The Pancreas - PowerPoint PPT Presentation
1 / 76
Title:
The Pancreas
Description:
no distinction between primary and secondary causes of diabetes. ... Symptoms of diabetes plus a random plasma glucose concentration 200 mg/dL (11.1 ... – PowerPoint PPT presentation
Number of Views:593
Avg rating:3.0/5.0
Title: The Pancreas
1
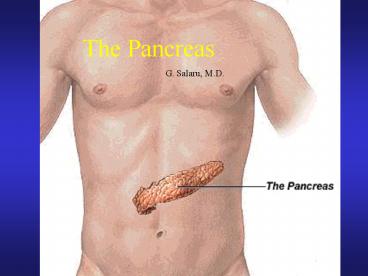
The Pancreas
G.
Salaru, M.D.
2
(No Transcript)
3
(No Transcript)
4
(No Transcript)
5
Congenital anomalies
- Agenesis
- Hypoplasia
- Pancreas divisum
- Annular pancreas
- Ectopic pancreas
6
(No Transcript)
7
(No Transcript)
8
The Pancreas
- Endocrine pancreas
- Diabetes Mellitus (DM)
- Islet Cell Tumors
- Exocrine pancreas
- Acute pancreatitis
- Chronic pancreatitis
- Carcinoma of the pancreas
9
Endocrine Pancreas
- 1 million microscopic units the islets of
Langerhans - 4 most important cell types of the islets are
- ? (beta) constitute 70 of the cells and contain
insulin - A (alpha) 20 of the cells and elaborate
glucagon - D (delta) secrets somatostatin which suppresses
the insulin and glucagon secretion - PP (pancreatic polypeptide) unknown physiologic
function
10
(No Transcript)
11
Diabetes Mellitus
- several syndromes of abnormal carbohydrate
metabolism hyperglycemia. - relative or absolute impairment in insulin
secretion, along with varying degrees of
peripheral resistance to the action of insulin. - no distinction between primary and secondary
causes of diabetes. - attempt to classify DM according to the etiologic
differences and to move away from the description
based on age of onset or type of treatment.
12
Etiologic classification of DM
- Type 1 DM Beta-cell destruction that usually
leads to absolute insulin deficiency - Immune-mediated
- Idiopathic
- Type 2 DM predominantly insulin-resistant with
relative insulin deficiency to a predominantly
secretory defect with insulin resistance - Gestational DM
- Other specific types
13
Other Specific Types
- Genetic defects of beta cell function
- Genetic defects involving insulin action
- Diseases of exocrine pancreas (pancreatitis,
trauma, neoplasia, CF etc.) - Endocrinopathies ( Cushings, acromegaly,
pheochromocytoma, hyperthyroidism etc.) - Drug-or chemical-induced (glucocorticoids,
thiazide diuretics, nicotinic acid, pentamidine,
etc.) - Infection-related (congenital rubella, CMV, etc.)
- Other genetic syndromes associated with diabetes
(Turner, Klinefelter, Down, etc.)
14
- Although the 2 major types of diabetes have
different pathogenic mechanisms and metabolic
characteristics, the long-term complications are
the major causes of morbidity and death from
diabetes. - These complications include
- Coronary heart disease which can lead to heart
attacks - Retinopathy which can lead to blindness
- Nephropathy which can lead to kidney failure and
the need for dialysis - Neuropathy which can lead to, among other
complications, foot gangrene requiring
amputation.
15
Incidence of DM
- In the US, more than 15.4 million persons have
DM, but only 60 of them have been diagnosed. - The annual mortality rate is about 54,000.
- In 1998, the cost of diabetes to the medical care
system in the US was 104 billion, a figure that
has been increasing yearly by 10-12. - It is the 7th leading cause of death in the US.
16
Criteria for the Diagnosis of DM
- Symptoms of diabetes plus a random plasma glucose
concentration gt200 mg/dL (11.1 mmol/L). - Fasting plasma glucose concentration gt126 mg/dL
(7.0 mmol/dL) - 2-hour plasma glucose concentration gt200 mg/dL (
11.1 mmol/dL)during an oral glucose tolerance
test.
17
Normal Insulin Metabolism
- Insulin is a peptide hormone composed of 51
aminoacids that is synthesized, packaged and
secreted in the pancreatic beta cells. - The major regulator of insulin secretion is
glucose which acts both directly and by
augmenting the action of other insulin
secretagogues. - A rise in the blood glucose levels, causes an
immediate release of insulin, presumably that is
stored in the beta-cell granules. If the
secretory stimulus persists, a delayed response
follows, which involves active synthesis of
insulin from the beta-cells. - Other agents, including intestinal hormones and
certain aminoacids (leucine and arginine), as
well as sulfonylureas, stimulate insulin release.
18
Functions of Insulin
- Insulin is a major anabolic hormone. It is
necessary for - Transmembrane transport of glucose and aminoacids
- Glycogen formation in the liver and skeletal
muscles - Glucose conversion to triglycerides
- Nucleic acid synthesis
- Protein synthesis
- Its principal metabolic function is to increase
the rate of glucose transport into certain cells
in the body. These are the striated muscle cells,
including myocardial cells, fibroblasts, and fat
cells, representing collectively about 2/3 of the
entire bodyweight.
19
Pathogenesis of type 1 DM
- This form of diabetes results from a severe,
absolute lack of insulin caused by a reduction in
the beta cell mass. - It usually develops in childhood, becoming
manifest and severe at puberty. - Patients depend on insulin for survival.Without
insulin, they develop serious metabolic
complications such as acute ketoacidosis and
coma. - Ketoacidosis may also be the first manifestation
of diabetes in young patients. - Three interlocking mechanisms are responsible for
the islet cell destruction - Genetic susceptibility
- Autoimmunity
- Environmental factors
20
Genetic susceptibility
- The precise mode of inheritance of the
susceptibility genes for type 1 DM remains
unknown. - 50 concordance rate among monozygotic twins.
- Only 5-10 of the children of first-degree
relatives with type 1 DM develop the disease. - Therefore,environmental factors must play an
important role in this type of diabetes.
21
- At least one of the susceptibility genes for type
1 DM resides in the region that encodes the class
II antigens of the major histocompatibility
complex on chromosome 6 (HLA-D) - About 95 of caucasian patients with type 1 DM
have either HLA-DR3 or HLA-DR4 alleles or both,
whereas in the general population the prevalence
of these antigens is only 40. - HLA-DR3 5x greater risk of developing diabetes
- HLA-DR4 7x
- HLA-DR3/DR4 14.3x
22
Autoimmunity
- A role for autoimmunity in the pathogenesis of
diabetes is supported by several morphologic,
clinical, and experimental observations - Lymphocytic infiltrate (insulitis) in the islets
in cases of recent onset. Both CD4 and CD8 T
cells are found within such infiltrates.
Furthermore, CD4 T cells from diseased animals
can transfer diabetes to normal animals, thus
establishing the primacy of T-cell autoimmunity
in type 1 DM. - Type 1 DM results from cell-mediated autoimmune
destruction of the beta cells of the pancreatic
islets.Circulatory markers of this destruction
are autoantibodies to insulin, islet cells,
glutamic acid decarboxylase (GAD), and several
tyrosine phosphatases.One or more antibodies are
present in 85-90 of newly diagnosed patients
with type 1 disease.
23
- In experimental animals and humans the insulitis
is associated with expression of class II major
hystocompatibility complex (MHC) molecules on
beta cells. - Type 1 patients (aprox.10) are prone to other
autoimmune disorders such as Graves disease,
Hashimotos thyroiditis, Addisons disease, and
pernicious anemia.
24
Environmental factors
- Although no definite environmental agent has been
identified, viruses are suspected as initiators
of the disease. - The viral infections implicated include
- Mumps
- Measles
- Rubella
- Coxsackie B
- Epstein-Barr (infectious mononucleosis)
- The most likely scenario is that viruses cause
mild beta cell injury, which is followed by an
autoimmune reaction against altered beta cells in
persons with HLA-linked susceptibility.
25
Pathogenesis of type 2 DM
- More than 80 of patients with diabetes in the US
have type 2 disease which has a strong genetic
base, as concordance rate among monozygotic twins
is almost 100. - There are 2 main defects in patients with type 2
DM - Insufficient insulin secretion (relative to the
glucose load) - Increased insulin resistance(inability of
peripheral tissues to respond to insulin) - Obesity increases insulin resistance and about
80 of patients with type 2 DM are obese (weight
loss can improve the diabetic condition). - Most patients with type 2 disease have a relative
or absolute deficiency of insulin, which is
milder than that of type 1, and not an early
feature of this variant of diabetes.
26
Pathogenesis of the Complications of Diabetes
- microvascular complications usually appear 10-15
years after the onset of DM retinopathy,
nephropathy, and neuropathy. - The Diabetes Control and Complication Trial
(DCCT) reported 30-50 decreased risk of
development of microvascular complications with
strict diabetic control. NEJM.1993329977.(previo
usly it was thought that tight control did not
have much effect on these complications.) - Most of the available evidence suggests that the
complications of DM are a consequence of the
metabolic derangements, especially hyperglycemia. - 2 mechanisms are considered important
- Nonenzymatic glycosilation
- Intracellular hyperglycemia with disturbance in
the polyol pathways
27
Nonenzymatic Glycosilation
- glucose attaches to the amino group of proteins
without the aid of enzymes. - nonenzymatic glycosylation of hemoglobin A (HbA)
leads to the formation of HbA1c, which normally
constitutes about 4 of hemoglobin in the red
blood cells. - HbA1c level provides an index of the average
blood glucose level over the preceding 2-4
months. - The results of DCCT trial indicate that a HbA1c
value in the 7.2 8.0 range (blood glucose
concentration of 155 mg/dL) significantly reduces
the appearance and progression of microvascular
complications.
28
- excessive glycosylation advanced glycosylation
products (AGEs) - serum albumin, collagen, basic myelin protein,
and low-density lipoproteins (LDLs). - AGEs attached to collagen in blood vessel walls
irreversibly cross-link to plasma proteins, e.g.
LDLs. - cross-linking retards the normal efflux of LDLs
that have entered the vessel wall and enhances
deposition of cholesterol in the intima and
accelerates the development of atherosclerosis.
29
Intracellular Hyperglycemia with Disturbance in
the Polyol Pathways
- In nerves, lens, kidney and blood vessels,
hyperglycemia leads to increase in intracellular
glucose (do not require insulin for glucose
transport) - polyol pathway - glucose is reduced to sorbitol
by the enzyme aldol reductase and then fructose. - Sorbitol tissue toxin,and has been implicated
in the pathogenesis of diabetic complications.
Sorbitol decreases phosphoinositide metabolism
and signal transduction. - Aldol reductase inhibition also has been shown to
prevent experimental cataracts and retinopathy.
30
- In the past it has been common to attribute
- microvascular complications (retinopathy,
nephropathy, neuropathy) to the polyol pathway - macrovascular complications (stroke, gangrene,
myocardial infarction) to glycation and AGEs. - However both pathways contribute to both sets of
complications.
31
Metabolic derangements
- Insulin major anabolic hormone glucose, lipid
and protein metabolism. - type 1 DM marked deficiency
- stimulation of glycogenolysis, which is normally
inhibited by insulin and favored by glucagon.
Fasting blood glucose may reach levels many times
greater than normal - exceeds the renal threshold glycosuria
- glycosuria induces an osmotic diuresis and thus
polyuria, causing a profound loss of water and
electrolytes.
32
- water loss AND hyperosmolarity depleted
intracellular water in the osmoreceptors of the
thirst in the brain intense thirst
(polydipsia). - Through poorly defined pathways, increased
appetite (polyphagia) develops, thus completing
the classic triad of diabetic findings
polyuria, polydipsia, and polyphagia. - With a deficiency of insulin, the scales swing
from insulin-promoted anabolism to catabolism of
proteins and fat. - Two important acute metabolic complications of
diabetes are ketoacidosis, and non-ketotic
hyperosmolar coma.
33
(No Transcript)
34
Morphology of Diabetes
- Three important factors in morphologic changes of
diabetes are - The duration of the disease
- The adequacy of metabolic control
- Genetic factors
35
Basement Membrane Changes
- Thickening of the BM (BMT) is characteristic of
DM. - capillaries microangiopathy
- Skin
- skeletal muscle
- Retina
- renal glomeruli
- renal medulla.
- BMT in nonvascular structures - renal tubules,
Bowmans capsule, peripheral nerves, placenta and
possibly other sites. - single layer BM replaced by concentric layers of
hyaline material (type IV collagen). - increased thickness BMT but more leaky than
normal to plasma proteins.
36
Anatomic changes in the pancreatic islets
- Type 1 DM
- Islets are small and beta cells are markedly
decreased in number or are absent - insulitis - lymphocytic infiltration is highly
specific for this form of diabetes. - Type 2 DM
- islet fibrosis and hyalinization (due to
deposition of amylin) are characteristic but not
specific. - Amylin (also known as islet amyloid polypeptide,
IAPP) is characteristic of type 2 DM and is
thought to interfere either with the conversion
of proinsulin to insulin or with sensing of
insulin by beta cells.
37
Circulatory changes
- In the course of 10-15 years of the disease, most
diabetics develop significant vascular
abnormalities. - Atherosclerosis is more extensive and occurs
earlier than in general population. - Coronary artery disease (CAD) accounts for more
than half of deaths in diabetics. Women with
diabetes have a risk of cardiovascular death that
is up to 7.5x that of aged-matched nondiabetic
women. Silent myocardial ischemia is more common
in diabetic patients than in general population. - Peripheral deposits may cause intermittent
claudication, gangrene, and, in men, organic
impotence on a vascular basis. - Surgical repair of large-vessel lesions may be
unsuccessful because of the simultaneous presence
of widespread disease of the small vessels.
38
Presumed Reasons for Accelerated Atherosclerosis
- Elevated blood lipid levels.
- Qualitative changes in the lipoproteins (low
levels of HDL, while LDL levels are high-normal
or high). The atherosclerotic lesion appears to
be initiated by oxidized LDL (not native LDL). - Increased platelet adhesiveness to the vessel
wall (enhanced thromboxane A2 synthesis and
decreased prostacyclin). - Increased secretion of endothelin-1 and
diminished production of nitric oxide (in vitro). - Increased incidence of hypertension in diabetics.
39
Kidneys
- The kidneys are prime targets of DM. Renal
failure is second only to myocardial infarction
as a cause of death from this disease. About half
of the cases of end stage renal disease in the US
are now due to diabetic nephropathy. - Diffuse glomerulosclerosis, nodular
glomerulosclerosis (Kimmelstiel-Wilson),
arteriolosclerosis, exudative lesions such as
fibrin cap or drops in Bowmans capsule,
occlusion of the glomeruli are renal
manifestations of diabetes. Deposition of albumin
and other proteins occurs in both glomeruli and
tubules. - Pyelonephritis is a frequent complication that
may be compounded by renal papillary necrosis. - The most specific lesions of diabetic
glomerulosclerosis are hyalinization of afferent
glomerular arterioles and the Kimmelstiel-Wilson
nodules.
40
Eyes
- The ocular involvement in diabetes are
- Retinopathy
- Cataract
- Glaucoma
- Diabetic retinopathy (retinal exudates, edema,
hemorrhages, and microaneurysms of small vessels)
is the leading cause of new blindness among
adults. It correlates with duration and control
of DM. - Retinopathy begins to occur 3-5 years after
diagnosis in patients with type 1 DM, and within
15-20 years of having the disease almost all
patients have some retinopathy. After 20 years of
type 2 DM, 50-80 of patients have retinopathy.
41
Nervous System
- The central and peripheral nervous systems are
not spared in diabetes. - The most frequent pattern of involvement is a
peripheral, symmetric polyneuropathy of the lower
extremities, that affects both motor and sensory
function but particularly the latter (symptomatic
paraesthesias of pins and needles). - Other forms include
- Autonomic neuropathy (gastroparesis, erectile
dysfunction) - Diabetic mononeuropathy usually affects the
third and sixth cranial nerves, the peroneal
nerve (foot drop), and the radial nerve (wrist
drop) - Cerebral vascular infarct and hemorrhages
- Degenerative changes of the spinal cord
42
Changes in other organs
- Fatty changes of the liver
- Glycogen vacuolation in the nuclei of the hepatic
cells - Degenerative changes of striated muscles
- Skin
- Xanthomas (collections of lipid-laden macrophages
in the dermis) - Furuncles and abscesses because of increased
propensity to infection frequent fungal
infections, especially with Candida albicans
43
Type 1 DM - clinical correlation
- Begins by age 20 in most patients
- Signs and symptoms are polyuria, polydipsia,
polyphagia, weight loss, muscle weakness. - Ketoacidosis may be the first manifestation in
young patients with diabetes. - Plasma insulin is low or absent, and glucagon
level is increased. - Blood glucose level is quite sensitive to
administered exogenous insulin, deviations from
normal dietary intake, unusual physical activity,
infection or other forms of stress.Inadequate
fluid intake or vomiting may rapidly lead to
significant disturbances in fluid and electrolyte
balance. - Thus , these patients are vulnerable on one hand
to hypoglycemic episodes and on the other hand to
ketoacidosis.
44
Type 2 DM clinical correlation
- Patients are often older (gt40 years) and
frequently obese. - The disorder is often part of a complex metabolic
syndrome (syndrome X), that constitutes a major
risk for cardiovascular disease. Obesity,
dyslipidemia, hypertension and clotting
abnormalities are other components of the
syndrome. - May also present with polyuria and polydipsia in
some cases unexplained weakness or weight loss. - Very often, however, the diagnosis is made by
routine blood or urine testing in asymptomatic
persons. - The metabolic derangements are usually
controllable and less severe. - In the decompensated state they develop
hyperosmolar nonketotic coma.
45
Characteristics DM 1 DM 2
46
Characteristics DM1 DM2
47
(No Transcript)
48
(No Transcript)
49
Islet Cell Tumors
- Tumors of the pancreatic islets are rare in
comparison with tumors of the exocrine pancreas. - They may be hormonally functional or
non-functional, single or multiple, benign or
malignant. - The most common are
- Insulinoma (beta cell tumor)
- Gastrinoma (Zollinger-Ellison syndrome)
- Glucagonoma (alpha cell tumor)
- Vipoma
50
(No Transcript)
51
(No Transcript)
52
(No Transcript)
53
(No Transcript)
54
(No Transcript)
55
Exocrine Pancreas
- The disorders of the exocrine pancreas are
relatively common in clinical practice. The three
most frequent are - Acute pancreatitis
- Chronic pancreatitis
- Carcinoma of the pancreas
56
(No Transcript)
57
Acute Pancreatitis
- In acute pancreatits, activation of the
pancreatic enzymes causes autodigestion of the
gland. - abdominal pain
- associated with raised levels of pancreatic
enzymes (amylase and lipase) in blood and urine. - It varies in severity from a mild, self-limited
condition called acute interstitial pancreatitis
(interstitial edema and inflamation of the
pancreas) to a severe life-threatening disorder
referred to as acute hemorrhagic pancreatitis,
which exhibits extensive hemorrhage into the
parenchyma of the pancreas. - About 80 of cases are associated with
cholelithiasis and alcoholism.
58
Pathogenesis
- Features of pancreatitis include tissue
proteolysis, lipolysis, and hemorrhage, resulting
from the destructive effect of pancreatic enzymes
released from acinar cells. - mechanisms are as follows
- Pancreatic duct obstruction (by gallstones, with
impaction in the ampulla of Vater and pancreatic
duct obstruction). An enzyme-rich interstitial
fluid accumulates, and the tissue leukocytes
release proinflammatory cytokines, promoting
local inflammation and edema). - Primary acinar cell injury (by viruses mumps,
drugs, trauma, and the ischemia of shock). - Defective intracellular transport of the
proenzymes (acinar cell digestive enzymes are
misdirected toward lysosomes rather than toward
secretion lysosomal hydrolysis of the proenzymes
promotes local release of activated enzymes.
59
Morphology
- basic pancreatic alterations
- Leakage of the vasculature to cause edema
- Necrosis of regional fat by lipolytic enzymes
- acute inflammatory reaction
- Proteolytic destruction of the pancreatic
substance - Destruction of the blood vessels with subsequent
interstitial hemorrhage
60
Clinical features
- medical emergency with acute abdomen, intense
abdominal pain with upper back radiation,
peripheral vascular collapse, and shock from
explosive activation of the systemic inflammatory
response. - Death from shock, ARDS, or acute renal failure
- Laboratory marked elevation of the serum
amylase during the first 24 hours, followed
within 72-96 hours by a rising serum lipase.
Hypocalcemia may result from precipitation of
calcium soaps in the fat necrosis if persistent
is a poor prognostic sign. - Common sequela are a sterile pancreatic abscess
from liquefaction of the tissue and pancreatic
pseudocyst from aberrant drainage of pancreatic
secretions.
61
acute pancreatitis
62
(No Transcript)
63
(No Transcript)
64
(No Transcript)
65
Chronic Pancreatitis
- repeated bouts of mild to moderate pancreatic
inflammation, with continued loss of pancreatic
parenchyma and replacement by fibrous tissue. - more debilitating than life-threatening because
of progressive loss of pancreatic function. - alcoholism and biliary tract disease, and less
commonly hypercalcemia, and hyperlipidemia. - Morphologic findings
- fibrosis
- reduced number and size of acini
- sparing of the islets of Langerhans
- variable obstruction of pancreatic ducts
66
Chronic pancreatitis
- may be silent, or recurrent attacks of pain may
occur at scattered intervals. - precipitated by alcohol abuse, overeating, and
drug use. - may have mild elevations of serum amylase and
lipase in the long run the destruction of acinar
cells precludes such diagnostic clues. - Late complications include
- Diarrhea (malabsorbtion)
- Steatorrhea
- Diabetes
- Pseudocyst
67
Carcinoma of the Pancreas
- Carcinoma of the pancreas refers to carcinoma of
the exocrine pancreas, almost always arising from
ductal epithelial cells (adenocarcinoma). - It is the fourth most common cause of death in
the US and accounts for 5 of all cancer death. - Survival rates are 18 at 1 year and only 2 at 5
years. - Incidence rates are higher in smokers (2-3 x)
than in nonsmokers alcohol consumption imposes a
modestly increased risk. - 65-80 y/o, MgtF, BgtW.
68
(No Transcript)
69
Morphology
- Distribution
- Head 60
- Body 15
- Tail 5
- Diffuse or widely spread 20
- small and ill defined or large (8-10 cm), with
extensive local invasion and regional metastases. - Microscopically, more or less differentiated
glandular patterns (adenocarcinoma) arise from
ductal epithelium, mucous or non-mucous
secreting.
70
(No Transcript)
71
(No Transcript)
72
(No Transcript)
73
Clinical features
- fatigue, anorexia, weight loss, and painless
jaundice. Pain may develop later in the course. - local extension or metastases at the time of
diagnosis. - With tumors in the head of the pancreas, the
ampullary region is invaded, obstructing the
outflow of the bile patients usually die of
obstructive jaundice and hepatobilliary
dysfunction while the tumor is still relatively
small and not widely disseminated. - In marked contrast, carcinoma of the body and
tail of the pancreas remain silent for some time
and may be quite large and widely disseminated by
the time they are discovered. - Migratory thrombophlebitis (Trousseau sign) may
occur, particularly with carcinoma of the body
and tail.
74
Diagnosis of pancreatic adenocarcinoma
- Tumor markers, including carcinoembryonic antigen
(CEA), CA 19-9, and CA 125, are associated with
pancreatic cancer but are not accurate enough to
rule in or rule out a clinical diagnosis. - CT is the principal diagnostic test, although
MRI, endoscopic ultrasonography, and ERCP each
have a role. - Cytologic and histologic specimens can be
obtained by ERCP. The aim is to determine if
curative resection (pancreaticoduodenectomy
Whipple procedure) is possible.
75
.
.
76
- About half of the patients who are deemed to have
operable disease by imaging studies are found to
have unresectable tumors at laparatomy. - In most instances, therapy is palliative, with
the aim of relieving jaundice, pain, and duodenal
obstruction. ERCP with billiary stent placement
relieves jaundice in most patients with
unresectable tumors. - Survival is related to functional status and is
usually 6-12 months.