Hyperbilirubinemia - PowerPoint PPT Presentation
1 / 49
Title:
Hyperbilirubinemia
Description:
Bilirubin Historical perspective: Neonatal jaundice has been recognized for centuries First anatomic description of jaundiced brains by Johannes Orth in 1875. – PowerPoint PPT presentation
Number of Views:1145
Avg rating:3.0/5.0
Title: Hyperbilirubinemia
1
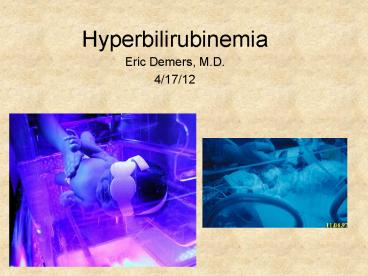
Hyperbilirubinemia
- Eric Demers, M.D.
- 4/17/12
2
Fetal Development
RBC production begins 2-3 wks (yolk
sac). Proceeds to liver (6 wks) and bone marrow
(20 wks). Bilirubin present at 14 wks (in
amniotic fluid at 12 wks). UVC bili 1.5 mg/dL _at_
20 wks bili 1.8 mg/dL _at_ term Fetal
RBC lifespan 45-90 days (Premie 35-50
days). Placenta can remove bilirubin, not
biliverdin.
3
Overview
Hyperbilirubinemia occurs in 80 term infants and
virtually all premature infants. Imbalance
between bilirubin production and elimination. 1
g Hemoglobin yields 34 mg bilirubin. Bilirubin gt
25 mg/dL occurs 1 in 750 infants. Bilirubin gt 30
mg/dL occurs in 1-3 per 10,000 infants.
4
Dennery, PA, et al. NEJM 2001, 344(8)581-90.
5
Heme Oxgenase (HO)
HO found in tissue macrophages, GI tract, and
reticuloendothelial system. Rate-limiting step
in bilirubin production. Inhibited by Tin
Mesoporphyrin.
Dennery, et. al. J. Perinat. 2001 21s17-20.
6
Bilirubin Transport
Predominantly Albumin 2 binding sites, 1 high
affinity Alpha-Fetoprotein Ligandin liver,
intracellular transport P-Glycoprotein (brain)
and MRP2 export pump in hepatocytes Glutathione-
S-transferases Lipoproteins RBCs
7
Bilirubin Transport
- Bilirubin transported in 4 different forms in
plasma - Unconjugated bilirubin bound to albumin.
- Unconjugated bilirubin unbound. (free)
- Conjugated bilirubin.
- Conjugated bilirubin bound to albumin.
(d-bilirubin)
8
UDP-Glucuronate ß-glucuronosyl Transferase
Bilirubin (insoluble) is glucuronidated in liver
twice Enzyme activity increased with
Phenobarbital, Dexamethasone, Clofibrate, and
Thyroid analogs. Basis for Crigler-Najjar and
Gilbert Syndromes.
9
Defects in UGT
Bilirubin-UGT1A1 isoform main conjugater. Located
in the Endoplasmic Reticulum of
hepatocytes. Crigler-Najjar type I complete
absence of UGT1A1 activity. Phototherapy?Liver
transplantation. Crigler-Najjar type II severe
but incomplete loss of UGT1A1 activity. Enzyme
inducible with phenobarbital. Gilbert Syndrome
mildly decreased UGT1A1 activity. Abnormal
promoter. TA(7) Allelle (Breast Milk
Jaundice)
10
Enterohepatic Circulation
Glucuronidated bilirubin is unstable. Broken
down by ß-glucuronidase in intestinal mucosal.
(also in breast milk) In neonates 1. 10x
increased concentration of ß-glucuronidase. 2.
Alkaline pH of proximal small bowel facilitates
non-enzymatic hydrolysis. 3. Excretion of
monoglucuronidated bilirubin (more rapid
breakdown.) Unconjugated bilirubin is readily
reabsorbed in intestine. Accounts for up to 50
hepatic bilirubin load in neonates. In adults,
bilirubin converted by bacteria in intestine to
urobilinogen and stercobilin (both are
water-soluble).
11
Bilirubin Historical perspective
Neonatal jaundice has been recognized for
centuries First anatomic description of
jaundiced brains by Johannes Orth in
1875. Kernicterus coined in 1904 by Christian
Georg Schmorl after postmortem examination of 120
jaundiced infants brains. 1932 Diamond,
Blackfan and Baty describe Erythroblastosis Fetali
s. 1930-1940 Discovery of Rh antigen. 1940-1950
Use of RBC transfusions?Exchange Transfusions
(Wallerstein) 1952 Association of serum
bilirubin level, Rh disease, and kernicterus
established by David Y.Y. Hsia.
12
Bilirubin Historical Perspective
1950s Kernicterus not restricted to Rh
Disease 1950-60s Increased understanding of
bilirubin metabolism. 1958 Phototherapy for
Jaundice. Sister Jean Ward, Dr. Cremer, and Jerry
Lucey (1968). 1964 Rhogam developed (Freda,
Gorman, and Pollack). 1970s Kernicterus in
Premature Infants. (benzyl alcohol) 1980s
Disappearance of Kernicterus. 1990s
Re-emergence of Kernicterus.
13
Risk Factors for development of
Hyperbilirubinemia
Dennery, PA, et al. NEJM 2001, 344(8)581-90.
14
The Bilirubin Set-up
- Neonates have
- Shortened RBC survival. (approx. 70 days)
- Increased RBC mass.
- Immaturity of hepatic glucuronidation.
- Enhanced enterohepatic circulation.
- Feeding issues Breast feeding, dehydration, etc.
15
Bilirubin 20 mg/dL Vigintiphobia Jon F.
Watchko and Frank A. Oski Pediatrics 1983,
71(4) 660-3
Challenged premise that bilirubin gt 20 mg/dL
requires exchange transfusion. (Data extrapolated
from Rh Disease.) Hsia et al. 1952 Rh disease,
18 infants with bilirubin 16-30 mg/dL and 50
infants with bilirubin gt 30 mg/dL developed
kernicterus.
16
Evaluation of Jaundiced Newborn
Bilirubin level plasma Mother-Baby studies Mom
and infants blood type and direct Coombs. CBC
with smear. Reticulocyte count.
17
Hour-Specific Bilirubin
Healthy, dCoombs neg. N 2840 (13,003) High
Risk (gt 95) TSB gt 8 mg/dL _at_ 24 hrs. TSB gt 14
mg/dL _at_ 48 hrs. TSB gt 17 mg/dL _at_ 84 hrs.
Bhutani, et al. Pediatrics 1999 103(1) 6-14.
18
Treatment
- Nutrition Breast vs. Bottle feeding vs. IV
fluids. - Phototherapy
- Inhibitors of hemoglobin degradation (Tin
Mesoporphyrin). - Stimulators of hepatic UDPG enzyme
(Phenobarbital). - Exchange Transfusion.
- IVIG Rh disease or ABO hemolytic disease.
19
Breast Feeding
Breast Feeding Jaundice first 5 days of
life. Breast Milk Jaundice 4-7 days of life.
(can persist for weeks) Likely Gilbert G6PD
deficiency Average weight loss 6.1 2.5.
5-10 BF infants lose gt 10 Breast fed infants
are 3x more likely to develop TSB gt 12 mg/dL, 6x
more likely to develop level gt 15 mg/dL versus
formula fed. Increasing the frequency of BF
during first several days of life decreases TSB
levels.( at least 8 times/24 hr
period) Supplemental feedings of water or
dextrose-water increase TSB. Interrupt
nursing?...Probably not unless TSB gt 25 mg/dL.
20
Phototherapy
Cremer study 1958. Not used in US until Luceys
study 1968. Factors (from Maisels) Light
source (Spectrum) 480-500 nm best
(blue-green) Blue fluorescent tubes (special)
as close as 10 cm from
baby Halogen risk of burns Fiberoptic
Wallby and BiliBlanket Light-emitting
diodes Dose (Irradiance) Design of
Phototherapy Exposed surface area in
infant Distance of light source from infant
21
Phototherapy
How does it work bilirubin Z,Z Photodegradation
Z-Lumirubin (2-6), more rapid
clearance. Photooxidation (to biliverdin and
others) slow process Photoisomerization
Increased polarity (solubility), does
not require liver conjugation. (20).
Bilirubin Z,E. Reversible process. How
effective Very. Lowers bilirubin by up to 50
first 24 hrs. Side Effects Cell/DNA
damage Photosensitivity Bronze Baby
Syndrome Eye Damage Retina Diarrhea Insensible
water loss/thermoregulation Blunts postprandial
increase in SMA blood flow
22
Tin-Mesoporphyrin
Competitive inhibitor of HO. Allows heme to be
eliminated directly. One dose effective at
preventing extreme hyperbilirubinemia. preventive
dose 1-6 µmol/kg treatment dose 6
µmol/kg Rapidly cleared from plasma but
prolonged half-life. (photosensitivity) Concerns
about heme homeostatic disruption. Currently not
FDA approved
23
Exchange Transfusion
Goals (Watchko in Neonatal Jaundice, 2000.) 1.
Removal of antibody-coated RBCs. 2. Correction
of anemia. 3. Removal of maternal antibody. 4.
Removal of other toxic byproducts of hemolytic
process. 85 infants RBCs removed by
double-volume exchange. (DVE) Majority of
bilirubin is extravascular DVE removes 110
circulating bilirubin (25 total
body) Post-exchange bilirubin levels 60
pre-exchange. 30 min post-exchange, serum bili
70-80 pre-exchange. Perform through UVC.
Duration 1.5 /- 0.5 hrs.
24
Exchange Transfusion
Many complications Hypocalcemia
5 Thrombocytopenia NEC Hypoglycemia Infection
Catheter-related complications Arrhythmias Emb
oli/Thrombosis Altered blood flow Apnea-Bradycar
dia Death 0.3-0.95 per 100 procedures Significa
nt Morbidity 6.7
25
ABO Incompatibility
Mom O and Baby A or B represents ABO
incompatibility. AgtB for antigenicity. Neonates
have fewer A, B antigens compared to adult
RBCs. 15 pregnancies at risk. 1/3 A or B
infants born to O mothers have positive Direct
Coombs. 1/5 with positive Coombs develop modest
to significant degree of hyperbilirubinemia. (TSB
gt 12.8 mg/dL)
26
Coombs Testing
Direct Coombs Recognizes antibodies on fetal
RBCs. Steps 2,3 Indirect Coombs Recognizes
antibodies in maternal serum. Steps 1-3
Blue Maternal Antibodies RBC Neonates
RBCs Green Coombs Reagent
27
Rh Disease
- Risk if mom is Rh neg. and baby is Rh positive.
(15 Caucasians are.) - Major antigen is D. (but other antigens exist)
- Prevent with Rhogam.(10 µg/ml fetal blood or
standard dose is 300 µg) - To develop Rh Disease, need (From Gabbe, 2002)
- The fetus must have Rh-positive erythrocytes, and
the mother must have - Rh-negative erythrocytes.
- 2. A sufficient number of fetal erythrocytes must
gain access to the maternal - circulation. (as little as 0.1 ml fetal blood)
- The mother must have the immunogenic capacity to
produce antibody - directed against the D antigen.
28
Glucose-6 Phosphate Dehydrogenase Deficiency
(G6PD)
X-linked recessive. Most common enzyme defect.
3.4 incidence (up to 20 with specific
populations) Mediterranean, Africa, SE Asia,
Arab. Class 1 severe deficiency, lifelong
hemolysis/anemia Class 2 severe deficiency,
1-10 enzyme activity Class 3 moderate
deficiency, 10-60 enzyme activity Class 4
Normal, 60-150 enzyme activity Class 5
Increased, gt150 enzyme activity Activity of
enzyme declines with increasing age of
RBC. Hemolysis triggered by oxidative
exposure. Increased risk of sepsis (unknown
mechanism)
Bhutani, V. Neoreviews 2012, 13(3)e166-77.
29
G6PD continued
Bhutani, V. Neoreviews 2012, 13(3)e166-77.
30
G6PD cont
- Evaluation
- Qualitative
- Fluorescent Intensity (FST) of NADPH-not
useful - with partial enzyme activity, semi-quantitative
- Quantitative Several methods, preferred
- Specrophotometric assay for NADPH formation
- PCR too many mutations ( 127 identified to
date) but useful confirmation and in females
31
Kernicterus Jaundice of the Nuclei
Bilirubin highly toxic to neurons, particularly
in certain regions of the brain. Toxicity
enhanced by acidosis, infection, respiratory
compromise, dehydration and hyperosmolarity. Regi
ons affected include hippocampus, thalamus,
striatum, auditory and oculomotor
nuclei. Kernicterus has both acute and chronic
components.
32
Bilirubin Neurologic Toxicitiy
Acute Phase (Acute Bilirubin Encephalopathy)
Early Lethargy, hypotonia, poor
suck Intermediate Moderate stupor,
irritability, hypertonia. May have fever,
high-pitched cry, altered MS Advanced
Retrocollis-Opisthotonos, shrill cry, no
feeding, apnea, fever, deep stupor/coma,
seizures, death Chronic Phase
(Kernicterus) a. Deafness/auditory system
dysfunction (high frequency, sensorineural
hearing impairments.) b. Movement disorders
Athetosis, dystonia, hypotonia c. Oculomoter
disturbances particulary upward gaze paresis d.
Dental enamel hypoplasia of deciduous teeth
33
Kernicterus
Medulla
Striatum, Hippocampus
34
Kernicterus
35
MRI and Kernicterus
Axial T2-weighted image
Axial T1-weighted image
Shah, Z et al. Australian Radiology 2003
47(1)55-7.
36
Kernicterus Registry
Created in 1992 by Dr. Audrey.K. Brown and
colleagues. Analyzed through January 1,
2001. Only 1/61 initial patients delivered by
C/S. 59/61 initial patients were breast
fed. Pre-discharge bilirubin level in 26
(16/61). 10/16 level was gt 95 on Hour-Specific
Bilirubin Nomogram. 44/61 (72) did not have
follow-up appointment within 2-3 days. 20.8
subsequently found to have G6PD
Johnson, LH et al. J. Pediatr. 2002
140(4)396-403.
37
Its natural for babies to be sleepy
Most babies are jaundiced
Jaundice gets worse before it gets better.
Dont worry as long as the baby is feeding,
wetting diapers, and stooling.
No need to bring the baby in to see the doctor
Try not to be an overanxious mother
Johnson, LH et al. J. Pediatr. 2002
140(4)396-403.
38
Root Causes in Reappearance of Kernicterus
JCAHO Sentinel Event Alert, April 2001, issue 18
- Patient Assessment
- a. Unreliability of visual assessment of
jaundice in newborns - with dark skin.
- b. Failure to recognize jaundice or severity
based on visual - assessment and measure bilirubin level before
d/c or at f/u. - c. Failure to measure bilirubin level in infant
who is jaundiced - in first 24 hrs. of life.
39
Root Causes in Reappearance of Kernicterus
JCAHO Sentinel Event Alert, April 2001, issue 18
2. Continuum of Care a. Early hospital d/c
(lt48 hrs.) without appropriate f/u (1-2 days
after d/c). Particularly in infants lt 38
wks. b. Failure to provide early f/u with
physical assessment for infants who are
jaundiced before d/c. c. Failure to
provide ongoing lactation support.
40
Root Causes in Reappearance of Kernicterus
JCAHO Sentinel Event Alert, April 2001, issue 18
3. Patient and Family Education a. Failure to
educate parents about jaundice b. Failure to
respond appropriately to parental concerns about
jaundiced newborn, poor feeding, lactation
difficulities or changes in newborn behavior and
activity.
41
Root Causes in Reappearance of Kernicterus
JCAHO Sentinel Event Alert, April 2001, issue 18
4. Treatment a. Failure to recognize, address
or treat rapidly rising bilirubin. b. Failure
to aggressively treat severe hyperbilirubinemia
in a timely fashion with intensive phototherapy
or exchange transfusion.
42
PICK Parents of Infants and Children with
Kernicterus
Founded in 2000 by seven mothers. Organized
workshop on Hyperbilirubinemia/Kernicterus in
2001 attended by CDC, JCAHO, NIH, AAP,
researchers, etc. Worked with JCAHO to issue
Sentinel Event Alert May 2001. Advocated for
classification of kernicterus as Never Event
by National Quality Forum (NQF). Worked with CDC
to issue MMWR on kernicterus on June
2001. Worked to educate multiple organizations
about hyperbilirubinemia and kernicterus. Initiat
ed research on kernicterus.
43
Major Risk Factors for Hyperbilirubinemia in
Full-Term Newborns J aundice within first 24
hours after birth. A sibling who was jaundiced
as a neonate. U nrecognized hemolysis such as
ABO blood type incompatibility or Rh
incompatibility. N onoptimal sucking/nursing. D
eficiency in glucose-6-phosphate dehydrogenase, a
genetic disorder. I nfection. C
ephalohematomas/bruising. E ast Asian or
Mediterranean descent.
MMWR 2001, 50(23) 491-4.
44
July 2004 AAP Guidelines
Management of Hyperbilirubinemia in the
Newborn Infant 35 or More Weeks of Gestation
Pediatrics, 2004 114(1) 297-316.
45
Risk/Protective Factors for Hyperbilirubinemia
46
Phototherapy 2004
47
Exchange Transfusion
48
BilirubinAlbumin Ratio
49
Follow-up Appointments