Manipulation of the immune response: - PowerPoint PPT Presentation
Title:
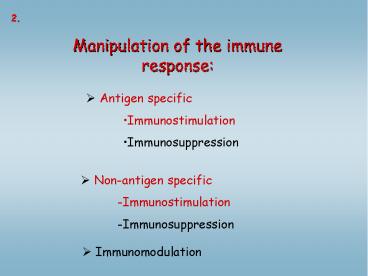
Manipulation of the immune response:
Description:
2. Manipulation of the immune response: Antigen specific Immunostimulation Immunosuppression Non-antigen specific-Immunostimulation-Immunosuppression – PowerPoint PPT presentation
Number of Views:265
Avg rating:3.0/5.0
Title: Manipulation of the immune response:
1
2.
Manipulation of the immune response
- Antigen specific
- Immunostimulation
- Immunosuppression
- Non-antigen specific
- -Immunostimulation
- -Immunosuppression
- Immunomodulation
2
Targets of immunotherapies elements of the
immune response cytokines, adhesion molecules,
cell membrane molecules, receptors,
antibodies Antibodies as drugs specificity
? antigenicity humanized antibodies,
targeting
3
Immunotherapies
Immunostimulation
- Induction of immune response against
- pathogenic microbes
- Inducing immunreponse against tumor cells
Immunosuppression
-inhibition of autoimmun processes -inhibition of
allergy -inducing transplantion
tolerance -fight against newborn haemolytic
aenemia
Immunomodulation
- shifting TH1 / TH2 balance in autoimmune diseases
or allergy - -modulation of antibody isotype in allergy
4
Fighting against infections
- After infection ?
- Traditional drugs (antibiotics, anti-viral drugs)
- Passive immunization (antibodies, cells)
- Aktive vaccination
Before infection ? vaccination ? 1) increase
the ratio of antigen specific cells
2) inducing specific immunological
memory
5
IMMUNOSTIMULATION -vaccination
Infectious diseases, epidemics Edward Jenner,
1796, smallpox
A landmark was discovery of the germ theory,
which included small parasites, bacteria and
viruses. This theory was mainly based on the
studies of Robert Koch (1843-1910), Louis Pasteur
(1822-1895) and many others.
6
What will happen next.......
7
(No Transcript)
8
Vaccine approaches
Type of vaccine Examples
Live attannuated or killed bacteria BCG, cholera
Live attennuated viruses Polio, rabies
Subunit (antigen) vaccine Tetanus toxoid, diphteria toxoid
Conjugate vaccines Haemophilus influenzae Pneumococcus
Synthetic vaccines Hepatitis (recombinant proteins)
Viral vectors linical trials of HIV ags in canarypox vector
DNA vaccines Clin trials ongoing for several infections
9
- Antigen specific immunostimulation
- Active immunization
- killed microbes
- attenuated microbes
- crossreactive microbe
- non-pathogenic live microbes
- non-toxic modified form
- modified microbial toxin
- Results
- antibody production effector T cells
- Adjuvants support immunostimulation
- concentrating ag
- prolonged contact with ag
- stimulation ofAPC
10
- Passive immunization rapid treatment of
potentially fatal disease - antigen specific IgG from hyperimmunized animal
(or human) - advantage immediate protection, but
transient, disadvantage no memory, - elimination of IgG, hypersensitivity,
neutralization, - species specific immune response
- application antitetanic sera, snakebite
- human IgG antibody defficiency
- Adaptive immunization
- therapy with immunocompetent cells
- - immunodeficiency
- congenital cellular immunodeficieny
- bone marrow (MHC compatibility!) or
immunocompetent cells from fetal liver, thymus
-enzyme deficiency
adenosin deaminase, - nucleosid phosphorylase
- somatic gene therapy bone marrow stem cells
transfected with a viral vector containing the
desired gene
11
Vaccination antigen specific immunostimulation V
accine against the microbe, or toxin produced by
the microbe Live, attennuated virus are more
efficient compared to killed virus (effector
mechanisms, CD8T cells higher ?) but
risk! ? New techniques Recombinant DNA
technologies Immunization with dendritic cells
new type vaccines
- Attennuation of pathogenic microbes
- Culturing virus in monkey cells ? mutations ?
virus growth in monkey cells, but ? does not
growth in human cells ? vaccine
- In vitro mutagenesis irreversible modification
of virus gene - influensa- changes every year - antigén shift
- directed mutagenezis
12
Attenuation of the pathogenic virus by culturing
in non-human cells
13
(No Transcript)
14
Mechanisms of the changes of surface antigens
on influensa virus antigen-drift and
antigen-shift
human virus
antigen drift
lung epithel cells
lung epithel cells
human virus
bird virus
antigen shift
lung epithel cells
lung epithel cells
Antigen drift continous small changes in viral
genes Antigen shift genes from two different
virus strains are mixed -gt new virus
15
Antigenic Drift Each years flu vaccine contains
three flu strains -- two A strains and one B
strain -- that can change from year to
year. After vaccination, your body produces
infection-fighting antibodies against the three
flu strains in the vaccine. If you are exposed to
any of the three flu strains during the flu
season, the antibodies will latch onto the
viruss HA antigens, preventing the flu virus
from attaching to healthy cells and infecting
them. Influenza virus genes, made of RNA, are
more prone to mutations than genes made of
DNA. If the HA gene changes, so can the antigen
that it encodes, causing it to change shape If
the HA antigen changes shape, antibodies that
normally would match up to it no longer can,
allowing the newly mutated virus to infect the
bodys cells. This type of genetic mutation is
called antigenic drift.
16
Pathogenic virus Mutation or deletion of
virulence gene Immunogenic but avirulent virus
-gt vaccine
17
- Development of non-pathogenic mutants
- Virus polio, mumps, rubella, measles, etc.
deletion or mutation of gene (s) necessery for
virulence - Bacterium Salmonella typhy non virulent
mutants were selected - - UDP galactose epimerase enzyme mutation --LPS
synthesis LPS low in mutants - -Targeting enzyme ? Tyr, Phe syinthesis, ?
- slow proliferation - ? vaccination
- chiken salmonella vaccination important
- Conjugate vaccine
- B and helper T cells recognize different epitopes
in the same molecular complex - Haemophilus influenzae B
- T cell-independent B cell response, to
polysacharide chain of bacteria - tetanusz toxoid polysacharide conjugate - gt T
dependent, efficient response even below two
years age - Tetanusz toxoid specific T cells produce
cytokines - B cell antibody against bactaerial
polysacharide
18
Haemophilus influenzae type B vaccine
- Conjugate vaccine
- B and helper T cells recognize different epitopes
in the same molecular complex
19
(No Transcript)
20
(No Transcript)
21
- Reverse immunogenetics
- Determination of T cell epitopes
HLAB53 protects against fatal cerebral
malaria. HLAB53binding peptides are identified
nonapeptide with proline at position 2 From
pathogen infected cells -gt identification of the
bound peptide with X Pro sequence Plasmodium
falciparum Strong T cell proliferation
Peptide -gt terapy
22
- Attennuated live microorganisms, as vector
- combined vaccine
- Salmonella tetanus toxoid ag, Listeria
monocytogenezis - Leishmania
- Yersinia pestis
- Schistosoma mansoni genes
- virus non-pathogenic (plant), many genes in
one - microbe as carrier antigene built in,
- cannot be repeated
- Synthetic peptides
- identification of T cell epitopes, ? peptide
synthesis - Disadvantage variability
- ISCOM immune stimulatory complex
- liposomes with peptides sejtbe bejut
23
Immunstimuláló komplex peptiddel
Fúzió
Peptid transzport az ER -be
Peptid bemutatása az MHCI-en keresztül a T sejtek
számára
24
(No Transcript)
25
(No Transcript)
26
(No Transcript)
27
Succesful vaccinations
SSPE stands for subacute sclerosing
panencephalitis, a brain disease that is a late
consequence of measles infection in a few
patients.
28
(No Transcript)
29
(No Transcript)
30
(No Transcript)
31
(No Transcript)
32
(No Transcript)
33
Diseases for which effective vaccines are still
needed. The number of people infected is
estimated at 200 million, of which 20 million
have severe disease. Current measles vaccines
are effective but heat-sensitive, which makes
their use difficult in tropical countries.
Estimated mortality data for 1999 from World
Health Report 2000 (World Health Organization).
34
Types of virus infection
polio, influenza, mumps, Yellow fever
herpes, varicella, EBV
HIV, hepatitis B, hepatitis C
35
Immune response after infection
36
Kinetics of antibody response
37
Targets of virus specific antibodies
38
PROBLEMS with vaccines
Specificity, isotype, localization of antibody
response is not correct
Antibody response does not provide protection
Adaptation mechanisms of pathogens inhibit the
immune reponse
39
Antibody production citotoxic T cells
activation protection against the virus
DNA targeting the right ligand,
internalization and direction to endosome
fusion with lysosomes lysosomal enzymes
degrade enzimek Synthetic virus
40
Intranasal, intrarectal, intravaginal
immunization ?mucosal immunization TL induction
in Peyer plaques, lamina propria Adjuvants pl.
cholera toxin B cAMP induction, IL-12
production suitable for mucosal immunization DNA
based vaccination Delivery in vivo
electroporation, gene gun ? whole protein
gene, or peptide MHCI, MHCII
presentation Viral vector (vaccinia, poxvirus)
strengthen the efficiency of rec DNA
Nuclear transzlocation signál
DNA plasmid
ligand
Endosomal lyzis, or bypass
?
Tissue specific regulated promoter
Therapic gene
41
(No Transcript)
42
Vaccine design
delivery, site of delivery
43
Selection of the epitope
APC
T
B
44
Selection of the epitope
45
- Strategies to develop new generation of
vaccines - Virus do not express suitable T cell epitopes
(selection during evolution) - Tumor suitable T cells are deleted
- Epitope enhancement
- increase peptide- MHC binding affinity - MHCII
TH cells repair of anchoring aa. - combinatorial peptide libraries
- peptide-MHC complex increase TCR- binding
affinity activation of both small and large
affinity T cells ? - increase the number of T cells that recognize
tumor epitope - increase TCR crossreactivity peptid chimera
recognition of different virus strains
46
Efficiency can be increased by modifying peptide
sequence
47
VACCINE DESIGN
48
COMPARISON OF VARIOUS TYPES OF VACCINES
49
(No Transcript)
50
The efficient vaccine - safe can be applied
to everyone including children - efficient to
protect against infection or disease (less
efficient) - protection for life long
memory - induce neutralizing antibodies -
induce T cell response - stabile, cheap,
no/few side effect - easy applicable (oralis
vaccine, e.g. Sabin dropp) - acceptable and
applicable everywhere (developing world)
Adjuvants non-specific signal, stimulation
of APC cytokine induction, antigén-depo slow
felszívódás aluminium hidroxid, or oil
emulsion. mixed vaccines - one can activate the
other ( e.g. Bordatella Pertussis
tetanusdifteria) cytokines IL-12 - TH1
response The way of immunization
Important the site of infection/
immunizations Oral vaccines the role of
mucosa (MALT)
51
Dendritikus sejtek mint vakcina hordozók