Goal of Quality Control - PowerPoint PPT Presentation
1 / 7
Title:
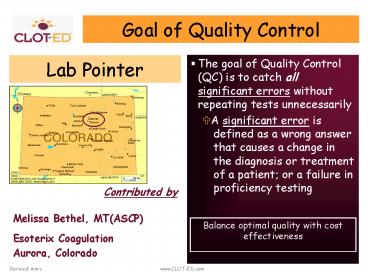
Goal of Quality Control
Description:
Balance optimal quality with cost effectiveness. Contributed by. Melissa Bethel, MT(ASCP) Esoterix Coagulation. Aurora, Colorado. What's Wrong With 2SD Ranges? ... – PowerPoint PPT presentation
Number of Views:41
Avg rating:3.0/5.0
Title: Goal of Quality Control
1
Goal of Quality Control
- The goal of Quality Control (QC) is to catch all
significant errors without repeating tests
unnecessarily - ?A significant error is defined as a wrong answer
that causes a change in the diagnosis or
treatment of a patient or a failure in
proficiency testing
Lab Pointer
Contributed by Melissa Bethel,
MT(ASCP) Esoterix Coagulation Aurora, Colorado
Balance optimal quality with cost effectiveness
2
Whats Wrong With 2SD Ranges?
- With 2 controls, there is 10 chance that the
run will be rejected when there is NOTHING wrong - With 3 controls per run, there is 15 chance of
rejection when there is NOTHING wrong - This wastes
- Time
- and causes frustration!!!
Not againmy control is out of 2 standard
deviations!
3
What to do?
- Analytes show varying biological variation and
assays show varying accuracy precision.
Therefore, in order to detect clinically
significant errors, it is best to determine QC
rules for an assay that are specifically based
on 1) its Total Allowable Error (TEa) and 2) its
specific performance.
Should I automatically repeat my controls?
Thats not true troubleshooting! You need to
develop QC ranges based on how your assay
performs and its total allowable error.
TEa allowable error based on CLIA requirements
for proficiency testing or determined from
individual and group biological variance
4
Solution Assay Specific QC Rules
- Determine TEa for the analyte from CLIA
regulations or biological variation tables - Using the Operational Process Specification
(OPSpecs) charts obtainable from the Westgard web
site at www.westgard.com, calculate which
Westgard rules are optimal based on the precision
accuracy of each analyte in relation to the
permitted biological variation
- Validate assay to determine imprecision ( cv)
and inaccuracy (bias) - Establish mean and standard deviation using the
historical coefficient of variation (cv) for the
assay (not simply using a 2SD range established
from 20-30 runs)
5
Example Historical CV
- Take monthly cv for each control level
- Average for 1 year
- Calculate the SD based on
- SD mean x historical cv
- Use the calculated SD to set the mean /- 2SD
limit
Takes into account slight variation in
instrumentation and reagents over time.
6
Total Allowable Error
- For Proficiency Testing, CLIA acceptable limits
for TEa are - Prothrombin Time 15
- APTT 15
- Fibrinogen 20
7
Westgard OPSpecs Charts
- An Operational Process Specifications (OPSpecs)
chart (at left) shows the relationship between
the quality required for a test and the
imprecision, inaccuracy, and QC that are
necessary to assure quality is achieved in
routine operation. - Allowable inaccuracy on the y- axis versus
allowable imprecision on the x-axis - One or more lines representing the operating
limits (allowable limits of imprecision and
inaccuracy). These lines correspond to different
Westgard control rules and different numbers of
control measurements that would provide at least
90 detection of medically important systematic
errors. - A top line, maximum limits for stable process,
defines the limits of inaccuracy and imprecision
for a method that is perfectly stable and would
require no quality control. - Normalized Operating Point indicates the
imprecision and inaccuracy of an individual
method (example, Prothrombin Time) - X-coordinate method cv () divided by defined
TEa (), then multiplied by 100 (1.04 cv
divided by 15 TEa x 100 6.9) - Y-coordinate method bias () divided by defined
TEa (), ratio then multiplied by 100 (1 bias
divided by 15 TEa x 100 6.7)
Prothrombin Time
The box to the right of the chart matches the
dots and dashes of the different operating limit
lines on the chart to the particular control
rules and numbers of control measurements (N)
being considered. The probablity for false
rejection (Pfr) and the number of runs (R) over
which the control rules are applied is also
shown. An R of 1 means the rules are applied to
the control data in a single run.
Prothrombin Time Example One run using two
controls offers 90 AQA (analytical quality
assurance for systematic error or the chance for
detecting medically important systematic errors)
and 0 probability for false rejection when using
the 13s Westgard Rule.