CH 14 Applications of Recombinant DNA Technology - PowerPoint PPT Presentation
1 / 30
Title:
CH 14 Applications of Recombinant DNA Technology
Description:
Fig. 10.12 Chorionic villus sampling, a procedure used for early prenatal ... Chorionic villus sampling can be done earlier, in the 8th 12th weeks of ... – PowerPoint PPT presentation
Number of Views:378
Avg rating:3.0/5.0
Title: CH 14 Applications of Recombinant DNA Technology
1
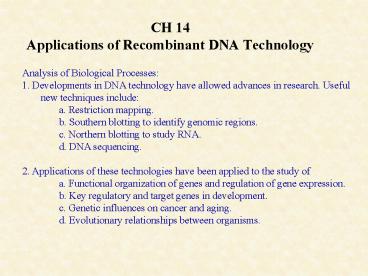
CH 14Applications of Recombinant DNA Technology
Analysis of Biological Processes 1. Developments
in DNA technology have allowed advances in
research. Useful new techniques include a.
Restriction mapping. b. Southern blotting to
identify genomic regions. c. Northern blotting to
study RNA. d. DNA sequencing. 2. Applications
of these technologies have been applied to the
study of a. Functional organization of genes and
regulation of gene expression. b. Key regulatory
and target genes in development. c. Genetic
influences on cancer and aging. d. Evolutionary
relationships between organisms.
2
Using Northern Blots to study transcriptionGluco
se Repression of Transcription of the Yeast GAL1
Gene
- GAL (galactose) genes in the yeast Saccharomyces
cerevisiae encode enzymes for break down of
galactose, which serves as their inducer. - Glucose represses GAL gene expression, and
existing GAL mRNAs are degraded, as shown by
Northern blot analysis of yeast samples taken at
time points and probed with the GAL genes. - Glucose added at time zero and amount of GAL1
transcripts analyzed at various times thereafter
by Northern blotting and probing
3
DNA Molecular Testing for Genetic Disease
Mutations
- 1. Many human diseases result from protein
defects caused by DNA mutations. DNA testing is
increasingly available for genetic diseases,
including - a. Huntington disease.
- b. Hemophilia.
- c. Cystic fibrosis.
- d. Tay-Sachs disease.
- Sickle-cell anemia.
4
Concept of DNA Molecular Testing
- 1. Designing DNA molecular tests requires
knowledge of gene mutations that cause a disease,
derived from sequencing the gene involved. - 2. Often many different mutations of a gene can
cause loss of function and lead to disease. The
breast cancer genes BRCA1 and BRCA2 are examples - a. Normal BRCA1 and BRCA2 genes control cell
growth in breast and ovarian tissue. - b. Mutations in the BRCA1 and BRCA2 genes can
lead to cancer. Hundreds of mutations in these
genes have been identified. - Each BRCA1 or BRCA2 mutation confers a different
risk of developing cancer, ruling out a single
DNA molecular test to assess an individuals
breast cancer risk associated with these genes. - Genetic testing reveals the presence of a
mutation associated with a genetic disease.
Genetic testing is usually done on a targeted
population of people with symptoms or a family
history of the disease.
5
Purposes of Human Genetic Testing
- 1. Human genetic testing serves three main
purposes - a. Prenatal diagnosis (fetal analysis).
- b.
- c.
6
Fetal Analysis
- Fetal Analysis is concerned with whether a fetus
is normal. A sample of fetal cells is needed for
the analysis. There are currently two methods of
obtaining the necessary sample
7
Fetal Analysis
Fig. 10.11 Amniocentesis, a procedure used for
prenatal diagnosis of genetic defectsAmniocentes
is is -Fluid contains fetal skin
cells -Seldom done before the 12th week of
pregnancy, due to small amounts of amniotic fluid
and risk to the fetus. -Cells cultured and
examined -Complicated and costly, so used
primarily in high risk cases
8
Fetal Analysis Fig. 10.12 Chorionic villus
sampling, a procedure used for early prenatal
diagnosis of genetic defects
- Chorionic villus sampling can be done earlier, in
the 8th12th weeks of pregnancy, by removal of
chorionic villus tissue either through the
abdomen as in amniocentesis, or via the vagina - Chorion is a
Fig 10.12
9
Fetal Analysis
- Once fetal cells are obtained they are usually
cultured in the laboratory, although chorionic
villus sampling may provide enough tissue to
assay directly. - Cells are examined for protein or enzyme
alterations or deficiencies, DNA mutations and
chromosomal abnormalities. - Amniocentesis is costly and cannot be performed
until the second trimester, removing early
abortion as an option in cases of severe genetic
defects. - Chorionic villus sampling can be done earlier,
but carries a higher risk of fetal death and
inaccurate diagnosis due to the presence of
maternal cells.
10
Fetal Analysis
- If both parents are carriers (heterozygotes) for
the mutant allele, the probability is 1/4 that
the fetus is an affected homozygote, 1/2 that it
is a carrier, and 1/4 that it is homozygous for
the normal allele. Genetic testing can determine
the result of a particular conception. - b. Genetic testing may be used during in vitro
fertilization to eliminate before implantation
embryos with mutated genes that could result in
serious disease... Ethical concerns?
11
Newborn screening
- Examples of tests for specific mutations using
blood from newborns include - a. Phenylketonuria (PKU)
- b. Sickle-cell anemia
- c. Tay-Sachs disease
12
Phenylketonuria (PKU)
- Phenylketonuria (PKU) is commonly caused by a
mutation on chromosome 12 in the phenylalanine
hydroxylase (PAH) gene (12q24.1) - 2. Phenylalanine is an essential amino acid, but
excess is harmful, and so is normally converted
to tyrosine. Excess phenylalanine affects the
CNS, causing mental retardation, slow growth and
early death.
Tyrosinase
PAH
Fig. 10.1 Phenylalanine-tyrosine metabolic
pathways
13
Phenylketonuria (PKU)
- PKUs effect is pleiotropic (wide reaching). Some
symptoms result from excess phenylalanine. Others
result from inability to make tyrosine these
include fair skin and blue eyes (even with
brown-eye genes) and low adrenaline levels. - Diet is used to manage PKU by providing just
enough phenylalanine for protein synthesis, but
not enough that it accumulates. To be effective,
the special diet must commence in the first two
months after birth, continue at least throughout
childhood, and be resumed before pregnancy in PKU
women to avoid phenylalanine levels that would
affect the fetus. - 5. All U.S. newborns are screened for PKU using
the Guthrie test - a. A drop of blood on filter paper is placed on
solid media containing b-2-thienylalanine and the
bacterium Bacillus subtilis. - b. Normally, b-2-thienylalanine inhibits growth
of Bacillus subtilis. - Phenylalanine allows Bacillus subtilis to grow in
the presence of b-2-thienylalanine, so bacterial
growth indicates high phenylalanine levels in the
blood, and the possibility that the infant has
PKU. - 6. NutraSweet ...
14
Sickle Cell Anemia
- J. Herrick (1910) first described sickle-cell
anemia, finding that red blood cells (RBCs)
change shape (form a sickle) under low O2
tension. - Sickled RBCs are fragile, hence the anemia.
- They are less flexible than normal RBCs, and form
blocks in capillaries, resulting in tissue damage
downstream. - Effects are pleiotropic, including damage to
extremities, heart, lungs, brain, kidneys, GI
tract, muscles and joints. Results include heart
failure, pneumonia, paralysis, kidney failure,
abdominal pain and rheumatism. - d. Heterozygous individuals have
15
Sickle Cell Anemia
- 2. Linus Pauling and coworkers (1949) used
electrophoresis and showed - Hemoglobin from individuals with sickle-cell
anemia (Hb-S) has altered mobility compared with
normal hemoglobin (Hb-A). - Hemoglobin from individuals with the sickle-cell
trait shows equal amounts of Hb-A and Hb-S,
indicating that - Therefore, the sickle-cell mutation changes the
form of its corresponding protein, and protein
structure is controlled by genes.
Sample loaded
-
Fig. 10.6 Electrophoresis of hemoglobin variants
16
Human ?-globin
- ?-globin subunit of hemoglobin
- Hemoglobin
- Binds O2 in lungs
- Delivers O2 to tissues in exchange for CO2
- Binds CO2 in tissues releases it in the lungs
(although most CO2 carried by bicarbonate)
17
Human ?-globin
Most aa coil into ?-helices fold around heme
group
18
Human ?-globin
Heme groups iron atom surrounded by
protoporphyrin ring Heme groups are examples of
nonprotein substances added to proteins after
translation
19
Human Hemoglobin
Hemoglobin is formed by four polypeptide chains,
two molecules of the a polypeptide and 2 of the b
polypeptide, each associated with a heme group
Quaternary
20
Human Hemoglobin
- How does hemoglobin bind O2 and CO2?
- Hydrophobic heme groups in pocket lined with
hydrophobic amino acids (both ? ? subunits) - O2 binds to hydrophobic heme pocket
- Surface amino acids of hemoglobin are
hydrophilic - Allows hemoglobin to function in erythrocytes
- Arginine at carboxyl end of ?-globin bind CO2
- Cant bind O2 and CO2 simultaneously
- CO2 binding
- Release of CO2
21
Sickle Cell Anemia
- V.M. Ingram (1956) found that the 6th amino acid
of the b chain in sickle-cell hemoglobin is
valine (no electrical charge) rather than the
negatively charged glutamic acid in the b chain
of normal hemoglobin - Outline of the genetics and gene products
involved in sickle-cell anemia and trait - a. Wild-type b chain allele is bA, which is
codominant with bS
Fig. 10.8 The first seven N-terminal amino acids
in normal and sickled hemoglobin ? polypeptides
22
Sickle-Cell Anemia
Hydrophobic valine at aa 6 embeds itself into the
hydrophobic heme pocket in a ? subunit of another
deoxygenated hemoglobin
23
Sickle-Cell Anemia
Several Hb S molecules attach to each other to
form a long double- stranded polymer
24
Sickle-Cell Anemia
Seven double-stranded polymers wind around each
other to form a sickle hemoglobin fiber Sickle
hemoglobin fibers cause erythrocytes to assume a
sickle shape Sickle cells clog capilaries -gt
tissue damage
25
(No Transcript)
26
Fig. 14.2 The beginning of the ?-globin gene,
mRNA, and polypeptide showing the normal Hb-A
sequences and the mutant Hb-S sequences
- RFLPs are associated with many genetic disorders.
Sickle-cell anemia is an example - A single base-pair change in the b-globin gene
results in abnormal hemoglobin, Hb-S, rather than
the normal Hb-A. Hb-S molecules cause sickling of
red blood cells. - b. The Hb-S mutation is an AT-to-TA base pair
change in the 6th codon of b-globin, resulting in
a valine rather than a glutamic acid, and also
eliminating a
27
probe
Fig. 14.3 Detection of sickle-cell gene by the
DdeI restriction fragment length polymorphism
- In the normal b-globin (Hb-A) gene there are
three DdeI sites, while the sickling form, Hb-S,
has only two DdeI sites. This difference can be
detected using Southern blot hybridization of
28
Examples of amino acid substitutions found in ?
polypeptides of various human hemoglobin variants
29
Fig. 4.5 The biochemical step for the conversion
of the brain ganglioside GM2 to the ganglioside
GM3, catalyzed by the enzyme N-acetylhexosaminidas
e A (hex A)
- 1. Caused by recessive mutation at the gene hexA
(15q23-q24), which encodes the lysosomal enzyme
N-acetylhexosaminidase A( HexA). The HexA enzyme
cleaves a terminal N-acetylgalactosamine group
from a brain ganglioside, a complex nerve
membrane glycolipid
30
Tay-Sachs disease
- 2. Infants homozygous recessive for this gene
will have nonfunctional HexA enzyme. Unprocessed
ganglioside accumulates in brain cells, and
causes various clinical symptoms - a. Infants have enhanced reaction to sharp
sounds. - b. A cherry-colored spot surrounded by a white
halo may be visible on the retina. - c. Rapid neurological degeneration begins about
one year of age, as brain loses control of normal
functions due to accumulation of unprocessed
ganglioside. - d. Progress is rapid, with blindness, hearing
loss and serious feeding problems leading to
immobility by age 2. - e. Death often occurs at 34 years of age, often
from respiratory infection. - 3. The disease is incurable. Carriers and
affected individuals can be detected by genetic
testing.