Unit 7 Change in Assignment: Reminder - PowerPoint PPT Presentation
1 / 29
Title:
Unit 7 Change in Assignment: Reminder
Description:
Study objectives 1-17 from U7 course pack. The exam will not ... Behavioral gerontology. SOs will be handed out in class for Dr. ... Gerontology ... – PowerPoint PPT presentation
Number of Views:70
Avg rating:3.0/5.0
Title: Unit 7 Change in Assignment: Reminder
1
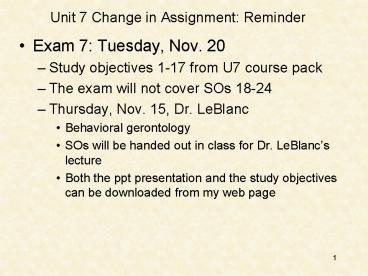
Unit 7 Change in Assignment Reminder
- Exam 7 Tuesday, Nov. 20
- Study objectives 1-17 from U7 course pack
- The exam will not cover SOs 18-24
- Thursday, Nov. 15, Dr. LeBlanc
- Behavioral gerontology
- SOs will be handed out in class for Dr. LeBlancs
lecture - Both the ppt presentation and the study
objectives can be downloaded from my web page
2
Unit 8 Very Different Assignment!
- Topics covered
- Certification in behavior analysis
- Research and professional ethics
- Unit Assignment 2 parts
- 20 pts over study objectives in course pack
- 15 pts for completion of first 7 modules of an
on-line training program about research ethics
(Behavioral and social sciences modules) - Research and professional ethics have the same
overarching guidelines/principles, and thus there
are a lot of similarities between them.
3
Unit 8 Very Different Assignment!
- On-line Training Program
- You must hand in a computer print out that you
have completed the on-line training on the day of
U8 exam, which is Tuesday, December 4 (no
electronic copies via email) - If you have already completed this training, you
only need to print off a copy of the page that
indicates that you have completed it. You dont
need to do it again. - Completion criterion established by HSIRB 80
correct on the quiz after the unit. Quizzes can
be retaken until you obtain the 80 criterion. - If you do not hand this in on the day of the exam
- no credit. Late assignments will not be
accepted. - See Study Objectives for grading criteria
- See Study Objectives for instructions on logging
onto the training program.
4
Unit 7 Introduction
- Health Care or Behavioral Medicine (clinical/BA)
- Psychologists work with physicians to deal with
medical problems and behavioral problems
associated with illness and medical conditions - Behaviors that result from medical problems
- Behaviors that cause medical problems (eating
disorders, cutting) - Behaviors that can solve medical problems
(health-related behaviors such as exercising and
eating healthy diets that can reduce hypertension
and heart disease) - Some areas of application
- ADHD (school psychologists and physicians)
- Gerontology - dementia, alzheimers
- Pediatric eating disorders (Johns Hopkins,
Baltimore Atlanta) - Rehabilitation from surgery, heart attacks,
strokes, head injuries - Chronic pain (Fordyces work, still state of the
art)
(hard to tell the difference, anarexia, bullemia,
Johnsons - BAAM, Pediatricians, preferred
treatment was behavioral for ADHD - ONLY one that
was effective)
5
SO1 Epileptic seizures and systematic
desensitization and relaxation procedures
- Why is it interesting and surprising that
behavioral procedures can reduce the severity and
frequency of epileptic seizures?
Epileptic seizures are caused by physiological
(biological) problems, usually a lesion in the
brain. They are organic. That is, they are not
learned behavioral problems. Even so, behavioral
procedures such as pogressive muscle relaxation
and other types of relaxation procedures can
reduce both the frequency and severity of
seizures.
6
SO1 Epileptic seizures, cont.
- Why is it that progressive muscle relaxation and
other relaxation procedures may reduce epileptic
seizures?
Epileptic seizures are often precipitated
(brought on) by stress. The behavioral
procedures reduce stress.
(meditation, yoga, exercising)
7
SO2 Explain what was maintaining the coughing
behavior of the girl described in the case study.
- The case involves an adolescent girl diagnosed
with hysterical neurosis. - At times, she coughed 40-50 times per minute!
(think about that) - She had also not talked for over two years
- Due to the coughing, she consumed over 2 gallons
of water a day - While she ate relatively normally, she avoided
meats and foods that would irritate her throat - Previous treatments psychotherapy, sleep
therapy, hypnosis, and acupuncture - She was hospitalized and treated with contingency
management procedures (behavioral treatment)
8
SO2 Cont.
- Explain what was maintaining the coughing
behavior of the girl described in the case study.
State the names of the behavioral principles.
First
- Attention from staff and parents (positive
reinforcement) - Whenever she coughed, staff would rush to her
bedside to console her, as would her parents if
they were there
Second
- Coughing terminated or avoided aversive
situations - such as interpersonal contacts and school.
Thus it - was an escape or avoidance behavior.
- (escape or avoidance - types of negative
reinforcement)
9
SO2 Contingency Management Procedure (not for
the exam)
- Extinction of coughing behavior
- Instructed staff to not pay attention to her when
she was coughing, but instead to pay attention to
her when she was not coughing (differential
reinforcement of other behavior) - Token economy
- She earned points for interacting with staff and
others on the hospital ward - Point contingencies were then moved from the ward
to the entire hospital, to the home community,
and finally to her peer group - Vocalizations were also shaped (remember she had
been mute for over two years)
10
SO2 Results (not for the exam)
- After only six weeks
- She wasnt coughing anymore
- She was speaking fluently
- Follow-up after 20 months
- The girl was still symptom free. That is, she
wasnt coughing and she was talking and
interacting with others normally.
Question
Given that the token economy program was
withdrawn, but the girl still did not cough and
was still interacting normally with others, can
we attribute her behaviors to the token economy
program?
11
SO3 Introduction Fordyces behavioral analysis
of pain
- Fordyce developed a behavioral analysis of
chronic pain (chronic back pain) and his analysis
and treatment are still considered to be state of
the art - His analysis (SO3)
- When people are immobilized by pain (that is,
they are not active, they dont go to work, they
sit around and complain), the problem may not be
due to the actual painful stimulation, but rather
due to the operant pain-related behaviors that
have been shaped up and reinforced by the
persons environment (the individuals with which
that the person interacts) - Thus, his treatment program does not target the
actual pain, but rather the operant behaviors
that people reinforce when a person is in pain.
(chronic back pain, but relevant to any type of
chronic pain, illness, medical condition behavior
s as target rather than behavioral contingencies)
12
SO3 Cont., but not for the exam
- Think about it - when someone is in pain or
discomfort, how do you react? What behaviors do
you reinforce? - Are you helping or hurting the individual to get
better when you reinforce operant pain-related
behaviors? - Clearly, you dont want to ignore reports of pain
in case some type of medical treatment is
required and you certainly want to be sympathetic
to show you care. On the other hand, are you
helping too much and caring too much. - Skinners essay On the ethics of helping
people.
13
SO3 Cont., but not for the exam
- My personal experiences - father and mother
- Father - died of bone cancer in 1995
- Mother as the ultimate care-giver
- She said (and I quote), I can make anyone into
an invalid. - About every two weeks, my father would stop
eating - Within an hour after I was there, I was able to
get him to eat - Engaging in other behaviors, reinforced by
tactile stimulation
(home hospice, nursing home, stroke, squeeze,
tossing ball, stuffed animal, real men dont play
with, red bow)
14
SO3 Cont., but not for the exam
- This is typically not a problem when individuals
are ill for a short period of time (cold, flu) - Why? After the person recovers, you are not going
to continue to reinforce whining and complaining! - The problem develops when individuals are ill or
in pain for long periods of time, e.g., six
months or longer - Please do not leave class and say Dickinson is
so cold and hard-hearted! She told us never to
show how much we care when someone is sick!
(whiners and complainers)
15
SO4 Analysis of care givers behavior Learn the
diagram.
SD R ----gt
Consequence, Sr
Ill significant other saying Thanks for caring!
I dont know what I would do without you!
Ill significant other engaging in
pain-related behaviors
Oh, poor baby!
Not for the exam, but note The response of
care giver then serves as a reinforcer for the
operant pain-related behavior of the significant
other R of ill person Consequence for ill
person Complaining Oh, poor
baby!
16
SO5 Should we refer to individuals who engage in
excessive pain-related behaviors as
psychosomatic? Why or why not?
No. Operant conditioning is automatic - it can
and does work without the awareness or
voluntary control of the individual. When care
givers and others in the environment frequently
and heavily reinforce operant pain-related
behaviors, they will increase in frequency.
Individuals are not faking it, nor is it all in
their heads. Rather, the pain-related behaviors
have been shaped up and reinforced by others in
the environment. To alter those behaviors, the
reinforcement provided by others must be altered.
(how many of you have whining and complaining
sos? Are you in part responsible for that?)
17
SOs 6-12 Introduction to Fordyces intervention,
the three essential features
- Extinction of all operant pain-related behaviors
- Change in the contingencies for physical therapy
- Change from medication on demand to time-based
medication - Also, decrease in dosage of medication,
administered in a cocktail (with full consent
of patient and monitoring by physician)
(hospital-based program, with patients giving
informed consent for procedures and being
monitored by a physician, multiple meds, pain
reliever, sleeping pills, antidepressants,)
18
SO6 Extinction of pain-related behaviors. Learn
diagrams.
Before intervention
R -----------gt
Consequences All pain related behaviors
A. Sr attention from others
e.g., complaints inactivity B. Sr-
escape/avoidance from unpleas. act.
After intervention
R ------------gt
Consequences All pain related behaviors
Extinction e.g., complaints,
inactivity
SO7 How do you extinguish a negatively
reinforced response? Lets say that when a friend
comes to visit the caregiver, the ill person
begins to complain loudly, increaes the sound of
the TV. The reinforcer is that the person leaves.
19
SO7 How do you extinguish a negatively
reinforced response?
Lets say that when a friend comes to visit the
caregiver, the ill person begins to complain
loudly, throws the newspaper or books on the
floor, and/or increases the sound of the TV,
making it very difficult for the friend and
caregiver to chat. In the past, after a few
minutes, the caregiver has asked the friend to
leave because the ill person is just having a
bad moment or day. The reinforcer for the ill
person is that the friend leaves (and thus the
caregiver is available to pay more attention to
the ill person). What should the caregiver do in
order to extinguish the complaining, throwing
things, and increasing the sound on the TV?
(how would you diagram this? part of so)
20
SO8 Physical Therapy, before and after. Learn
diagrams.
Before intervention
R
Consequences Complaints when doing A.
Sr rest physical therapy
B. SR- escape pain
After intervention
R
Consequences Completion of PT req.
Sr rest
SR- escape pain
(Main contingency change change in the
behaviors, while rein stays the same)
21
SO9 Medication on demand, before intervention
diagrams
MO Response--gtSr/SD Response--gtConsequen
ce
Pain Get meds Sight of meds Take meds
Decrease in pain (SR-) Pain Get meds
Sight of meds Take meds Attention from
others (Sr)
Sight of others
- SO 10 (first diagram above)
- What is the reinforcer establishing effect of
pain as the MO? - What is the evocative effect of pain as the MO?
- What is the SD evocative effect of pain as the
MO? - What is the conditioned reinforcer establishing
effect of pain as the MO?
(on demand, take 1 or 2 when in pain, not to
exceed 6 in 24 hours the MO is completely
responsible for why people take more medication
on demand than when it is time based.)
22
SO11 Time-based medication, after intervention
diagrams
MO Response--gtStimulus
Response--gtConsequence
No or Get meds Sight of meds
Take meds No or little decrease Little pain
in pain No or
Get meds Sight of meds Take meds No or
little attention Little pain
Sight of others from
others
- SO 12 (first diagram above)
- What is the reinforcer abolishing effect of no
pain, the MO? - What is the abative effect of no pain as the MO?
- What is the SD abative effect of no pain as the
MO? - What is the conditioned reinforcer abolishing
effect of no pain as the MO?
23
SO13 Not for exam, but some interesting issues
- The 36 patients had pain from 4 1/2 - 30 years
and none had worked in over three years - The inpatient program lasted only 7 weeks!
- Patients reported having much less pain
- Fascinating, since Fordyces program did not
target the actual pain, but rather the operant
pain-related behaviors - Because pain is self-reported, we really dont
know whether the pain decreased (sometimes
physical activity will actually decrease pain) - Patients were taking much less medication (see p.
89) - They were taking fewer meds and less dosages
(decreased from 2 to 1 dosage units) - Before, many were taking multiple meds
(narcotic/analgesic, analgesic, sedative/hypnotic)
(very common, multiple meds)
24
SO14 Results of a follow-up study by
ReinhardtStudy was conducted by Roberts at U. of
Minn
14A. What percentage of patients who completed
the program were living normal lives (including
working)?
77
14B. What percentage of patients who refused
treatment were not working?
83, which means only 17 were working
14C. How many prescription meds were the
successful patients taking?
None
14D. How many different prescription meds were
the patients who refused treatment taking?
An average of over three!
25
SO15 Table 5-4 Compliance with medication
regimens
- Zifferblatt analyzes the circumstances under
which individuals are likely to take their
medications and when they are not - His analysis takes into account the following
factors Cue specificity (is the antecedent event
easily detected and specific to the response),
antecedent event (actually, the MO), the behavior
of taking the medication, consequence, latency of
the consequence and, finally, the likelihood that
the person will take the medication in the future.
26
SO15 Examples from the table
First two in table
Upset stomach Take antacid --gt Relief of
discomfort (5-10 min) Likely Headache
Take headache powder --gt Relief of headache
(10-15 min) Likely
Some modified examples from the remainder of the
table
No ant. event Take aspirin --gt Avoid arthritic
pain (prevent, ?) Not likely No ant.
event Take calcuim --gt Avoid osteoperosis
(prevent, ?) Not likely No ant. event Take
vitamin C --gt Avoid cold (prevent,?)
Not likely
What behavioral contingency (principle) is
represented by the first two examples? What
behavioral contingency is represented by the
other examples?
27
SO16 Why escape contingencies control behavior
more effectively than avoidance contingencies
- With escape contingencies, there is
- An MO which
- Increases the reinforcing value of the
consequence (usually a decrease in pain with
medications) - Evokes behaviors that have in the past been
reinforced by that consequence (taking the med) - An immediate, salient (obvious) consequence (pain
reduction) that follows the behavior (in this
case, taking the med) - With (unsignaled) avoidance contingencies, there
is - No MO
- No immediate, salient consequence that follows
the behavior (the behavior postpones or avoids an
aversive stimulus)
28
SO17 Taking medication for a headache vs. taking
medication for blood pressure
Taking medication for a headache
MO R ----gt
Consequence Headache Take meds
Decrease headache
- The MO makes the decrease in pain reinforcing
- The MO evokes taking meds
- Taking the meds reduces the pain
Taking medication for a high blood pressure
No MO R ----gt
Consequence High blood pressure Take meds
Low blood pressure (not detectable)
(not detectable)
- No MO to make decrease in blood pressure
reinforcing - No MO to evoke taking meds
- Taking the meds does not result in a salient
consequence
(how could you create an MO for high blood
pressure? What role might VB play?)
29
The End
- Questions?
- Instructional Assistance Hours
- Monday, Nov. 19
- 500 to 630 pm
- Wood Hall lounge, first floor
- Lexi is in the hot seat