The Respiratory System - PowerPoint PPT Presentation
1 / 54
Title:
The Respiratory System
Description:
The Respiratory System Supplies O2 to blood and gets rid of CO2 Consists of Nose and nasal cavity Throat (pharynx) Voice box (larynx) Windpipe (trachea) – PowerPoint PPT presentation
Number of Views:162
Avg rating:3.0/5.0
Title: The Respiratory System
1
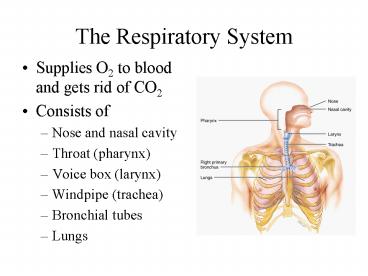
The Respiratory System
- Supplies O2 to blood and gets rid of CO2
- Consists of
- Nose and nasal cavity
- Throat (pharynx)
- Voice box (larynx)
- Windpipe (trachea)
- Bronchial tubes
- Lungs
2
Functions of the Respiratory System
- Cleaning and filtering air
- Ventilation
- Gas exchange
- Gas transport
- Smell
- Speech
3
Respiratory System Anatomy
- Upper respiratory system (tract)
- Nose and nasal cavity
- Pharynx throat
- Lower respiratory system (tract)
- Larynx voicebox
- Trachea windpipe
- Bronchi airways
- Lungs
- Refer to locations of infections
4
Nose -- Internal Structures
--------------Nasal concha
Internal Naris--------------
-------External Naris (nostril)
- External nares (nostrils) open into nasal cavity
- Divided into two sides by nasal septum (not
shown) - Nasal septum is composed of bone cartilage
- Nasal conchae on lateral walls swirl air and
expose lining to more air - Internal nares (choanae) are openings to pharynx
5
Functions of the Nasal Structures
- Olfactory epithelium for sense of smell
- Pseudostratified ciliated columnar with goblet
cells lines nasal cavity - Large blood supply warms air
- Mucous moistens air traps dust
- Cilia move mucous towards pharynx
- Paranasal sinuses open into nasal cavity
- Found in ethmoid, sphenoid, frontal maxillary
- Lighten skull resonate voice
6
Pharynx
- Five inch long muscular tube
- Extends from internal nares to end of larynx
- Functions
- passageway for food and air
- resonating chamber for speech production
- tonsil (lymphatic tissue) protect from infection
- Distinct regions -- nasopharynx, oropharynx and
laryngopharynx
7
Nasopharynx
Nasopharynx-------------
- From internal nares to soft palate
- Openings of auditory (Eustachian) tubes from
middle ear cavity - Adenoid or pharyngeal tonsil in roof
- Passageway for air only
- pseudostratified ciliated columnar epithelium
with goblet
8
Oropharynx
Nasopharynx-------------
Oropharynx---------------
- From soft palate to epiglottis
- Palatine tonsils found in side walls, lingual
tonsils in base of tongue - Common passageway for food air
- Stratified squamous epithelium
9
Laryngopharynx
Nasopharynx-------------
Oropharynx---------------
Laryngopharynx-----
-------------Epiglottis
------------------Cricoid cartilage
Esophagus---------------------------
- Extends from epiglottis to cricoid cartilage
- Common passageway for food air
- Ends as esophagus inferiorly
- Stratified squamous epithelium
10
Larynx
- Cartilage connective tissue tube
- Constructed of 3 single 3 paired cartilages
- Contains vocal cords voice box
11
Trachea
- Five inches long one inch in diameter
- Extends from larynx into chest where it divides
to form two bronchi(us) - 16 to 20 incomplete
- C-shaped cartilage rings
- Lined with pseudostratified epithelium
Trachea---------------
Bronchus---------------------------
--------------Bronchus
12
Gross Anatomy of Lungs
- Base, apex, cardiac notch
- Oblique horizontal fissure in right lung
results in 3 lobes - Oblique fissure only in left lung produces 2 lobes
13
Mediastinal Surface of Lungs
- Blood vessels airways enter lungs at hilus
- Forms root of lungs
- Covered with pleura (parietal becomes visceral)
14
Lung Lobules
- Lung lobules are smaller compartments within
lobes - Consist of
- Terminal bronchiole supplies air to lobule
- Each terminal bronchiole divides into several
respiratory bronchioles - Respiratory bronchioles divide into alveolar
ducts - Alveolar ducts supply air to alveolar (air) sacs
- Each sac composed of two or more smaller
alveoli(us) - Extensive blood supply
---terminal bronchiole
---respiratory bronchiole
---alveolar sac
alveolar duct---------------------
-------alveolus
15
Details of Respiratory Membrane
- Four tissue layers two fluid layers make the
respiratory membrane.
16
Respiratory Physiology
- Ventilation, Gas Exchange, Gas Transport and
Control of Ventilation
17
Pulmonary (alveolar) Ventilation
- Basic concepts and definitions
- Ventilation called negative draft ventilation
- Breathing in called inspiration or inhalation
- Breathing out called expiration or exhalation
- Pressure within the lung called alveolar pressure
- Pressure within the pleural cavities called
intrapleural pressure always less than
atmospheric pressure. Keeps lungs attached to
chest wall and inflated
18
Breathing or Pulmonary VentilationQuiet
Ventilation - Eupnea
- Air moves into lungs when pressure inside lungs
is less than atmospheric pressure - Contraction of diaphragm and rib muscles
(external intercostals) enlarges chest and
reduces alveolar pressure to below atmospheric
pressure - Air drafts into lungs negative draft
- inspiration or inhalation
19
Breathing or Pulmonary Ventilation
- Air moves out of lungs when pressure inside lungs
is greater than atmospheric pressure - Diaphragm and rib muscles (ext. Intercostals)
relax - Chest gets smaller
- Elastic recoil of alveoli creates Alveolar
pressure greater than atmospheric pressure - Air is pushed (squeezed) out of lungs
- Expiration or exhalation
20
Drawing of Ventilation Cycle
21
Animation of Ventilation
22
Boyles Law and Ventilation
- As size of container increases, pressure inside
decreases - As the size of closed container decreases,
pressure inside is increased
23
Forced Ventilation During Exercise
- Forced inspiration
- Require larger decreases in intrapleural and
alveolar pressures - Diaphragm and external rib muscles contract more
forcefully making the chest wider. - Other back muscles become involved
- Results in deeper breaths
24
Forced Ventilation During Exercise
- Forced Expiration
- Require larger increases in intrapleural and
alveolar pressures - Diaphragm and external intercostal rib muscles
relax - Internal intercostal rib muscles contract
compressing rib cage making the chest narrower. - Abdominal muscles contract compressing abdomen
forcing diaphragm to move up further - Air forced out
25
Lung Volumes and Capacities
- Volume is one measure of quantity of air
- Capacity is sum of two or more volumes
- Spirometer or respirometer device for measuring
volumes and capacities - Record called spirogram
26
Lung Volumes and Capacities
- Ventilation rate is number of breaths per minute
- Resting ventilation rate averages12 breaths per
minute (Range 12 to 20 breaths / minute) - Tidal Volume (VT) is amount of air in one breath
- Resting tidal volume is about 500 mL
27
Lung Volumes and Capacities
- If resting tidal volume (VT) 500 mL, then
- 350 mL reaches alveoli
- Remaining 150 mL remains in conducting airways
above alveoli - Called anatomic dead air
- Dead air does not participate in gas exchange
- The 350 mL in alveoli is the only air
participating in gas exchange
28
Lung Volumes and Capacities
- Lung volumes
- (1) Tidal Volume (Vt) Volume of air in one breath
- (2) Inspiratory Reserve Volume (IRV) Volume of
air inspired in addition to VT - (3) Expiratory Reserve Volume (ERV) Volume of air
expired in addition to VT - (4) Residual Volume (RV) Volume of air that
cannot be expired even with maximum forced
expiration.
29
Lung Volumes and Capacities
- Lung Capacities
- (1) Inspiratory Capacity (IC) Vt IRV
- (2) Functional Residual Capacity
- (FRC) RV ERV
- (3) Vital Capacity (VC) Vt IRV ERV
- (4) Total Lung Capacity (TLC) VC RV
30
Lung Volumes and Capacities
- FEV1 stands for forced expiratory volume in one
second - Percentage of vital capacity expired in 1 second
- Should be 75 or higher
- If not, may indicate chronic obstructive
pulmonary disease such as chronic bronchitis or
emphysema
31
Spirogram
32
Gas exchange
- In lungs External respiration
- Diffusion of O2 from alveolar air into blood
- Diffusion of CO2 from the blood into alveolar air
- In tissues Internal respiration
- Diffusion of O2 from blood into tissues
- Diffusion of CO2 from tissues into blood
- Diffusion across the extremely thin respiratory
membrane from higher to lower concentrations of
gases
33
Gas Exchange Diagram
External Respiration
Internal Respiration
O2
O2
CO2
CO2
O2
Oxygenated Blood
Alveolus
CO2
O2
CO2
O2
O2
CO2
CO2
Deoxygenated Blood
Tissues
34
Measurements of Gas Concentrations
- Daltons Law of Partial Pressure
- In a mixture of gasses, the total pressure is
equal to the sum of pressures contributed by each
individual gas - These individual pressures are partial pressures
- Symbol for the partial pressure of a gas is Pg
where g stands for the specific gas
35
Measurements of Gas Concentrations
- Partial pressures
- Our atmosphere is mixture of nitrogen, oxygen,
argon, carbon dioxide and other trace gasses - Total pressure of our atmosphere is essentially
equal to PN2 PO2 PAr PCO2
36
Measurements of Gas Concentrations
- Partial pressures
- Since Oxygen (O2) 21 of our atmosphere, its
PO2 0.21 x 760 159 mm Hg - Since CO2 0.04 of our atmosphere, its PCO2
0.0004 x 760 0.3 mm Hg - O2 and CO2 are the most important respiratory
gases, so their partial pressures are used in our
discussion of gas exchange
37
Partial Pressures and Gas Exchange
- Partial pressure of O2 and CO2 in oxygenated
blood - PaO2 is symbol for partial pressure of oxygen in
oxygenated (arterial ) blood and is about 95 mm
Hg - PaCO2 is symbol for partial pressure of carbon
dioxide in oxygenated (arterial) blood and is
about 40 mm Hg
38
Partial Pressures and Gas Exchange
- Partial pressure of O2 and CO2 in deoxygenated
venous blood - PvO2 is symbol for partial pressure of oxygen in
deoxygenated (venous) blood and is about 40 mm Hg - PvCO2 is symbol for partial pressure of carbon
dioxide in oxygenated (venous) blood and is
about 45 mm Hg
39
Gas Exchange Diagram
External Respiration
Internal Respiration
O2
PaO295 mm Hg
CO2
PaCO240 mm Hg
O2
Oxygenated Blood
Alveolus
CO2
O2
CO2
PvO240 mm Hg
O2
PvCO245 mm Hg
CO2
Deoxygenated Blood
Tissues
40
Henrys Law and Gas Exchange
- More oxygen in the air, results in more oxygen in
the blood - Formally stated
- The amount of gas that will dissolve in a liquid
is proportional to-
(1) Partial pressure of the gas - (2) Solubility of the gas in the liquid
(3) Temperature of the liquid
41
Gas Transport
- Gas Pickup and Delivery
42
Oxygen Transport
- 98.5 of O2 carried by iron of hemoglobin
- Only 1.5 dissolves in plasma
- Hemoglobin (Hb) picks-up oxygen in lungs and
delivers it to tissues - Becomes oxyhemoglobin (Hb-O2) when picks-up O2
- Becomes deoxyhemoglobin (Hb-H) when O2 delivered
43
Hemoglobin Molecule
- Each Hb molecule has four heme groups, and each
heme contains an iron atom (Fe) - Iron has affinity for O2
- This affinity greater in lungs than in tissues.
44
Oxygen Saturation
- Hb molecule saturated when its iron binds four O2
molecules - Hb unsaturated if iron has no O2 molecules
- Percent saturation refers to how many irons of
the Hb molecules have O2 - Arterial blood has the higher percent saturation
45
Loading and Unloading
- Pick-up of O2 in lungs called loading
- Delivery of O2 to tissues called unloading
46
Factors in O2 Loading and Unloading
- (1) PO2 main factor in O2 loading and unloading
- Higher Po2 in lungs favors loading
- In lung capillaries Po2 is high and O2 binds to
Hb - Lower PO2 in tissues favors unloading
- In tissue capillaries PO2 is low and Hb-O2
releases O2 - In resting person, nearly 25 of O2 unloaded
47
Other Factors in Loading and Unloading
- (2) Acid
- Lower pH of tissues capillaries favors unloading
- Hemoglobin has less affinity for O2 at lower pH
- Bohr Effect
- Higher pH of lungs capillaries favors loading
- Hb has higher affinity for O2 at higher pH
48
Other Factors continued
- (3) PCo2
- Higher PCo2 of tissue capillaries favors
unloading - Related to pH as follows
- Carbon dioxide water ? carbonic acid or
- CO2 H2O ? H2CO3 ? H HCO3-
- CO2 forms acid when dissolved in water
- (4) Temperature
- Higher temperature of tissues favors unloading
- Lower temperature of lungs favors loading
49
Other Factors continued
- (5) BPG (2,3 bisphosphoglycerate)
- When BPG binds to hemoglobin in tissue
capillaries, Hemoglobin loosens its grip on O2 - More O2 released into tissues
- Higher metabolic rate, higher altitude and
certain hormones increase BPG formation
50
Oxygen Transport Diagram
External Respiration
Internal Respiration
O2
Hb-O2
Hb-O2
Oxyhemoglobin
Alveolus
Hb-H
Hb-O2
Hb-H
- Loading
- Higher Po2
- Higher pH
- Lower Temp
- UnLoading
- Lower Po2
- Lower pH
- Higher Temp
- ?BPG
O2
Hb-H
Deoxyhemoglobin
Aerobic Cell Respiration
Tissues
51
Fetal Hemoglobin Oxygen Affinity
- Differs from adult hemoglobin in structure
affinity for binding O2 - Maternal blood in placenta has less O2 than
normal oxygenated blood - When Po2 is low, fetal hemoglobin can still bind
enough O2
52
Carbon Monoxide Poisoning
- CO from car exhaust tobacco smoke
- Binds to iron on the Hb heme group 250 times more
strongly than O2 - CO poisoning
- Treat by administering pure O2
53
CO2 Transport
- 7 dissolves in plasma
- 23 becomes Hb-CO2 carbaminohemoglobin
- 70 converted to bicarbonate (HCO3- and most
bicarbonate transported in plasma as sodium
bicarbonate
70 Converted to bicarbonate
54
Control of Ventilation
- Medullary rhythmicity Neurons in the Medulla
Oblongata - Inspiratory Area
- Controls basic rhythm of respiration
- Inspiration for 2 seconds, expiration for 3
- Autorhythmic cells active for 2 seconds then
inactive - Expiratory Area
- Inactive during most quiet breathing only active
during forced ventilation
55
Control of Ventilation
- Neurons in the Pons coordinate transition between
inhalation and exhalation - Apneustic area stimulates inhalation resulting in
prolonged inhalation - Pneumotaxic area inhibits inspiration before
lungs can become over-inflated
56
Respiratory Centers
57
Factors Affecting Breathing
- (1) CO2
- Hypercapnia (increase in CO2) excites
chemoreceptors in carotid arteries, aorta and
medulla oblongata and breathing rate increases - (2) O2
- Hypoxia (decrease in O2) such as at high altitude
causes imcreased breathing rate
58
Factors Affecting Breathing
- (3) Proprioceptors
- Muscle contraction and joint movement increase
during exercise - Increased stimulation of proprioceptors quickly
increases breathing rate - Happens as soon as you start to exercise
59
Factors Affecting Breathing
- (4) Inflation (Hering-Breuer) Reflex
- As lungs over-inflate, stretch receptors become
excited - Increase in nerve impulses to pons and medulla
inhibits apneustic and inspiratory area - Inhalation stops before lungs can be damaged
- (5) Conscious Control Intentional breathing
60
Clinical Terms
- Apnea No breathing
- Hyperventilation Rapid breathing
- Hypoventilation Slow breathing
- Orthopnea Labored breathing when lying
- down flat and is relieved by sitting up.
61
Clinical Terms
- Dyspnea painful breathing
- Chronic obstructive pulmonary diseases (COPD's)
- Emphysema
- Chronic bronchitis
62
Clinical Terms
- Tuberculosis
- Pneumonia
- Lung cancer