respect to the three (3) options above, the reduction in future premium or the cash refund provided may at the option of the group policyholder be Divided evenly among such subscribers, Divided based on each subscribers actual contribution to premium, or Apportioned in a manner that reasonably reflects each subscribers contribution to premium.
Non-ERISA, non- governmental plans (churches, tribes) Group policyholder will only receive rebate dollars if they execute a written assurance that outlines how the rebate dollars are to be used. If the group policyholder in this situation does not execute the written assurance, then the entire rebate will be distributed to subscribers.
Reduction would be based on subscriber portion of
premium Note Group policyholders should consult
their company attorney and tax advisor
61
Impact to Guam
- Insurance Market Reforms will benefit consumers
including unreasonable rate increases - Access and Affordability through Health Exchange
- Increased Funding for Medicaid up to 58 Million
in 2019 - Medical Loss ratio Rebates
- 21 New Taxes will be implemented
62
Impact to Guam
- The bottom line is the Federal Government is
about to assume MASSIVE new powers - These powers include designing insurance plans,
telling people where they can go for coverage and
how much insurers are allowed to charge - How then are doctors and hospitals suppose to
practice medicine?
63
Health Care Reform
Questions?