RETINAL VEIN OCCLUSION - PowerPoint PPT Presentation
Title:
RETINAL VEIN OCCLUSION
Description:
RETINAL VEIN OCCLUSION Epidemiology 51% 65y 10-15% – PowerPoint PPT presentation
Number of Views:353
Avg rating:3.0/5.0
Title: RETINAL VEIN OCCLUSION
1
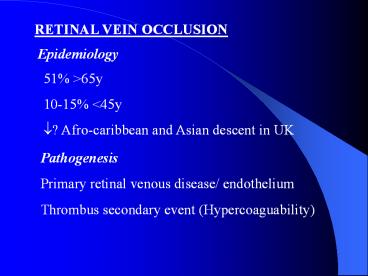
RETINAL VEIN OCCLUSION
Epidemiology
51 gt65y 10-15 lt45y ?? Afro-caribbean and Asian
descent in UK
Pathogenesis Primary retinal venous disease/
endothelium Thrombus secondary event
(Hypercoaguability)
2
AETIOLOGICAL CONDITIONS
COMMON SYSTEMIC LOCAL
1. BP Glaucoma
2.Hyperlipidemia Trauma
3.DM Orbital lesions
4.Smoking Oedema-drusen optic disc
RARER 1.MM and Waldestrom 6.Secondary causes of 1, 2, 3 such as acromegaly cushing, hypothyroidism
2.CRF 6.Secondary causes of 1, 2, 3 such as acromegaly cushing, hypothyroidism
3.Vasculitis 6.Secondary causes of 1, 2, 3 such as acromegaly cushing, hypothyroidism
4.Thrombotic disorders 6.Secondary causes of 1, 2, 3 such as acromegaly cushing, hypothyroidism
5. Oral contraceptives (oestrogen)/ no HRT 6.Secondary causes of 1, 2, 3 such as acromegaly cushing, hypothyroidism
3
DIAGNOSIS
- Painless loss of vision- unilateral
- Asymptomatic
4
BRVO
Arteriovenous crossings Macular branch (DD from
diabetic maculopathy)
ACUTE CHRONIC
Haemorrhages Venous sheathing
Retinal oedema Exudates
Cotton wool spots Collaterals
Tortuous veins CMO
gt5 dd non-perfusion NVE
5
CRVO
ACUTE CHRONIC
Dilated tortuous retinal veins Swollen optic disc Intraretinal haemorrhage Cotton wool spots Retinal oedema Sheathing of veins Absorption of haemorrhage Disc collaterals Macular oedema
6
MECHANISMS OF VISUAL LOSS
Ischaemic (direct- indirect) Exudative (macular
oedema)
30 non-isch. Convert to ischaemic type first 4/12
Eyes at High Risc for Ischaemic Complications
1.RAPD 2. ??? VA 3. FFA gt10DD, 5-10 DD 4.Cotton
wool spots gt10, 5-10 5. Deep dark haem.
(infarct) 6. Elderly ( rubeosis)
7
DIFFERENTIAL DIAGNOSIS
1.Accelerated hypertension 2.DM 3.Slow-flow
retinopathy 4.Peripapillary telangiectasia 5.
AION 6.Lupus/ radiation retinopathy 7. CMV
retinitis 8.Ocular ischaemic syndrome
8
MEDICAL INVESTIGATIONS
ALL PATIENTS FBC, ESR, UE, LFT, GLC, Lipid
profile Protein electrophoresis ECG TFT MORE
SPECIALISED CXR Cardiolipin, Lupus
anticoagulant CRP, ACE, FTA-ABS RF, ANA, DNA,
ANCA MRI orbit, brain
9
MANAGEMENT OCULAR
BRVO Argon laser for macular oedema if foveal
vasculature intact (FFA), VA 6/12-6/60 3-6/12
after the initial event Sectoral PRP for
proliferative complications or if areas of
non-perfusion gt5DD FU 6/52, up to 2years after
(collaterals)
10
CRVO Prevention of neovascularisation Grid no
benefit FFA and Laser haemorrhages sufficiently
resolved Monthly FU/ total of 2years gt40DD
PRP 10-40DD no lt10 (non-ischaemic)
no Non-ischaemic cases convert to ischaemic 13
6/12 18 18/12 CHECK RAPD ALWAYS IN FU
11
- MEDICAL
- Maximise visual outcome
- ? cardiovascular morbidity/ mortality (risk
factors) - Prevent recurrence to other eye (15 over 5
years) Aspirin/ dipyridamole