Acid Base Jeopardy - PowerPoint PPT Presentation
1 / 66
Title:
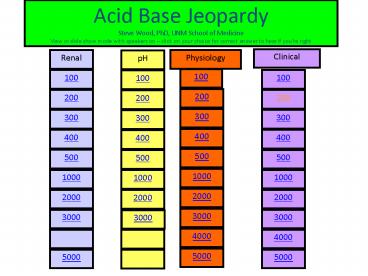
Acid Base Jeopardy
Description:
Acid Base Jeopardy Steve Wood, PhD, UNM School of Medicine View in show mode with speakers on click on your choice for correct answer to hear if you re right – PowerPoint PPT presentation
Number of Views:134
Avg rating:3.0/5.0
Title: Acid Base Jeopardy
1
Acid Base Jeopardy Steve Wood, PhD, UNM School of
Medicine View in slide show mode with speakers on
click on your choice for correct answer to hear
if youre right
Clinical
Renal
Physiology
pH
100
100
100
100
200
200
200
200
300
300
300
300
400
400
400
400
500
500
500
500
1000
1000
1000
1000
2000
2000
2000
2000
3000
3000
3000
3000
4000
4000
5000
5000
5000
2
explanation
3
explanation
4
(No Transcript)
5
explanation
6
explanation
7
(No Transcript)
8
explanation
9
explanation
10
The diuretic acetylzolamide (diamox) inhibits the
enzyme carbonic anhydrase. Which of the
following data sets shows the expected effects of
this drug on pH and renal function?
Urine pH Blood pH Urine vol. Net acid exc.
A
B
C
D
explanation
11
- Acetylzolamide (diamox) is an inhibitor of
carbonic anhydrase. Predictable side-effects
effects of diamox treatment would include - Diuresis and acidification of urine, decreased
blood PCO2 - Antidiuresis, decreased blood Na and PCO2
- Increased Na excretion, diuresis, alkalinization
of urine, decreased blood pH - Diuresis, increased Hsecretion, no change in
blood PCO2
explanation
12
(No Transcript)
13
explanation
14
explanation
15
explanation
16
(No Transcript)
17
(No Transcript)
18
explanation
19
explanation
20
(No Transcript)
21
A buffer system e.g.,
HA
H
A
-
is most effective when
A.
HA gt A
-
B.
HA lt A
-
C.
HA A
-
D.
pH gt
pK
22
The defense against acid load with the slowest
response time is
- Chemical buffering
- Renal compensation
- Respiratory compensation
- Hemoglobin proton coupling
23
- The acid base status of a pregnant woman in
- the 3rd trimester is best depicted by point___.
- A) 3
- 4
- C) 7
- D) 2
- E) 6
24
A normal rate of bicarbonate reabsorption in the
renal tubule cells requires the enzyme
- Carbonic anhydrase
- Lactate dehydrogenase
- Tyrosine hydroxylase
- Carbonate reductase
25
The most important mechanism of hydrogen
secretion in the proximal tubule is
- H ATPase (electrogenic H pump)
- H - K antiporter
- Na - H antiporter
- diffusion
26
Lab results for a 24 hour urine sample show
Titratable acid 20 mEq NH4 40 mEq
HCO3- 3 mEqThe patients net acid excretion
is
- 63 mEq/day
- 20 mEq/day
- 57 mEq/day
- 23 mEq/day
27
The inhibition of ventilation by metabolic
alkalosis is countered (partially reversed) by
the stimulation of ventilation due to
- pH increases
- hypercapnia
- hypoxia
- low bicarbonate
28
COPD patient in respiratory failure. ABG report
PaO2 35 mm Hg PaCO2 64 mm Hg pH 7.2
Hb 10 g/dL Sat. 60 HCO3- 26
mEq/L Base excess 0 mEq/L
- Acid base status is most accurately described as
- Uncompensated metabolic acidosis
- Uncompensated respiratory acidosis
- Compensated respiratory acidosis
- Compensated metabolic acidosis
explanation
29
4. COPD patient with with cyanosis and marked
peripheral edema. ABG report
The patients acid base status on room air is
- Compensated respiratory alkalosis
- Uncompensated respiratory alkalosis
- Uncompensated metabolic alkalosis
- Compensated metabolic alkalosis
explanation
30
A COPD patient who is an alcoholic is admitted to
the ER after losing consciousness at home. ABG
shows
pH 7.2 PCO2 52 mm Hg HCO3- 18 mmEq/L PaO2
81 mm Hg
The patients acid base status is
- Normal
- Respiratory metabolic acidosis
- Respiratory acidosis
- Metabolic acidosis resp. alkalosis
- Metabolic alkalosis
31
During an operation, the arterial PCO2 and pH of
an anesthetized patient are monitored. The
patient is being ventilated by a mechanical
respirator, and the initial values are normal
(PCO2 40 mm Hg pH 7.41). If the ventilation
is increased, which of the following is most
likely to occur?
- Arterial PCO2
- Decrease
- Decrease
- Decrease
- Increase
- Increase
- Increase
- Arterial pH
- Decrease
- Increase
- No change
- Decrease
- Increase
- No change
explanation
32
A patient excretes 3 L of urine with a pH of 7.6
with a HCO3- 24 mEq/L. What is the net acid
excretion?
- 24 mEq/L
- 48 mEq/L
- Negative
- Can not tell from these data
explanation
33
Lab results for a patient with DKA show a HCO3-
10 mEq/L, PCO2 33 mm Hg. You forgot your
calculator and impress the chief resident by
telling her that you used the Henderson-Hasselbalc
h equation to calculate a pH _______.
- 7.4
- 6.8
- 6.1
- 7.1
explanation
34
Lab results for a patient with respiratory
failure and cholera show a HCO3- 2 mEq/L,
PCO2 66 mm Hg. You forgot your calculator and
impress the chief resident by telling her that
you used the Henderson-Hasselbalch equation to
calculate a pH _______.
- 7.4
- 6.8
- 6.1
- 7.1
explanation
35
Daily Double
36
Daily Double
37
Daily Double
38
Final Jeopardy
39
Use a bicarb pH diagram to plot the course of a
triple disorder in an alcoholic with ketoacidosis
who develops hyperventilation from liver failure
and then starts to vomit.
40
(No Transcript)
41
9
3
10
5
1
4
8
2
6
7
The diagram above shows plasma bicarbonate as a
function of pH at different PCO2 levels. The two
points that represent mixed acid base disorders
are
- 2 and 6
- 4 and 7
- 8 and 10
- 8 and 9
explanation
42
Filtered load GFR x plasma concentration
180 L/day x 24 mEq/L 4320 mEq/day
43
Alkalosis will inhibit the central and peripheral
Chemoreceptors causing hypoventilation and
increased PCO2, which will cause alveolar and
arterial PO2 to Decrease. This will stimulate
the carotid body PO2 receptor Which will oppose
the inhibition by alkalosis. Also, the
Increased PCO2 will compensate the
alkalosis. Systemic alkalosis causes
vasoconstriction in most vascular Beds. This may
be countered by the hypoxia in some beds But
normally there is cerebral and coronary
vasoconstriction. Alkalosis caused decreased
extra and intracellular calcium Leading to
prolonged action potentials and muscle spasm
(tetany).
44
urine may be alkaline as well as acidic,
depending on diet and/or compensation for
alkalosis. citrus fruits, due to high amounts of
citrate will produce alkaline urine. citrate
is metabolized to citric acid by adding a
hydrogen ion. this makes blood, and urine, more
alkaline. compensation for metabolic alkalosis
is both respiratory and by renal excretion of
bicarbonate.
45
Acidosis inhibits the slow calcium channels which
are activated during phase 2 of the cardiac
action potential. in addition, tissue acidosis
causes hydrogen in and potassium out of cells
leading to hyperpolarization (more negative
membrane potential). The force of contraction is
directly dependent on the magnitude of the
initial calcium influx, therefore acidosis
decreases the force of contraction. For more
http//www.accessmedicine.com/content.aspx?aID889
838 Used id rossmed password rossmed
46
CA is present in both the brush border of the
luminal membrane and in the cytoplasm.
nahco3 uptake from filtrate is inhibited so hco3-
reabsorption is blocked leading to higher urine
ph and lower blood ph
http//www.accessmedicine.com/content.aspx?aID943
477searchStracetazolamide
47
anion gap NA (CL HCO3-) 135 118 17
mEq/l pH 7.35 so acidosis. what kind? has to
be metabolic since pco2 is low, not high. PCO2
is down by 6 to partially compensate for HCO3-
being down by 6 (which would predict that ph
would be 7.3 and instead it is 7.35 due to
partial respiratory compensation
48
pH 7.29 acidosis PCO2 27 mmHg, so you
know its metabolic acidosis and
hyper Ventilation is compensatory HCO3- so you
also know it is metabolic acidosis
49
The concentration of free hydrogen ion is so
small it is measured in nanomoles (a nanomole is
a billionth of a mole) A pH of 7.4 40 nmoles/L
(extracellular) A pH of 7.0 is 100 nmoles/L
(typical intracellular)
50
The renal tubule cells normally secrete enough
hydrogen ion to completely reabsorb all the
filtered bicarb (4320 mEq/L) PLUS enough extra to
produce new bicarb to replace that lost in
buffering fixed acid from metabolism (80 mEq/L)
for a total of 4400 mEq/L
51
because pco2 is increased from 40 to 51 (11 mm
hg), you would expect the pH to be decreased by
about 0.1 units, which it is. so, you have
uncompensated respiratory acidosis. the pao2
increases to only 112 mm hg on 65 oxygen. this
probably means there is a fairly large right to
left shunt where venous blood entering the lungs
does not come into contact with the high oxygen
levels in the alveoli.
52
- Most of the acidification of urine takes place
- In the
- Proximal tubule
- Descending loop of Henle
- Ascending loop of Henle
- Distal tubule/collecting duct
explanation
53
explanation
54
acidosis stimulates the carotid body ph receptor
and causes systemic vasodilation. acidosis
causes hyper- kalemia and this lowers resting
membrane potential. sustained depolarization
lead to muscle weakness.
55
Diarrhea cause metabolic acidosis. HbO2 affinity
decreases. Acidosis stimulates the carotid body
pH receptor and causes systemic vasodilation.
Acidosis inhibits the slow calcium channels
which are activated during phase 2 of the cardiac
action potential. in addition, tissue acidosis
causes hydrogen in and potassium out of cells
leading to hyperpolarization (more negative
membrane potential). The force of contraction is
directly dependent on the magnitude of the
initial calcium influx, therefore acidosis
decreases the force of contraction. For more
http//www.accessmedicine.com/content.aspx?aID889
838 Used id rossmed password rossmed
56
the distal part of the nephron exchanges
cellular hydrogen and/or potassium ions for
sodium ions in the tubular urine. Ammonia
diffuses into acid urine and is trapped as
ammonium ion. Diamox, by interfering with the
supply of cellular hydrogen ions, reduces
exchange of hydrogen for sodium and favors the
exchange of potassium for sodium. Am J Physiol
194 125-134, 1958 Localization of
Acidification of Urine, Potassium and Ammonia
Secretion and Phosphate Reabsorption in the
Nephron of the Dog Robert F. Pitts 1, Ruth S.
Gurd 1, Richard H. Kessler 1, and Klaus
Hierholzer 1 1 From the Department of Physiology,
Cornell University Medical College, New York
City
57
Point 8 indicates a combination of respiratory
(high PCO2) and metabolic (lowered bicarb)
acidosis. This might happen in a patient with
lung disease who has diarrhea. Point 10 shows a
combination of respiratory (low PCO2) and
metabolic (high bicarb) alkalosis. This might
happen in a patient with liver failure who starts
vomiting. In liver failure toxins may stimulate
the respiratory ctr. Causing hyperventilation
(respiratory alkalosis) and low potassium may
also cause a metabolic alkalosis.
58
pH pK log HCO3-/(PCO2 x ?) pH 6.1 log
2/(66 x 0.03) 6.1 log 2/1.98 ? 6.1 (log 1
0)
59
pH pK log HCO3-/(PCO2 x ?) pH 6.1 log
10/(33 x 0.03) 6.1 log 10/1 ? 7.1 (log 10
1)
60
Net acid excretion (titratable acid ammonia)
urine bicarb If urine has pH gt 7.4 net acid
excretion is always negative.
61
Increased ventilation will lead to decreased PCO2
and, as a result, increased pH
62
Uncompensated respiratory acidosis because PCO2
is increased from 40 to 64 24. this predicts
that pH should be decreased by about 0.2 units,
which it is (7.2). If there were any renal
compensation, pH would be higher than 7.2 as
bicarbonate is produced by the kidneys and there
would be a positive base excess.
63
Compensated respiratory alkalosis because PCO2 is
decreased from 40 to 16 - 24. This predicts
that pH should be increased by 0.2 units, to 7.6.
With renal compensation, bicarb is decreased to
15, so the actual pH is 7.5 (partial
compensation).
64
The pH is acidosis. The low bicarb means its
metabolic. The low PCO2 means the expected
respiratory compensation (hyperventilation) has
occurred. The anion gap is 140 (112 12)
16 mEq/L (normal range ? 8 16)
65
Filtered sodium enters the proximal tubule by way
of several co-transporters (see figure) but most
of the reabsorption is via the Na-H antiporter.
66
(No Transcript)