RETINAL VEIN OCCLUSION - PowerPoint PPT Presentation
Title:
RETINAL VEIN OCCLUSION
Description:
Neovascularisation scatter laser CRVO Ischemic Non-ischemic CRVO Ischemic Non-ischemic Non-ischemic CRVO (Course and Follow-up) Residual signs: Disc ... – PowerPoint PPT presentation
Number of Views:2164
Avg rating:3.0/5.0
Title: RETINAL VEIN OCCLUSION
1
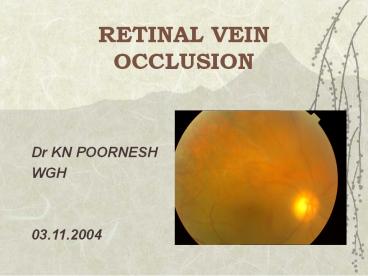
RETINAL VEIN OCCLUSION
- Dr KN POORNESH
- WGH
- 03.11.2004
2
CLASSIFICATION
- BRVO CRVO
- Major BRVO Non-ischemic
- Minor Macular BRVO Ischemic
- Peripheral BRVO
Papillophlebitis - Hemiretinal Vein occlusion
3
PATHOGENESIS
- Arteriosclerosis
- ?
- Compression of the vein
- ?
- Venous endothelial cell loss
- Thrombus formation
- Venous Occlusion
4
PATHOGENESIS
- Venous occlusion ? elevation of
venous -
capillary pressure -
? - ? ? ? Stagnation
of blood flow - ?
? - Increased tissue pressure Hypoxia of the
retina - ?
? - Damage to capillary endothelial
cells - extravasation of blood
constituents
5
RISK FACTORS(in order of importance)
- Advancing age 50 cases over 65 yrs.
- Systemic HT, Hyperlipidemia, Diabetes, Smoking,
Obesity. - Raised IOP risk of CRVO
- Inflammatory Behcets, Sarcoid,AIDS, SLE,
Toxoplasma. - Hyperviscosity Polycythemia, MM, Waldenstrom
macroglobulinemia.
6
RISK FACTORS
- 6. Acquired thrombophilic Hyperhomocystinemia,
Antiphospholipid antibody syndrome. - 7. Inherited thrombophilic increased levels of
clotting factors 7 11, deficiency of
antithrombin 3, protein C S, resistance to
activated protein C. - Other Risk factors
- Hypermetropia (BRVO), Congenital anomaly of
Central retinal vein (CRVO), Optic disc drusen,
- Drugs (OC, Diuretics), Migraine (rare).
- Retrobulbar external compression
Dysthyroid eye disease, Orbital tumor
7
Major BRVO
8
COURSE of BRVO
- 6 to 12 months to resolve
- Venous sheathing
- Collateral venous channels
- Microaneurysms, Hard exudates,
Cholesterol crystal deposition. - Macula RPE changes or
- ER gliosis, chronic CME.
9
(No Transcript)
10
(No Transcript)
11
(No Transcript)
12
Prognosis and Complications of BRVO
- Depends on Site Size of occluded vein
Integrity of perifoveal
capillary network - 50 Recover VA of 6/12 or better.
- Complications 1. Chronic macular edema
- 2. Macular ischemia
- 3.
Neovascularisation, - NV (within 3
yrs) - 10- NVD, 20-30-
NVE - 4. Recurrent VH, TRD.
13
(No Transcript)
14
(No Transcript)
15
(No Transcript)
16
Management of BRVO(BVOS)
- Wait for haemorrhage to clear (3 months).
- FFA
- Macular edema and VA 6/12 or worse after 3
months grid laser follow-up after 2-3 months. - Macular ischemiano treatment.
- 5 DD or gt area of CNP 4 monthly follow- up for
12-24 months. - Neovascularisation scatter laser
17
(No Transcript)
18
CRVO Ischemic Non-ischemic
Frequency 25 75
VA 20/400 or lt (90) gt than 20/400 (90)
Site at lamina cribrosa Far behind lam crib
RAPD marked slight
VF defect common rare
Fundus Ext hgs cotton wool spots, severe disc edema, marked tortuosity of vessels Less exten hgs, few cotton wool spots, mild disc edema, variable tortuosity of vessels
19
CRVO Ischemic Non-ischemic
FFA Wide spread capillary non- perfusion Delayed venous return, late leakage, good perfusion.
ERG Reduced b wave amplitude, reduced b/a ratio normal
Prognosis 50 develop rubeosis NVG in 2-4 months 3 develop rubeosis and NVG. 50 return to VA 6/12 or better.
20
(No Transcript)
21
(No Transcript)
22
(No Transcript)
23
Non-ischemic CRVO(Course and Follow-up)
- Residual signs Disc collaterals, epiretinal
gliosis, pigmentary changes at macula. - Conversion to ischemic CRVO occurs in 15 of
cases within 4 months and 34 within 3 years. - Follow-up should be for 3 years.
- Prognosis depends on initial VA, near normal VA
in 50, Chronic CMO- unresponsive to laser
(CVOS). - 8-10 risk of BRVO or CRVO in the fellow eye.
24
Ischemic CRVOManagement (CVOS)
- Follow-up monthly for 6 months
- ?IOP, undilated gonioscopy SLE
- Angle NV is the best clinical predictor of NVG.
- Treatment PRP in eyes with angle or iris NV.
Monthly follow-up until stabilisation or
regression.
25
Hemiretinal vein occlusion
- Less common than BRVO and CRVO
- Occlusion of superior or inferior branch of the
CRV. - Features of BRVO, involving the superior or
inferior hemisphere - Prognosis depends on severity of macular edema
and ischemia.
26
PAPILLOPHLEBITIS(Optic disc vasculitis)
- Healthy individuals, lt 50 years
- Optic disc swelling with secondary venous
congestion rather than venous thrombosis. - APD absent, retinal haemorrhages confined to
posterior fundus. - Prognosis 80 -- 6/12 or better
- 20 visual loss -- macular edema
27
ManagementRecent advances
- Recent onset of non-ischemic CRVO high intensity
laser to create chorioretinal shunt. - AV sheathotomy for treatment of CME due to BRVO.
- Ischemic CRVO- PP Vitrectomy Intraocular gas
Radial neurotomy
28
Management Recent advances
- Intravitreal tPA
- Transvitreal vein cannulation
- Section of posterior scleral ring
- Drug therapy -- Troxerutin
- -- Petroxyfylline
- -- Hemodilution
- Intravitreal Triamcinolone
29
Thank You