RESPIRATORY PHYSIOLOGY (HUMAN PHYSIOLOGY I) Dr. Waheeb Alharbi - PowerPoint PPT Presentation
1 / 28
Title:
RESPIRATORY PHYSIOLOGY (HUMAN PHYSIOLOGY I) Dr. Waheeb Alharbi
Description:
RESPIRATORY PHYSIOLOGY (HUMAN PHYSIOLOGY I) Dr. Waheeb Alharbi References (1) Physiological basis of medical practice. By; John B. West (2) Concise Human ... – PowerPoint PPT presentation
Number of Views:5096
Avg rating:3.0/5.0
Title: RESPIRATORY PHYSIOLOGY (HUMAN PHYSIOLOGY I) Dr. Waheeb Alharbi
1
RESPIRATORY PHYSIOLOGY(HUMAN
PHYSIOLOGY I)Dr. Waheeb Alharbi
2
References
- (1) Physiological basis of medical practice.
- By John B. West
- (2) Concise Human Physiology
- By M. Y. Sukkar, H. A. El-Munshid
- M. S. m. Ardawi
- (3) Human physiology
- ByGuyton
3
Lecture 1
- Ventilation
- Gas transport
- Tissue respiration
- Functional anatomy of the respiratory system
- Basic mechanism of VE
- Lung volume and capacities
- Dead space
- Alveolar VE
- VD and uneven VE
4
- Resp is the use of O2 by the living cell for
oxidation of nutrients. This result in production
of CO2. - It can be divided into 4 main events
- 1) pulmonary VE
- 2) gas diffusion
- 3) gas transport
- 4) regulation of resp
- VE is the movement of air between the environment
and the alveoli. It can be spontaneous or
artificial. - Air is a mixture of gases. According to Daltons
Law, the total pres of a mixture of gases is the
sum of the pres of the individual gases (Ptotal
P1 P2 P3 ).I.e. partial pressure. - VE fr X VT
5
Gas transport
- Most gases transported in the blood in 2 forms
- 1- Dissolved in the plasma
- 2- Combine with Hb
- Under normal circumstances, more than 98 of the
O2 in a given vol of blood is transported in
RBCs, bound to Hb.
6
Tissue resp
- It means getting energy out of glucose.
- The most efficient form of resp is aerobic
(require O2) and anaerobic resp (does not require
O2). - Aerobic resp It is the normal process by which
food substances are broken down and oxidized to
provide energy. - Glucose O2 ? CO2 H2O energy
released - Anaerobic resp It means that energy can be
derived from food substances without the
simultaneous utilization of O2. - Glucose ? lactic acid much less energy
released
7
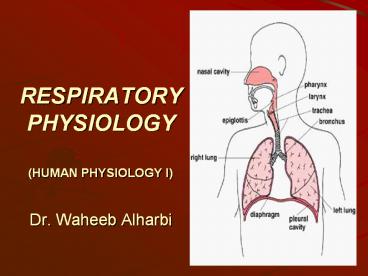
Functional anatomy of the resp system
- Anatomy of the resp system is composed of
- 1) the resp air ways
- 2) the lungs
- 3) the resp muscles
- 4) the neural centers
- The main function of the lungs is to provide
continuous gas exchange between inspired air and
blood in the pulmonary circulation, supplying O2
and removing CO2, which is then cleared from the
lungs by subsequent expir. - The functional structure of the lung can be
divided into - 1- The Conducting zone, and
- 2- The respiratory zone.
- The Conducting zone (air flow) Air comes into
the nose and the mouth through the pharynx,
larynx and then through the trachea. - The respiratory zone (gas diffusion) It begins
when alveoli start to appear in the walls of the
bronchioles.
8
(No Transcript)
9
(No Transcript)
10
(No Transcript)
11
(No Transcript)
12
(No Transcript)
13
Basic mechanism of vent
- Breathing consists of 2 phases inspiration
(active process) and expiration (passive
process). - During inspir The diaphragm and intercostals
muscles contract. The diaphragm moves downwards
increasing the vol of the thoracic cavity, and
the intercostals muscles pulls the ribs up
expanding the rib cage and further ? this vol. - During expir The diaphragm and intercostals
muscles relax. This returns the thoracic cavity
to its original vol, ? the air pressure in the
lungs, and forcing the air out.
14
(No Transcript)
15
- Pleural pressure It is the pres in the narrow
space between the lung pleura and chest wall
pleura. - Alveolar pressure It is the pres inside the lung
alv.
16
(No Transcript)
17
(No Transcript)
18
Lung volumes and capacities
- Capacity is the sum of 2 or more vols.
- Lung vol and capacity can be measured by a
spirometer. It also can be measured by
vitalograph, gas dilution and body
plethysmography. - Lung vol includes
- 1) Tidal volume (VT) It is the vol of air
expired and inspired in each breath (500 ml). - 2) Inspiratory reserve volume (IRV) It is the
max vol of additional air that can be inspired
from the end of a normal insp (3100 ml). - 3) Expiratory reserve volume (ERV) It is the
max vol of additional air that can be expired
from the end of a normal exp (1200 ml). - 4) Residual volume (RV) It is the vol of air
that remains in the lung after maximal exp (1200
ml). - Lung capacities include
- 1) Inspiratory capacity (IC) VT IRV.
- 2) Functional residual capacity (FRC) ERV RV.
- 3) Vital capacity (VC) IC ERV.
- 4) Total lung capacity (TLC) IC FRC.
19
Spirometer
20
(No Transcript)
21
Normal values of lung vol and capacities in both
male female
22
LUNG CAPACITIES AND RESP DISEASES
- A) Restrictive Disease. Resp disease which make
it more difficult to get air in to the lungs.
They restrict inspiration. Includes fibrosis,
sarcoidosis, muscular diseases, and chestwall
deformities. - B) Obstructive Disease. Resp disease which make
it more difficult to get air out of the lungs.
Includes emphysema, chronic bronchitis, asthma. - C) A summary of lung capacity changes during
disease such as follow - Restrictive Disease ? VC ? TLC, ? RV, ? FRC.
- Obstructive Disease ? VC ? TLC, ? RV, ? FRC.
23
(No Transcript)
24
Anatomical and physiological VD
- VD is defined as the vol of inspired air that
does not participate in GE. - The normal VD in a young adult man is about 150
milliliters. This ? slightly with age. - There are two types of VD anatomical and
physiological. - (1) Anatomic VD is the vol of an inspired
breath which has not mixed with the gas in the
alv. It is anatomical because it measures the
anatomical vol of the conducting airways leading
up to the alv. It can be measured from the vol of
expired gas leaving the mouth and nose before the
'front' of alveolar gas containing CO2 arrives at
the lips. - (2) Physiological VD is the vol of an inspired
breath which has not taken part in GE. It is
physiological because it assesses one of the
functions of the lungs (GE). It can be estimated
using the Bohr equation, which is derived from
the fact that the vol of gas expired equals the
vol from the VD plus the vol from the alv.
25
- In a normal person, the anatomic and physiologic
VD are nearly equal because all alv are
functional in the normal lung, but in a person
with partially function or nonfunctional alv in
some parts of the lungs, the physiologic VD may
be as much as 10 times the vol of anatomic VD.
26
VA
- VA is the total vol of new air entering the alv
and adjacent GE area each minute. - It is equal to the resp frequency times the
amount of new air that enters these area with
each breath - VA fr X (VT- VD)
- What is the VA in a normal person?
- VA . X (. - .) ml/min
- Because of the VD, rapid, shallow resp produces
much less VA than slow, deep resp at the same
minute vol (see table).
27
Table Effects of variations in respiratory rate
depth on VA.
28
VD and uneven VE
- In the upright subject the bases of the lungs are
found to be better ventilated than the apices.
This can be demonstrated by breathing radioactive
xenon. - The uneven VE is due to the effect of gravity.
Similarly, a subject in the supine position will
have better VE of the posterior parts of the
lungs than the anterior parts. Uneven VE can
significantly affect gas exchange in the lungs. - VE is preferentially distributed to the more
dependent portions of the lungs because, as a
result of the weight of the lungs, the
intrapleural pres is lower (i.e. less negative). - A clinical correlate of the effect of gravity on
VE is that arterial oxygenation is improved in
unilateral lung diseases when patients lie on
their sides so that the good lung is in the
dependent position.