Inner cell mass - PowerPoint PPT Presentation
1 / 45
Title:
Inner cell mass
Description:
corpus luteum produces progesterone & estrogen to maintain lining of uterus ... Dystocia and prolonged labor. Dystocia = difficult labor. due to fetal position or size ... – PowerPoint PPT presentation
Number of Views:70
Avg rating:3.0/5.0
Title: Inner cell mass
1
(No Transcript)
2
Blastocoele
Becomes amniotic sac
Blastocyst (cross section)
Spermatozoa
Morula
Ovum (cross section)
Cleavage
Inner cell mass
Destined to become fetus
Fertilization
Trophoblast
Secondary oocyte (ovum)
Accomplishes implantation and develops into fetal
portions of placenta
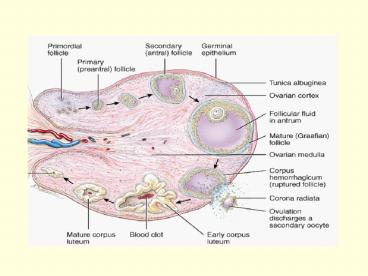
Ovulation
Ovary
Implantation
Endometrium of uterus
3
Surface of uterine lining
Decidua
Inner cell mass
Cords of trophoblastic cells
4
Physiological and hormonal changes in pregnancy
- Chorion
- from day 8 until 4 months secretes hCG which
keeps corpus luteum active - corpus luteum produces progesterone estrogen to
maintain lining of uterus
5
hormonal changes in pregnancy (cont.)
- Placenta
- by 4th month produces enough progesterone
estrogen - relaxin which relaxes tissues of pelvis and cervix
6
- human chorionic somatomammotropoin (hCS) or human
placental lactogen (hPL) - helps prepare mammary glands for lactation
7
- corticotropin-releasing hormone (CRH) increases
secretion of fetal cortisol (lung maturation)
acts to establish timing of birth
8
Hormonal Secretion by the Placenta
9
Hormone Blood Levels
- Human chorionic gonadotropin (hCG) produced by
the chorion is less important after 4 months,
because the placenta takes over the hormonal
secretion of the corpus luteum.
10
Response of the mothers body to Pregnancy
- Weight gain
- Metabolism
- Digestive System and nutrition
11
Response continued
- Cardiovascular System
- blood volume 30 above normal
- increased cardiac output, heart rate and blood
pressure - Cardiovascular changes to meet needs of fetus
- Respiratory System
- diaphragm is raised
- movement is restricted
- rate is increased
- increase in tidal volume 30
12
Response
- Urinary System
- Increased glomerular filtration rate
- increased urine formation
13
Labor and Parturition
- Parturition means giving birth labor is the
process of expelling the fetus - progesterone inhibits uterine contraction
14
- Labor begins when progesterones inhibition is
overcome by an increase in the levels of estrogen
15
Figure 20.27Page 791
Human chorionic gonadotropin (hCG)
Estrogen
Progesterone
Fertilization
Delivery
16
Why estrogen level is increased?
- placenta stimulates fetal anterior pituitary
which causes fetal adrenal gland to secrete DHEA - placenta converts DHEA to estrogen
- estrogen overcomes progesterone and labor begins
17
- Hormonal Factors That Cause Increased Uterine
- Contraction
- Ratio of Estrogens to progesterone
- from 7th month onward estrogen secretions
- increased (progesterone remains constant)
- Effect of oxytocin on the uterus
- Effect of Fetal Hormones on the Uterus
18
- Mechanical Factors That Increase the
Contractility - of the Uterus
- Stretch of the uterus
- Stretch of the cervix
- A positive feedback Theory
19
Positive Feedback during Labor
- Uterine contraction forces fetal head into cervix
(stretch) - Nerve impulses reach hypothalamus causing release
of oxytocin
20
- Oxytocin causes more contractions producing more
stretch of cervix more nerve impulses
21
The blue arrows designate the sequence of events
leading to the onset of parturition. The green
arrows designate the positive-feedback
cycle responsible for the progression of
parturition.
Uterine contractions
Push fetus against cervix
Responsible for progression of parturition
(through neuroendocrine reflex)
Prostaglandin production
Oxytocin secretion
22
True Versus False Labor
- True labor begins when contractions occur at
regular intervals - produces pain
- back pain increases with walking
- dilation of cervix with a discharge of
blood-containing mucus in the cervical canal
23
- False labor produces pain at irregular intervals
but there is no cervical dilation
24
3 stages of labor
- Stage of dilation
- 6-12 hours
- from onset of labor to the complete dilation of
the cervix - rupture of amniotic sac
25
Placenta
Umbilical cord
Partially dilated cervix
Uterus
First stage of labor Cervical dilation
Second stage of labor Delivery of the baby
Third stage of labor Delivery of the placenta
26
- Stage of expulsion
- from complete cervical dilation to delivery of
the bacy - 10 minutes to hours
27
- Placental stage
- 5 30 minutes
28
Obstetrical Complications
- Ante-partum
- Intra-partum
- Post-partum
29
Ante-partum complications
- Pregnancy induced hypertension PET
(pre-eclamptic toxemia) Toxemia of pregnancy - Dysfunctional labor patterns
30
contd.
- Abnormal placenta position
- Placenta previa
- Abruptio placenta
31
Pregnancy-Induced Hypertension
- Elevated blood pressure
- Preeclampsia (PET)
- sudden hypertension
- large amounts of protein in the urine
- generalized edema, blurred vision headaches
- Eclampsia convulsions coma in mother
32
Dysfunctional Labor Patterns
- Contraction insufficient to produce dilation and
effacement - fetal malposition
- excessive analgesia
- fetal post maturity
- increased maternal age
33
contd.
- Premature rupture of the membranes
- increased maternal age
- cervical damage from surgical instrumentation
34
Abnormalities of the placenta
- Placenta previa
- placenta implantation at the lower segment of the
uterus - obstructing the descent of the babys head
- presented with antepartum hemorrhage
35
contd.
- Abruptio placentae
- premature separation of the placenta
- bleeding may be concealed or revealed
36
Intra-partum complications
- Dystocia and prolonged labor
- Dystocia difficult labor
- due to fetal position or size
- breech presentation is butt or feet first in
birth canal
37
contd.
- Prolonged labor - ? considerCesarean section
(C-section) - horizontal incision through lower abdominal wall
and uterus
38
Post-partum complications
- Retained placenta due to abnormal implantation of
placenta (placenta accreta) - Post partum hemorrhage
39
- Puerperium 6 week period following the birth of
a baby - Physiological changes
- uterus involution
- menstruation resume by 9-12 weeks post partum in
70 of women (not lactating) - weight loss to prepregnancy weight (6 weeks to 6
months)
40
- Most common complications
- Urinary tract infection
- Thromboembolism
- Depression fourth day baby blues
41
Physiology of Lactation
- Lactation production release of milk
- After delivery, progesterone levels drop
suckling increases the release of prolactin
oxytocin (milk ejection reflex)
42
- Colostrum cloudy fluid released for few days
- True milk produced by 4th day
43
Benefits of Breast-feeding
- Faster better absorption of the right
nutrients - Beneficial cells
- functional white blood cells
- neutrophils help ingest bacteria in babys gut
- macrophages produce lysozymes
- plasma cells provides antibodies prevent
gastroenteritis
44
contd.
- Decreased incidence of diseases later in life
- reduction in allergies, respiratory GI
infections, ear infections diarrhea - Parent-child bonding
45
Complications of breast feeding
- puerperal mastitis
- lactation failure due to infrequent suckling