Respiratory system - PowerPoint PPT Presentation
1 / 38
Title:
Respiratory system
Description:
Respiratory system What is respiration? Multiple definitions Ventilation of lungs (breathing) Exchange of gases between air and blood Also between blood and tissues ... – PowerPoint PPT presentation
Number of Views:216
Avg rating:3.0/5.0
Title: Respiratory system
1
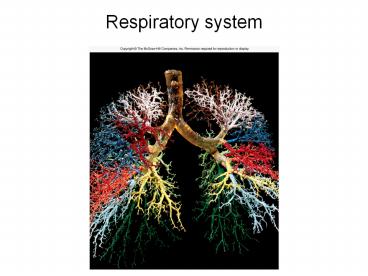
Respiratory system
2
What is respiration?
- Multiple definitions
- Ventilation of lungs (breathing)
- Exchange of gases between air and blood
- Also between blood and tissues
- Oxygen consumption during metabolic activities
- Happens in what organelle?
3
What organs are involved?
- Conducting regions
- Nose
- Larynx
- Epiglottis
- Trachea
- Bronchi
- Lungs
- Bronchioles
- Respiratory region
- Alveoli
- Upper respiratory
- Head and neck
- Lower respiratory
- Trachea to lungs
4
What does the nose do?
- Receive and humidify incoming air
- Smells
- Voice resonating chamber
- Filter out bacteria
5
Why do I only breath out of one chamber at a time?
- Nasal fossa chamber
- Divided by nasal septum
- Lamina propria of inferior concha swell
- Every 30-60 minutes
- Alternate chambers
- Allows for rehydration
- Epistaxis
- Nose bleed most common in inferior concha
6
Whats up with the pharynx and larynx?
- Pharynx extends from nose/mouth to larynx
- Good at trapping large dust particles
- Larynx voice box
- Job keep food/water out of trachea
- Also produces sound
- Glottis (opening) guarded by epiglottis
7
What does the trachea do?
- Hyaline cartilage rings stiffen tube
- Directs air to lungs via bronchi
- Pseudostratified epithelium
- Mucociliary escalator cilia sweep mucus upward
to pharynx
8
What parts make up the lungs?
- Right lung superior, middle, inferior lobes
- Left lung superior and inferior lobes only
- Bronchial tree
- Branched air tubes from primary bronchi (two) to
secondary bronchi to tertiary bronchi to
bronchioles - Overlapping plates of cartilage give shape
9
What parts make up the lungs?
- Bronchioles (no cartilage) have smooth muscle to
dilate/contract - Asthma
- Bronchiolconstriction (irritants, cold air,
histamine) and bronchioldilation - Click below for asthma movie!
10
What parts make up the lungs?
- Terminal bronchioles follow after bronchioles
- Final branches of conducting division (region)
- Cilia prevent congestion via mucociliary
escalator - Next are respiratory bronchioles
- Beginning of respiratory division
- Divide into alveolar ducts
- End in alveolar sacs
11
What do the alveoli do?
- Approx. 150 million great S.A.
- Mostly squamous alveolar cellswhy?
- A few cuboidal cells (great alveolar cells)
- Secrete pulmonary surfactant
- Disrupts hydrogen bonds
- Prevents alveolar collapse during expiration
- Premature infants lack
12
What do the alveoli do?
- Alveolar macrophages consume anything mucus
doesnt strain out - Items smaller than 2 micrometers
- Capillaries surround each alveolus
- Distance air must travel
- Called respiratory membrane
- Squamous alveolar cell, basement membrane,
capillary squamous cell
13
What are the pleurae and why are they there?
- Moist serous membrane covering outside of lungs
- Visceral pleura inside
- Folds out at hillum to form outer parietal pleura
- Pleural cavity between parietal and visceral
layers - Filled with pleural (serous) fluid
- Pleurae functions
- Reduce friction
- Create pressure gradient to help with lung
inflation - Compartmentalization prevent infection spread to
neighboring organs
14
How does breathing occur?
- Atmospheric pressure drives respiration
- Atm. pressure weight of air column
- 1 atm. 760 mmHg
- Boyles law pressure and volume are inversely
proportional - Intrapulmonary pressure changes opposite to
volume load - Lower intrapulmonary pressure below 760 mmHg to
draw breath
15
What happens during inspiration?
- Diaphragm does most of the work
- Phrenic nerves cause diaphragm to flatten
- External intercostals also contract, elevating
(expanding) ribcage - Increases lung volume so pressure ______
- Parietal pleurae cling to external intercostals
- Visceral pleurae cling to parietal pleurae
- Helps increase volume
16
What happens during inspiration?
- Air is warmed to assist volume expansion
- 500 ml air inhaled during resting inspiration
- 150 ml is dead air (held in conducting regions)
- Thus only 350 ml to alveoli (respiratory
division) - Alveolar ventilation rate (AVR) 350 ml (or
whatever value) X number of breath per minute
17
What happens during expiration?
- Passive process
- Diaphragm and external intercostals allowed to
relax - Natural elasticity of ribcage, lungs and tendons
assist via recoil - Boyles law volume decreases so pressure
___________ and air ______ - Hard exhale use internal intercostals to depress
ribcage
18
Why does a lung collapse?
From http//www.lunge.no/files/news/pneumothorax.
gif
- Pneumothorax air in the pleural cavity
- Can happen if thoracic wall is punctured
- Separates visceral and parietal pleurae
- Result? Lung collapse atelectasis
- Can also happen if area of lung is blocked
- Blood absorbs air and lung collapses
From http//medinfo.ufl.edu/bms5191/pulmon2/imag
es/1a.jpg
19
How is ventilation measured?
- Spirometer
- Measures respiratory volumes
- Tidal volume amount of air inhaled or exhaled
when relaxed - Inspiratory reserve volume amount can breath in
above tidal volume with maximum effort - Expiratory reserve volume
- Residual volume what remains in lungs after
maximum expiration (keeps alveoli inflated)
20
What are some breathing variations?
- Apnea temporary breath cessation
- Dyspnea gasping, labored breathing, shortness of
breath - Orthopnea dyspnea while lying down
- Eupnea normal, quiet breathing
- Hyperpnea increased rate and depth of breathing
- Tachypnea accelerated respiration
- Hyperventilation expels too much CO2, raising pH
- Hypoventilation increases CO2, lower pH
21
What controls breathing?
- Medulla oblongata
- Inspiratory neurons
- Expiratory neurons (dont fire during eupnea)
- Unknown how rate of breathing is set
- Pons
- Regulates ventilation via pneumotaxic center
- Sends inhibitory signals to med. Obl. inspiratory
center - More impulses shorter breath
- Voluntary control motor cortex of frontal lobe
- Automatic controls can override to protect
organism
22
What happens during gas exchange?
- Air composition O2, N2, H2O, CO2
- Daltons law partial pressure of each adds up to
total pressure - What should they add up to at sea level?
23
What affects gas exchange?
- Takes about 0.25 secs to create equilibrium
- Erythrocyte takes 0.75 sec to pass through
alveolar cap. - During exercise erythrocyte present for 0.3 sec
24
What affects gas exchange?
- Concentration gradients of gases
- Blood entering lungs
- PO2 40 mmHg
- PCO2 46 mmHg
- Blood leaving lungs
- PO2 95 mmHg
- PCO2 40 mmHg
- Solubility Same amount of gases exchange,
though, bec. CO2 is about 20 times as soluble in
water
25
What affects gas exchange?
- Membrane thickness respiratory membrane v. thin
- Left ventricular failure edema and thickened
resp. memb. - Result gases cant equilibrate fast enough
- Membrane area more resp. memb. S.A. better gas
exchange - Emphysema, tuberculosis decrease S.A.
26
How is oxygen transported?
- Oxygen 98 bound to hemoglobin
- Review hemoglobin structure
- How many molecules of oxygen can one hemoglobin
hold? - As more oxygen bind to hemoglobin, affinity for
oxygen increases - Oxyhemoglobin vs. deoxyhemoglobin
- CO poisoning carboxyhemoglobin (HbCO) competes
with oxygen for binding site - Binds 210 times more tightly than oxygen to heme
group
27
How is carbon dioxide transported?
- Three ways
- Carbonic acid
- 70 of CO2 is hydrated
- CO2 H2O ? H2CO3 ? HCO3- H
- Carbamino compounds (23)
- To plasma proteins and hemoglobin to form
carboaminohemoglobinHbCO2 (different from
carboxyhemoglobin) - Binds to polypeptides, not to heme groups
- Dissolved gas (7)
- Dissolves in plasma like CO2 in soda pop
28
What is carbon dioxide loading?
- Carbonic acid reaction occurs in plasma and
erythrocytes - Carbonic anhydrase in RBCs speeds reaction
- Chloride shift HCO3 diffuse out of RBCs,
replaced with Cl- - H binds to Hb (this buffers RBC pH)
29
What is oxygen unloading?
- H bound to HBO2 decreases affinity for O2
- Causes RBC to offload oxygen more easily
- Under what conditions would this happen?
- Venous reserve oxygen not offloaded
- Can sustain life for up to five minutes
30
What happens in exhalation?
- Carbon dioxide offloading
- Exact reverse of loading process
- Oxygen loading
- Reverse of offloading
31
Does Hb always offload the same amount of O2?
- No!
- If PO2 of tissue is lower, more is offloaded
- Higher temp more offloaded
- Bohr effect active tissues put off more CO2
which lowers blood pH - This causes more O2 offloading Bohr effect
- BPG (bisphosphoglycerate) binds to Hb and
promotes O2 offloading - RBS anaerobic fermentation intermediate
- Fever, growth hormone, NE stimulate BPG synthesis
32
Does Hb always load the same amount of CO2?
- No!
- Haldane effect low HbO2 allows more CO2
transport - HbO2 doesnt bind CO2 as well as deoxyhemoglobin
(HHb) - HHb binds more H which removes H from solution
- How does this affect the reaction CO2 H2O ?
H2CO3 ? HCO3- H?
33
How does blood chemistry affect ventilation?
- Peripheral chemoreceptors monitor
- Carotid bodies and aortic bodies
- Central chemoreceptors also monitor
- In brainstem
- Both monitor blood pH
- How does this relate to O2 and CO2 levels?
34
How does blood chemistry affect ventilation?
Recall CO2 H2O ? H2CO3 ? HCO3- H
- H in CSF is main site of monitoring
- H doesnt cross blood-brain barrier but CO2
does, then reacts with water - Problem few proteins present to buffer H
- Acidosis blood pH lower than 7.35
- Common cause hypercapnia (high CO2 value)
- To correct blow off CO2 rapidly
(hyperventilation) - Alkalosis above 7.45
- Common cause hypocapnia
- To correct take up CO2 rapidly (hypoventilation)
35
How does blood chemistry affect ventilation?
- Ketoacidosis from diabetes mellitus
- Lipid oxidation produces ketone bodies
- Leads to low pH
- Hyperventilation called Kussmaul respiration
- Blowing off CO2 helps remove H and compensate
for ketone body H production
36
What are some respiratory disorders?
- Hypoxia oxygen deficiency
- Hypoxemic hypoxia low arterial PO2
- High altitude, impaired pulmonary function,
respiratory arrest, lung disease - Ischemic hypoxia inadequate blood circulation
- e.g. from congestive heart failure
- Anemic hypoxia from anemia
- Histotoxic hypoxia from metabolic poison (e.g.
cyanide) - Hyperoxia produces hydrogen peroxide and free
radicals
37
What are some respiratory disorders?
- Chronic obstructive pulmonary disease (COPD)
- Long-term obstruction of airflow
- Asthma
- Chronic bronchitis cilia immobilized and reduced
in number - More goblet cells present produces sputum
- Emphysema alveolar walls destroyed
- Smokers often have one or more of these
38
How does smoking and cancer affect the lungs?
- Lung cancer accounts for the most cancer-related
deaths - Causes smoking, followed by pollution
- Tobacco more than 15 carcinogens
From http//www.aafp.org/afp/991201ap/photo.html