Renal system (physical assessment) - PowerPoint PPT Presentation
Title:
Renal system (physical assessment)
Description:
Renal system (physical assessment) Inspection: Skin- pallor, yellow-gray, excoriations, changes in turgor, bruises, texture(e.g. rough, dry skin) – PowerPoint PPT presentation
Number of Views:1921
Avg rating:3.0/5.0
Title: Renal system (physical assessment)
1
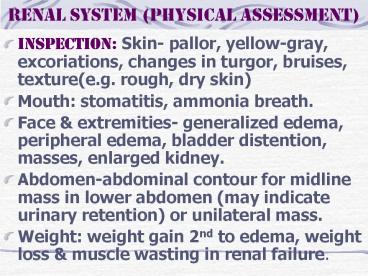
Renal system (physical assessment)
- Inspection Skin- pallor, yellow-gray,
excoriations, changes in turgor, bruises,
texture(e.g. rough, dry skin) - Mouth stomatitis, ammonia breath.
- Face extremities- generalized edema, peripheral
edema, bladder distention, masses, enlarged
kidney. - Abdomen-abdominal contour for midline mass in
lower abdomen (may indicate urinary retention) or
unilateral mass. - Weight weight gain 2nd to edema, weight loss
muscle wasting in renal failure.
2
Renal system (physical assessment)
- General state of health- fatigue, lethargy,
diminished alertness. - Palpation- No costovertebral angle tenderness,
nonpalpable kidney bladder, no palpable masses. - Percussion Tenderness in the flank may be
detected by fist percussion. If CVA tenderness
pain are present, indicate a kidney infection or
polycystic kidney disease. - Auscultation The abdominal aorta renal
arteries are auscultated for a bruit, which
indicates impaired blood flow to the
kidneys
3
Renal Systems (Diagnostic test)
- Urinalysis- evaluation of the renal system for
determining renal disease. - Wash perineal area use a clean container.
- Obtain 10 to 15 mL of the 1st AM sample
- If the client is menstruating, indicate this on
the lab. requisition form. - Specific Gravity-measures the kidneys ability to
concentrate urine. Measured by multiple-test
dipstick (most common method), refractometer-instr
ument used in the lab, urinometer (least accurate
method). Cold specimens produce a false high
reading. Factors that interfere with an accurate
reading include radiopaque contrast agents,
glucose proteins.
4
Renal Systems (Diagnostic test)
- A decrease in SG (less conc. urine) occurs with
increased fluid intake, diuretic administration,
diabetes insipidus. - An increase SG (more conc. Urine) occurs with
insufficient fluid intake, decreased renal
perfusion, or the presence of ADH. - Urine Culture Sensitivity- identifies the
presence of microorganisms determines the
specific abx. that will treat the existing
microorganisms. Note that urine from a client who
forced fluids may be too dilute to provide a
positive culture.
5
Renal Systems (Diagnostic test)
- Creatinine clearance test- A blood timed urine
specimen that evaluates kidney function. - Blood is drawn at the start of the test the AM
of the day that the 24-hour urine specimen
collection is complete. Maintain the urine
specimen on ice or refrigerate. If the client is
taking steroids, check with MD regarding the
administration of these medications during test.
Encourage adequate fluids before during the
test.
6
Renal Systems (Diagnostic test)
- Vanillymandelic acid (VMA)- to diagnose
pheochromocytoma, a tumor of the adrenal gland.
The test identifies an assay of urinary
catecholamines in the urine. Instruct to avoid
foods such as caffeine, cocoa, cheese, gelatin at
least 2 days prior to beginning of the collection
during collection. Save all urine on ice or
refrigerate. Instruct to avoid stress to
maintain adequate food fluids during the test.
7
Renal Systems (Diagnostic test)
- Uric acid- A 24-hour collection to diagnose gout
kidney disease. - Encourage fluids a regular diet during testing.
Place the specimen on ice or refrigerate. - KUB (Kidney, ureters, bladder) radiograph-An
x-ray film that views the urinary system
adjacent structures used to detect urinary
calculi. - Bladder ultrasonography-A noninvasive method of
measuring the volume of urine in the bladder.
8
Renal Systems (Diagnostic test)
- Computed tomography (CT) MRI- provide
cross-sectional views of the kidney urinary
tract. - Intravenous pyelogram (IVP)- the injection of a
radiopaque dye that outlines the renal system.
Performed to identify abnormalities in the
system. Withhold food fluids after midnight
before the test. Inform the client abt. Possible
throat irritation, flushing of the face, warmth
or salty taste that may experienced during the
test.
9
Renal Systems (Diagnostic test)
- Renal angiography- the injection of a radiopaque
dye through a catheter for examination of the
renal arterial supply. Assess the client for
allergies to iodine, seafood radiopaque dyes.
Inform about possible burning feeling of heat
along the vessel when the dye is injected. - NPO after MN on the night of the test. Instruct
to void immediately before the procedure.
Inspect the color temperature of the involved
extremities. Inspect site for bleeding.
10
Renal Systems (Diagnostic test)
- Renal Scan- An IV injection of a radiopaque for
visual imaging of renal blood flow. Instruct that
imaging may be repeated at various interval
before the test is complete. Assess for signs of
delayed allergic reactions, such as itching
hives. - Cystometrogram (CMG)- A graphic recording of the
pressures exerted at varying phases of the
bladder. Inform of the voiding requirements
during after the procedure.
11
Renal Systems (Diagnostic test)
- Cystoscopy Biopsy- the bladder mucosa is
examined for inflammation, calculi or tumors by
means of a cystoscope, a biopsy may be obtained.
NPO after MN before the test. Monitor for
postural hypotension. Note that pink-tinged or
tea-colored urine is common. Monitor for bright,
red or clots notify MD. - Renal biopsy- insertion of a needle into the
kidney to obtain a sample of tissue for exam. NPO
after MN. Provide pressure to the biopsy site for
30 minutes. Check site for bleeding. Force fluids
to 1500-2000 mL. Instruct to avoid heavy lifting
strenuous activity for 2 weeks.
12
Urinary Tract Infection (UTI)
- Inflammation of the bladder from infection or
obstruction of the urethra. - The most common causative organism are E. coli,
Enterobacter, pseudomonas, serratia. - More common in women because they have shorter
urethra than men, the location of the urethra
in women is close to the rectum. - Sexually active pregnant women are most
vulnerable to UTI.
13
Urinary Tract Infection (UTI)
- Causes Allergens or irritants, such as soaps,
sprays, bubbles bath - Bladder distention, calculus, hormonal changes
influencing alterations in vaginal flora. - Indwelling urethral catheter, loss of bacterial
properties of prostatic secretions in the male - Sexual intercourse, urinary stasis, use of
spermicides, wet bathing suits
14
Urinary Tract Infection (UTI)
- Assessment Frequency urgency, burning on
urination, voiding in small amount, inability to
void, incomplete emptying of the bladder, lower
abdominal discomfort or back discomfort, cloudy,
dark, foul smelling urine, hematuria, bladder
spasms, malaise, chills, fever, nausea
vomiting. - Implementation Obtain urine C/S to identify
bacterial growth. Instruct to force fluids up to
3000 mL a day. Provide meticulous perineal care
with an indwelling catheter. Instruct to avoid
alcohol. Provide heat to abdomen or sitz bath for
complaints of discomfort
15
Urinary Tract Infection (UTI)
- Nursing Diagnosis Acute pain r/t inflammation of
mucosal tissue of UT as manifested by pain on
urination, flank pain, bladder spasms. - Provide relief by administering analgesics such
as Pyridium or combination agents (Urised). Alert
that urine color will be orange blue or green
with combination agents. - Teach the use of nonpharmacologic technique-
heating pad, warm showers.
16
Urinary Tract Infection (UTI)
- Impaired urinary elimination r/t UTI as
manifested by bothersome urgency, hematuria or
concern over altered elimination pattern - Obtain midstream voided specimen for C/S.
- Administer antimicrobial drugs.
- Teach signs symptoms of UTI.
- Encourage adequate fluid to help prevent
infection and dehydration.
17
Urolithiasis
- Formation of urinary stones urinary calculi
formed in the ureters. - When a calculus occludes the ureter blocks the
flow of urine, the ureter dilates, producing a
condition known as hydroureter. - If the obstruction is not removed, urinary stasis
results in infection, impairment of renal
function on the side of the blockage, resultant
hydronephrosis irreversible kidney damage.
18
Urolithiasis
- Causes Family history of stone formation
- Diet high in CA, vitamin D, milk, protein,
purines - Obstruction urinary stasis
- Dehydration
- Use of diuretics, which can cause volume
depletion - Immobilization
- Hypercalcemia, hyperparathyroidism
- Elevated uric acid, such as gout
19
Urolithiasis
- Nursing Assessment Nausea, vomiting, dietary
intake of purines, phosphates, low fluid intake
chills. - Elimination Decreased u/o, urinary urgency,
feeling of bladder fullness. - General Acute, severe colicky pain in flank,
back, abdomen groin or genitalia burning
sensation on urination, dysuria,anxiety. - Skin warm, flushed skin or pallor with cool.
- Urinary tenderness on palpation on renal areas,
passage of stone(s). - Increased BUN creatinine WBC, calcium,
phosphorus, uric acid. - KUB- calculi or anatomic changes on IVP
20
Urolithiasis
- Implementation Force fluids up to 3000 mL/day,
unless contraindicated-to facilitate the passage
of the stone prevent infection. - Strain all urine for the presence of stones.
- Turn and reposition immobilized clients.
- Administer analgesics response to pain.
- Instruct in the diet specific to the stone
composition.
21
Urolithiasis
- Surgical therapy
- Nephrolithomy- incision into the kidney to remove
the stone. - Pyelolithotomy- incision into the renal pelvis to
remove the stone. - Ureterolithotomy-removal of stone in the ureter.
- Cystotomy- indicated for bladder calculi.
- Lithotripsy- procedure used to eliminate calculi
in the kidney. Hematuria is common after the
procedure. A stent is often placed after the
procedure to promote passage and to prevent
obstruction, then removed 1 to 2 weeks after
lithotripsy.
22
Urinary Tract Infection (UTI)
- Teaching teach good perineal care to wipe from
front to back. - Instruct to void every 2 to 3 hours.
- Instruct to void drink a glass of water after
intercourse. - Encourage menopausal women to use estrogen
vaginal creams to restore pH. - Instruct the female to use water- soluble
lubricants for coitus, especially after menopause.
23
Polycystic Kidney Disease
- A cystic formation and hypertrophy of the kidney,
which lead to cystic rupture, infection,
formation of scar tissue and damaged nephrons. - The ultimate results of this disease is renal
failure. - Types Infantile inherited autosomal recessive
trait that results in the death of the infants
within few month after birth. - Adult dominant trait results in end-stage renal
disease.
24
Polycystic Kidney Disease
- Assessment Flank lumbar pain or abdominal pain,
fever, chills, UTIs, hematuria, proteinuria,
pyuria HTN, palpable abdominal masses enlarged
kidney. - Implementation
- Monitor for gross hematuria which indicates cyst
rupture. - Increase sodium water loss intake because
sodium loss rather than retentions. - Provide bed rest if cyst ruptured bleeding
occurs
25
Polycystic Kidney Disease
- Implementation Prepare for percutaneous cyst
puncture for relief of obstruction or draining an
abscess. - Prepare client for dialysis and encourage genetic
counseling.
26
Renal Tumors
- May be benign or malignant Common sites of
metastasis include bone, lungs, liver, spleen or
other kidney. - Assessment Dull flank pain, palpable renal mass,
painless hematuria. Unknown cause. - Treatment Radical nephrectomy Removal of the
entire kidney, adjacent adrenal gland renal
artery vein. - Radiation therapy chemotherapy.
27
(No Transcript)
28
Renal Tumors
- Implementation Monitor abdomen for distention
caused by bleeding - Observe bed linens under the client for bleeding
- Monitor for hypotension, decreases in urinary
output alterations in LOC, indicating
hemorrhage. - Monitor urinary ouput
- Do not irrigate or manipulate the nephrostomy
tube if in place.
29
Nephrotic Syndrome
- Arising from protein wasting 2nd to diffuse
glomerular damage. - Assessment Proteinuria, edema, anemia,, malaise,
irritability, HTN, waxy pallor of the skin,
amenorrhea or abnormal menses. - Implementation Monitor I/O. Bedrest if edema
present, monitor daily weights. - Administer plasma expanders, to raise the osmotic
pressure.
30
Nephrosclerosis
- Sclerosis of the small arteries arterioles of
the kidney. There is decreased blood flow, which
results in patchy necrosis of the renal
parenchyma. - Benign occurs in adults 30 to 50 yrs. of age. It
is caused by vascular changes resulting from
hypertension and from atherosclerosis process. - Malignant-complication of HTN,characterized by
sharp increase in BP with a diastolic pressure
greater than 130 mm Hg. - Treatment- aggressive antihypertensive therapy.
The prognosis is poor.
31
Phases of ARF
- Oliguric phase GFR decrease,hyperkalemia, fluid
overload, elevated BUN creatinine. - Diuretic phase GFR Begins to increase,
hypokalemia, hypovolemia, gradual decline in BUN,
creatinine. - Recovery phase BUN is stable normal, complete
recovery may take 1 to 2 years.
32
Stages of Chronic RF
- Stage 1 Diminished renal reserve-renal function
is reduced, no accumulation of metabolic wastes,
nocturia polyuria occurs as a result of
decreased ability to concentrate urine. - Stage 11 Renal Insufficiency metabolic waste
begin to accumulate, oliguria edema occur as a
result of decreased responsiveness to diuretics. - Stage 111 excessive accumulation of metabolic
waste. Kidney are unable to maintain homeostasis.
Dialysis is required.
33
Kidney Transplant
- Implantation of a human kidney from a compatible
donor into a recipient. - Performed for irreversible kidney failure.
- Immunosuppressive medications must be taken for
life. - Complications Graft rejection- fever, malaise,
elevated WBC, graft tenderness, signs of
deteriorating renal function, acute HTN, anemia.
Occurs immediately after surgery to 48
hours-removal of rejected kidney.
34
Kidney Transplant
- Avoid prolonged period of setting
- Recognize the signs symptoms of infection
rejection. - Avoid contact sports
- Use medications maintained immunosuppressive
therapy for life.
35
(No Transcript)