Disease - PowerPoint PPT Presentation
1 / 56
Title: Disease
1
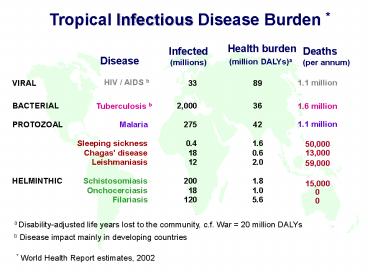
Tropical Infectious Disease Burden
Health burden (million DALYs)a
Infected (millions)
Deaths (per annum)
Disease
HIV / AIDS b
1.1 million
VIRAL
BACTERIAL
1.6 million
Tuberculosis b
1.1 million
PROTOZOAL
Malaria
Sleeping sickness
50,000
Chagas' disease
13,000
Leishmaniasis
59,000
HELMINTHIC
Schistosomiasis
15,000
Onchocerciasis
0
Filariasis
0
a Disability-adjusted life years lost to the
community, c.f. War 20 million DALYs
b Disease impact mainly in developing countries
World Health Report estimates, 2002
2
Common human parasitic diseases in the USA
3
The Continuing Crisis in Drug Discovery
Development
Cerebral malaria
- Only 13 new drugs for all tropical diseases from
1975-2005 - Pharmaceutical companies discontinuing
- research in all infectious diseases
- Low economic return
- High cost (800 million)
- Poor success rate
4
Tools for Disease Control
Diagnostics, Drugs, Vaccines detect,
eliminate prevent infection
Chemical, biological and physical control methods
reduce transmission
Parasite
Vector
Host
Public health and education increase health
awareness, reduce exposure, increase compliance,
etc.
5
Why Do We Need New Drugs?
- Control of insect vectors inadequate
- No vaccines available yet
Anopheles gambiae
- Current drugs are unsatisfactory
SPf66 vaccine trial
- Drug resistance
- Side effects
- Poor efficacy
- High cost
- Route of administration
- Availability
Incidence of resistance to common antimalarial
drugs
6
Compound Success Rate by Stages
Discovery
Target validation and lead discovery
(gt104 compounds)
Preclinical
Laboratory and animal testing
(250 lead compounds)
Phase I
Safety and dosage (20-80 healthy volunteers)
(5 drug candidates)
Phase II
Efficacy and side effects (100-300 patient
volunteers)
Success 1 in 5,000
Phase III
Adverse reactions (1000-5000 patients)
Approval
(1 drug)
Post marketing surveillance
6 years
6 years
2 years
5-10 years
Preclinical
Clinical
Approval
Withdrawal
Cost gt800m
Source Pharmaceutical Industry Profile 2001
7
The Ideal Product Profile
Safe for use (men, women, children and
foetus) Minimal toxicity (tolerable side
effects) Few contraindications (drug-drug
interactions HIV or TB co-infections) Efficacious
(treatment lt 14 days 3 days malaria)
Resistance (low resistance potential) Orally
active (avoid needles and hospitalization) Broad
spectrum (all disease species, including
resistant lines) Stable (2 years shelf life at 40
?C and 75 relative humidity) Affordable
(diseases of the poor 1 per patient, malaria)
8
Lead Discovery Target Validation Chemical
Genomics
Parasite
Mammalian cell
Whole cell screens with chemical libraries /
natural products (selectivity/druggability)
Unknown potential targets cellular poisons
Mode of action studies (target identification)
Potential druggable targets
Genetic validation (essentiality)
Validated druggable targets lead
(added value)
9
Target Selection, Validation and Lead Discovery
Genomic Approach
Metabolome
Genome
Proteome
Transcriptome
(target identification)
Comparative genomics metabolomics
Comparative biochemistry molecular biology
Potential targets
Genetic validation (essentiality)
Validated targets
Chemical validation (selectivity/druggability)
Druggable targets Lead
(added value)
10
Criteria for Target Selection
- Essential for survival in appropriate life cycle
stage - Generally not molecules involved in
virulence or invasion - Absent, significantly different or non-essential
to host - Examples trypanothione, Type II Fab, DHFR-TS,
ODC - Selective inhibition possible with drug-like
molecules - Avoid enzyme co-factors and
phosphorylated substrates - Easy to isolate, overproduce and assay
- Ideally soluble recombinant enzyme,
with known structure and chemical
mechanism. Generally not multi-component,
membrane or structural proteins - Assay modifiable for HTS format
- Ideally mix and measure methods. Avoid
separation methods / radioisotopes
11
Discovery Research Drug Discovery Needs
Target identification - bioinformatics chemical
genomics Target validation - inducible
(conditional) gene knockout and RNAi /
antisense Target characterization - function,
mechanism and structure Compound evaluation -
reporter systems for screening in vitro and in
vivo Assay development - high throughput
screening (identify lead compounds) Mechanistic
studies - modes of drug action and drug
resistance mechanisms Molecular diagnostics -
prediction of therapeutic efficacy and drug
toxicity, especially non-invasive methods
Target ID validation
Assay Dev. and HTS
Lead Identification
Lead Optimisation
Preclinical Development
Phase I
Ph. II
lt Discovery Research gt
12
Treatment of helminth infections
Adult worms do not multiply in the mammalian
host. The most effective chemotherapeutic
targets have been Motility Energy Metabolism
1. Drugs affecting motility a. Worms have
complex nervous systems b. Active motility is
essential for the worms to resist expulsion by
bowel peristalsis
2. Drugs affecting energy generation or metabolic
pathways a. Enteric helminths exist in an
anaerobic environment, and have developed
special mechanisms for generating energy.
13
1. Drugs affecting motility
14
Praziquantel This drug has modernized the
treatment of cestode and trematode infections. It
appears to cause tetanic contraction of
schistosomes by altering calcium transport and
membrane integrity
Avermectins These drugs act by increasing the
Cl- permeability of nerve andmuscle membrane of
invertebrates acting ona glutamate-gated Cl-
channel. They cannotpass the blood-brain
barrier, therefore, they have little toxicity.
They are extremely potent against nematodes,
ectoparasites, and insects.
15
Simplified schematic representation of the
invertebrate and vertebrate chloride ion channels
under avermectin control
16
2. Drugs affecting energy generation
or metabolism
Pyrvinium pamoate
Mebendazole
(Oxidative phosphorylation)
Diethylcarbamazine
Niclosamide
Thiabendazole
(Affect microtubules)
(Arachidonic acid metabolism)
(oxidative phosphorylation)
17
Cysticercosis treatment
- Treatment should be individualized based on cyst
location, level of inflammation and clinical
presentation - Therapy should include analgesics, antiepileptic
drugs, cysticidal drugs, surgical resection of
lesions and placement of ventricular shunts - Parenchymal cysticercosis with viable cysts
Albendazole 15 (mg/kg/day) with dexamethasone
(0.1 mg/kg/day). Praziquantel. - Subarachnoid ccs antiparasitic therapy
- No reason to use antiparasitic drugs to treat
dead calcified cysts. Symptomatic therapy. - Surgical therapy ventricular shunting to
resolve hydrocephalus. Also excision of giant
cysts or intraventricular cysts
Albendazole
18
Treatment of schistosomiasis
Praziquantel Oxamniquine
Structure Isoquinilone Tetrahydroquinilone
Active against All Species
S. mansoni Dosage 40-60mg/kg
15-40mg/kg Single
dose 1-2 doses Cure Rate
70-100 80-100 Main
Side Diarrhea,Nausea
Dizziness Effects Abdominal pain
Drowziness Price/adult 0.25 -
3 2 - 5 dose Mode
of Calcium Channel Delayed action
Action blocker ? Alkylation ?
Oxamniquine
19
Prophylaxis and treatment of protozoal
infectionsTreatment of amebiasis
- Several drugs are available to clear symptomatic
and asymptomatic enteric (luminal) infection
(e.g. dichloroacetamides which have unknown mode
of action) - Metronidazole (Flagyl) is the drug of choice for
invasive amoebiasis (and should be combined with
a lumen acting drug as it is not fully effective
on luminal stages) - Metronidazole is a prodrug which is activated by
an enzyme involved in the microaerobic
fermentation metabolism of E. histolytica
20
Treatment of giardiasis
Metronidazole not FDA approved but used (250 mg
x 3 for 5-7 d) Tinidazole Single dose of 2 g.
Furazolidone approved by the FDA for
giardiasis Paramomycin used for pregnant
women Nitazoxanide recently approved for
giardiasis and cryptosporidosis in children
NitazoxanideAlinia (nitazoxanide)
Tablets (nitazoxanide) for oral suspension
21
Treatment of trichomoniasis
- METRONIDAZOLE 2g orally in a single dose (97
cure rate) - Brand name Flagyl. Sexual partner should also be
treated - TINIDAZOLE recently licensed for use in the
USA. Useful for resistant infections
Sexual education helps prevent the spread of this
disease
22
Metronidazole activation by PFO and NADH
ferredoxin reductases
Pyruvate CoASH
Ferredoxin
NADH
(ox)
NADHFerredoxin oxidoreductase
Pyruvate ferredoxin oxidoreductase
Acetyl- CoA
Ferredoxin
NAD
(red)
R-NO2
R-NO2- RNH2
Ferredoxin reduces the nitro group to a nitro
anion radical and other reduced intermediates
that bind to DNA and proteins
23
Drugs for Malaria
Quinoline and aminoalcohols
Halofantrine
Artemesinin analogues
Other antimalarials
Atovaquone
24
Chemotherapy of Malaria Spectrum of activity
of antimalarial drugs
(doxycyclin)
25
Chloroquine
Still the cornerstone of malaria prophylaxis and
treatment. Concentrated 100-200-fold in
infected RBC's mechanism of action otherwise not
clear. Chloroquine resistant P. falciparum
represents one of the greatest public health
problems in the world today. First reported in
1961 from South America, now in Southeast Asia
and Africa, and spreading rapidly.
26
Chloroquine
- RBC cytoplasm is taken up by endocytosis
- The endocytosis vesicle fuse with the food
vacuole (a homolog of the secondary lysosome)
were hemoglobin digestion occurs - Digestion frees large ammounts of heme
- Heme is toxic to the parasite and is neutralized
by polymerization into the malaria pigment or
hemozoin - Chloroquine accumulates in the food vacuole (its
a weak base and like all lysosomes the FV is an
acidic compartment) - Chloroquine is thought to interfere with the
polymerization and detoxification of heme
27
Chloroquine
28
Mechanisms of drug resistance
drug uptake inhibited
Increased repair
Drug inactivated
drug
drug
cell damage
drug activation
Drug extruded
blocked
drug drug-target complex
altered target
Substrate competition
Simplified scheme illustrating the main
biochemical mechanisms of drug resistance
29
Resistance to chloroquine
1960
1965
1978
1989
http//www.tigr.org/tdb/edb/pfdb/CQR.html
30
Resistance to chloroquine
- Chloroquine resistance is associated with
decreased accumulation of the drug in the food
vacuole - Genetic studies have shown that resistance is
linked to the integral membrane protein PfCRT - This putative transporter localizes to the
membrane of the food vacuole - Studies using parasite cultures suggests that a
series of point mutations in PfCRT are
responsible for resistance - Large field studies have found strong association
of these mutations with chloroquine resistance - Currently the exact physiological function of
PfCRT is unknown
PfCRT, resistance mutations highlighted
31
Pyrimethamine and sulfadoxine (Fansidar)
An antifolate-sulfonamide combination especially
designed for antimalarial use. Has been useful
in treating chloroquine resistant P. falciparum,
but causes fatal cutaneous reaction in 1/20,000
users.
Sulfadoxine The sulfonamides are structural
analogues of para-aminobenzoic acid (PABA),
and competitive inhibitors of dihydropteroate
synthetase. Pyrimethamine An antifolate, a
highly selective and powerful competitive
inhibitor of dihydrofolate reductase.
32
Folate metabolism
PLASMODIUM
HUMAN
Pteridine PABA
Dihydropteroate synthetase
Dihydropteroic acid Dihyrofolate Tetrahydrofo
late FAH4 cofactors
GLUTAMATE
Preformed dietary folates Tetrahydrofolate
FAH4 cofactors
Dihydrofolate reductase
NADPH NADP
NADPH NADP
Dihydrofolate reductase
Thymidine Purines Methionine Glycine
f-met-tRNA DNA DNA
RNA PROTEINS
Thymidine Purines Methionine Glycine
f-met-tRNA DNA DNA
RNA PROTEINS
Parasites synthesize their own folic acid unlike
man, they cannot import preformed folic acid.
Tetrahydrofolic acid is an essential cofactor for
the synthesis of nucleic acid precursors, and
some amino acids.
33
The combination FANSIDAR
The mixture of pyrimethamine and sulfadoxine in a
fixed ratio (Fansidar) synergistically inhibits
folate synthesis. The combination was designed
so that both drugs have similar pharmakokinetics
in man. Mechanism of synergism still
controversial perhaps because of multiple
blockades in a single metabolic pathway. The
advantages of the synergistic combination
include -less of each component required for
the same antiparasitic effect (lessens likelihood
of toxicity) -reduced likelihood of developing
resistance -can achieve antiparasitic effects
which either drug alone cannot. Basis for
selective toxicity - mammalian cells have no
dihydropteroyl synthetase they must use
preformed folates. - mammalian dihydrofolate
reductase is 3,600 times less sensitive to
pyrimethamine than is the enzyme of
Plasmodium. - biosynthesis in parasites can be
synergistically inhibited by an antifolate
sulfonamide combination. Resistance to Fansidar
has been reported for all four species of
Plasmodium. Molecular mechanism, include -
reduced drug transport - increased production of
p-aminobenzoic acid - increased levels of
dihydropteroyl synthetase and/or dihydrofolate
reductase - mutation in dihydropteroyl
synthetase and/or dihydrofolate reductase
34
Antifolate resistance developed very fast (5
years)
35
Quinine
"The oldest chemotherpeutic drug still in use",
resurrected to treat and prophylaxis against
chloroquine resistant P. falciparum. More toxic
and less convenient than chloroquine.
36
New antimalarial drugs
Three relatively new antimalarial drugs are all
active against the erythrocytic, but not the
hepatic stage of the parasites.
QINGHAOSU (artemisinin derivatives)
HALOFANTRINE
MEFLOQUINE
DOXYCYCLINE
PROPHYLAXIS
37
Atovaquone-Proguanil (Malarone)
Atovaquone
Binding of atovaquone to the ubiquinol Oxidation
pocket of yeast cytochrome bc1
Proguanil
Prophylaxis and treatment
38
Combinations of Artemisinin and other
antimalarial are promising
- Extracts of Artemisia annua (sweet wormwood) have
long been used in traditional Chinese medicine to
treat fever - Chinese investigators extracted the active
ingredients and showed that they and there
chemical modifications are powerful
anti-malarials - However mono-therapy results in high level of
recrudescence - Combining Artemisinin with other drugs have been
very successful especially for severe malaria - Artemisinin acts very fast which helps to reduce
mortality and get patients out of their coma
quickly
39
Primaquine
The only antimalarial with significant reliable
activity against exoerythrocytic parasites.
Mechanism of action unknown. Glucose 6-phosphate
dehydrogenase deficiency, the first known
genetic abnormality associated with an enzyme,
was discovered and reported in 1956 as a result
of investigations of the hemolytic anemia induced
in some individuals by primaquine.
40
Parasites, too Time to Development of
Resistance to Antimalarial Drugs
1940
1950
1960
1970
1980
1990
41
Malaria Drug Pipeline
Discovery phase Protein farnesyltransferase
Fatty acid biosynthesis (Fab I Fab H) Cysteine
proteases (falcipains) Dihydrofolate reductase
(DHFR-TS) folic acid biosynthesis
Predevelopment phase Manzamine alkaloids Novel
DB289 analogues Novel tetracyclines 8-Aminoquinoli
nes
Development phase 4(1H)-Pyridones Isoquine
(4-aminoquinoline) Dihydroartemesinin /
piperaquine (Artekin) Tafenoquine
Clinical trials OZ277 (synthetic peroxide Phase
I) Artemisone (semi-synthetic peroxide Phase
I) Pyronaridine-Artesunate (Phase I) DB289 (oral
diamidine Phase II) Pediatric Artemether-Lumefant
rine (Coartem Phase II) Chlorproguanil-Dapsone-Ar
tesunate (CDA Phase II) Chlorproguanil-Dapsone
(LapDap Phase III) Intravenous Artesunate
42
Chemotherapy of toxoplasmosis
- Inhibitors of dihydrofolate reductase Pyrimetham
ine in combination with sulfonamides - Sulfonamides Sulfadiazine, sulfamethazine,
sulfamerzaine. - Clindamycin
- Macrolides and azalides Roxithromycin,
azythromycin, clarithromycin, spiramycin - Tetracyclines Doxycline, minocycline
- Hydroxynaphthoquinones
- Atovaquone.
- Others Eimycine, aprinocid, dapsone, quinghasou,
pentamidine - Combination therapy
- pyrimethamine-dapsone, clarithromycin-minocycline
, azithromycin-pyrimethamine, azithromycin-sulfad
iazine, etc - Biological response modifiers Cytokines
(IFN-?, IL-2, TNF, IL-1, IFN-?) in combination
with chemotherapy
43
Chemotherapy of cryptosporidiosis
Latest drug to be used- a nitrothiazole
benzamide with broad antimicrobial spectrum
Chemical structures for nitazoxanide (a) and its
first metabolite in human plasma, tizoxanide
(b) Giles et al., Trends in Parasitology, 18,
95-97, 2002..
44
Drugs for Human African Trypanosomiasis
Suramin
Pentamidine
Melarsoprol
Eflornithine (D,L-?-DFMO)
45
Chemotherapy of HAT
African trypanosomes Winthout central nervous
system (CNS) involvement pentamidine (1941)
(also used for Toxoplasma gondii) and
suramin (1921) With CNS involvement
Melarsoprol (1949), and a-difluoromethylornitine
(1990).
46
Drug resistance in human and animal African
trypanosomiasis
Distribution of drug-resistant trypanosomes in
sub-Saharan Africa. Note that drug resistance is
more prevalent and widespread amongst
trypanosomes of animal origin, while reports of
treatment failure in human trypanosomiasis are
confined to a belt stretching from Angola,
through D.R. of the Congo, northwestern Uganda,
and southern Sudan. (Drug resistance in
Trypanosoma brucei spp., the causative agents of
sleeping sickness in man and nagana in cattle. E.
Matovu, T. Seebeck, J. C. K. Enyarua and R.
Kaminsky. Microbes and Infection/Volume 3, Issue
9, July 2001/Pages 763-770)
47
Drugs for Chagas Disease
Nifurtimox
Benznidazole
48
Chemotherapy of Chagas disease
American trypanosomiasis
1. Prevention of blood transmission by blood
transfusion crystal violet (uncoupler of
oxidative phosphorylation) 2. Acute
infection nifurtimox (mode of action through
oxidative stress) benznidazole (covalent
binding to DNA and proteins).
49
Drugs for Leishmaniasis
Pentostam
Pentamidine
Amphotericin B (AmBisome)
Paromomycin (Aminosidine)
Miltefosine
50
Chemotherapy of Leishmaniasis
1. Visceral leishmaniasis (L. donovani)
Pentavalent antimonials (sodium stibogluconate)
2.Mucosal (L. braziliensis) and cutaneous (L.
mexicana, L. tropica) leishmaniasis
Amphotericin B, pentavalent antimonials. In
Liposome formulations Ambisome
51
Chemotherapy of Leishmaniasis
First oral treatment for visceral leishmaniasis,
also effective in other forms
52
Kinetoplastid Drug Pipeline
Discovery phase Trypanothione reductase
(HAT/CHA/LEISH) Protein farnesyltransferase
(HAT/CHA/LEISH) Cysteine proteases
(HAT/CHA/LEISH) Whole organism screens of
libraries and compound collections
Predevelopment phase Megazol (HAT)
Development phase Nifurtimox (late stage
HAT) Oral Berenil (early stage HAT) DFMO
enantiomers and oral DFMO (HAT) Antifungal azoles
(CHA)
Clinical trials K777 (Phase I cysteine protease
inhibitor for CHA) DB289 (Phase II oral
diamidine for HAT) Paromomycin (Phase III VL in
Africa)
53
Some Hope for Change
- Huge involvement of major foundations (Gates,
Wellcome Trust, Novartis, etc) - Drug Donations by Major Pharmaceutical Companies
- 36 million treatments to 14 million people in
2007 - Merck Mectizan (Ivermectin) Onchocercasis and
Lymphatic Filariasis - Pfizer Zithromax (Azythromycin) Trachoma
- GSK Albendazole Lymphatic Filariasis
- MedPharm Praziquantel Schistosomiasis
- J J Mebendazole Soil-transmitted helminths
(hookworms, - ascaris, trichuris)
- Bayer Nifurtimox Chagas
gt 1 billion dollars
54
Some Hope for Change
- US Army
- A Nonprofit pharmaceutical company
- Public/Private Partnerships for Drug
Development.
(Paramomycin for Leishmaniases)
55
(No Transcript)
56
References
- Fairlamb, A. (2005) Making Discovery research in
TDR relevant to tropical diseases.
UNICEF/UNDP/World Bank/WHO Special Programme for
Research and Training in Tropical Diseases (TDR). - Docampo, R., and Moreno, S.N.J. (2003) Current
chemotherapy of human African trypanosomiasis.
Parasitol. Res. 90, S10-S13. - Urbina, J.A., and Docampo, R. (2003) Specific
chemotherapy of Chagas disease controversies and
advances. Trends Parasitol. 19, 495-501.