Pyridoxine sensitivity in Primary Hyperoxaluria - PowerPoint PPT Presentation
1 / 38
Title:
Pyridoxine sensitivity in Primary Hyperoxaluria
Description:
Dutch Society of Pediatric Nephrology. Dutch Society of Nephrology ... Christiaan van Woerden Resident Paediatrics. Simone Denis Technician ... – PowerPoint PPT presentation
Number of Views:234
Avg rating:3.0/5.0
Title: Pyridoxine sensitivity in Primary Hyperoxaluria
1
Pyridoxine sensitivity in Primary Hyperoxaluria
Christiaan v Woerden, Hans Waterham, Frits
Wijburg, Ronald Wanders, Jaap GroothoffEmma
Childrens hospital AMC, Amsterdam
2
What has brought them to the top?
What made them the greatest?
genes?
environment?
3
Primary Hyperoxaluria I (PHI) peroxisomal
enzyme (AGT) deficiency in the liver
4
Role of pyridoxine (B6)
- Essential co-factor of AGT
- mutation Gly82Glu inhibits B6 binding? no AGT
activity - Reduction of oxalate excretion by B6 in B6
deficiency - Reduction oxalate excretion pharmacological
dosages B6 in 30 of PH1 patients W Europe
5
PH1 extreme heterogenous phenotypical expression
- No symptoms, sole kidney stones,
nephrocalcinosis, UTI - or
- Interstitial nephritis fibrosis, ESRD? systemic
oxalosis - retinopathy , blunted vision, bone pain,
fractures, ?growth, arthopathy - peripheral neuropathy, heartblock,
myocarditis, skin calcification, peripheral,
gangreen, pancytopenia, splenomegaly, vascular
calcification, arterial wall stiffening
6
Genotype-phenotype association? Impact B6
sensitivity?
AGT mutation ?AGT metabolic activity ?level of
endogenous oxalate
Clinical severity
oxalate diet, hydration medication Infec
tion Renal handling oxalate
7
Mrs. A
- Age 22 kidney stone
- ? Hyperoxaluria (5x normal) hyperglycoluria
- Liver biopsy AGT residual activity of 48
- Reduction of hyperoxaluria to high normal
(0.057 mmol/mmol kreat) under pyridoxine 50 mg - Age 38 good health, 1 new stone removed, US
small calcifications
8
Mrs. B, sister of Mrs. A
- Age 6 kidney stones, surgical removal
- Age 30 diagnosis PH1, lost to follow-up
- Age 50 kreat 200 µmol/l, nephrocalcinosis
- Liver biopsy 15 AGT-activity
- Age 51 ESRD
9
Mrs. C, sister of A B
- Age 48 ESRD (1 year after diagnosis B)
- AGT-activity 9
- Age 49 renal tx
- Nephrocalcinosis renal graft
10
Mrs. C, sister of A B
- Age 48 ESRD (1 year after diagnosis B)
- AGT-activity 9
- Age 49 renal tx
- Nephrocalcinosis renal graft
- All 3 sisters homozygous G170R mutation
11
AGT in liver biopsy specimens
O Immunoreactive AGT - immunoreactive AGT
(Danpure ea J Inher Metab Dis 17 487-499, 1994)
12
AGT deficiency over 50 mutations
- liver biopsy
- immunoreactivity enzyme activity
- Protein not synthesized (nonsense m) - -
- Protein synthesized OK but inactive -
- Protein synthesized OK but unstable
- Protein rapidly degraded -
- Protein aggregates /-
- Protein mistargeting mitochondrion
13
Gly82Glu (Pyr-) mutation abolishes pyridoxine
(PLP) binding (imm/enz-) Gly41Arg (Pyr-)
abolishes contact 2 monomers destablilisation?
aggregation AGT
From Zhang et al, JMB, 2003
14
2 polymorphic variants a major minor allele
- Minor allele 4 population Europe/USA
- Normal AGT peroxisomal localisation by way of
Peroxisomal Targeting Sequence 1 as folded dimer - Minor allele P11L aa replacement
- ? catalytic act AGT to 30
- ? dimerisation AGT in vitro at 37
- 5 mitochondrial location AGT by a weak
Mitochondrial Targeting Sequence at N-terminus - Mitochondrial AGT import only as an unfolded
monomer
15
G170R F152I ?? activity of P11L-induced
mitochondrial mistargeting to 90 by unfolding
the AGT
from Danpure et al
16
G170R F152I ?? activity of P11L-induced
mitochondrial mistargeting to 90 by unfolding
the AGT
- pyridoxine may increase the activity of 10
peroxisomal AGT - association pyridoxine sensitivity?
from Danpure et al
17
Association B6 sensitivity - outcome 1. the
Dutch experience
- follow-up PH 1972-2002
- search for patients
- Dutch Registration Renal Replacement Therapy
(RENINE) - Dutch Society of Pediatric Nephrology
- Dutch Society of Nephrology
- if no answer contact by phone
- review of all available medical charts
- Total number of patients 62
- PH1 57 PH2 1
- PH-unidentified 4
- Prevalence PH1 2.9 per 106
- Incidence PH1 0.15 per 106 per year
v Woerden et al, NDT 18, 2003 Kidney Int 66,
2004
18
Age at diagnosis
19
End-stage renal disease at diagnosis
20
Outcome renal function
57
at diagnosis
30 preserved renal function
27 renal insufficiency
19 ESRD
21
Outcome renal function
57
at diagnosis
30 preserved renal function
27 renal insufficiency
19 ESRD
2 improved/ 2 stabilized
4 ESRD
at follow-up
24 preserved renal function
5 ESRD/ low GFR
28 ESRD/ low GFR
11 death
22
Clinical biochemical parameters in relation to
renal insufficiency
RR relative risk, 95CI 95 confidence
interval
23
Mutation analysis patients
- 33/57 patients of 26 families
- Median age onset of symptoms/diagnosis 5.7/6.6
(0.1-50/57) - Mean follow up after diagnosis 12.5 years (0.1-
49) - 20/33 patients onset lt 18th years of age
- 6/33 patients onset lt 1st year of age
24
Mutations
- 11 patients homozygous for G170R - pyr
- 4 patients homozygous for P152I - pyr
- 3 patients homozygous for 33InsC - pyr-
- 3 patients homozygous for G82R - pyr-
- 1 patient homozygous for G170R V336D
- mutation - pyr-
- 11 patients compound heterozygous - pyr-
25
G170R homozygosity (Pyr)
11
at diagnosis
6 preserved renal function
5 ESRD
5 kidney Tx all B6 responsive
1 ESRD (not treated)
at follow-up
5 preserved function
3 preserved function
kidney Tx preserved function
26
F152I homozygosity (Pyr)
4
at diagnosis
2 preserved renal function
2 ESRD
1 kidney Tx B6 responsive
1 dialysis
at follow-up
2 preserved function
1 preserved function
27
33InsC homozygosity (pyr-)
3
at diagnosis
3 neonatal ESRD
1 deceased
2 liver kidney Tx
at follow-up
1 preserved function
1 deceased (liver failure)
28
G82R (pyr-)
3
at diagnosis
3 normal GFR
1 preserved
1 decreased GFR
1 ESRD
at follow-up
1 liver kidney-tx
GFR decreasing
29
Mrs. B, sister of Mrs. A
- Age 6 kidney stones, surgical removal
- Age 30 diagnosis PH1, lost to follow-up
- Age 50 kreat 200, nephroclacinosis
- Liverbiopsy 15 AGT-activity
- Age 51 ESRD
- Follow-up (8 years)
- Same year renal Tx, calcification Tx kidney, GFR
46 at 5 years follow up - Normalisation oxalate excretion under pyridoxine
30
Mrs. C, sister of A B
- Age 48 ESRD (1 year after diagnosis B)
- AGT-activity 9
- Age 49 renal tx
- Nephrocalcinosis graft
- Follow-up (7 years)
- Normalisation oxalate excretion under B6
- GFR graft 56 after 5 years of follow-up
- All 3 sisters homozygous G170R mutation
31
The American experienceMonico et al Am J
Nephrol 2005
- 23 PH1 patients
- 6 homozygotes G170R
- 1 homozygous F152I
- Homozygotes G170R F152I B6 responsive and high
AGT residual act (19 vs.10 heterozygotes G170R
8 non-G170R) - No follow up
- Conclusion association B6 and G170R F152I
32
The German experienceHoppe et al, Am J Nephrol
2005
- Patients 65 PH 42 PH1 12 unclassified
- 7 B6 full response - no mutation found - AGT 7.2
(1 patient) - 9 B6 partial response (25-50)- 4 heterozygous
G170R - AGT 4.7 - Time interval symptoms - diagnosis 1-31 year
- 17 no B6 response - AGT 5.2
- 25 (38) ESRD - 2 homozygous G170R
- 6 isolated kidney tx - 1 successful, 3
recurrences, 2 failed
33
The Israel experienceFrishberg et al Am J
Nephrol 2005
- 56 PH1 patients
- 21 families
- 15 mutations, 1 nonsense, 13 missense mutations
- No B6 responsiveness, AGT-activity near to 0
- Prevalent phenotype early onset CRF
- 20 ESRD childhood (18), 15 at infancy
- Clinical presentation 43 lt age 5
- 12 asymptomatic at diagnosis
34
Conclusions pyridoxine sensitive PH1
- Homozygosity G170R and F152I minor allele,
others? - 20-30 PH1 patients Western Europe/USA
- Relatively late onset adult patients!!
- Diagnosis often delayed
- Good outcome if early diagnosed
- no indication for liver Tx
35
(No Transcript)
36
PH1 group Emma childrens Hospital AMC
Christiaan van Woerden Resident
Paediatrics Simone Denis Technician Hans
Waterham Molecular Geneticist Ronald
Wanders Biochemist Carla Annink Technician
Marinus Duran Clinical Chemist Frits
Wijburg Pediatrician Metabolic Diseases Jaap
Groothoff Pediatric Nephrologist
37
Participating centres
- AN Bosschaart (Enschede)
- WT v Dorp (Haarlem)
- MAGL ten Dam (Nijmegen)
- CFM Franssen (Groningen)
- IH Go (Nijmegen)
- JJ Homan vd Heide (Groningen)
- JP v Hooff (Maastricht)
- F Th Huysmans (Leiden)
- JE Kist-van Holthe tot Echten (Leiden)
- W Koning-Mulder (Enschede)
- G Kolsters (Zwolle)
- MR Liliën (Utrecht)
- S Lobatto (Hilversum)
- LAH Monnens (Nijmegen)
- J Le Noble (Schiedam)
- C Ramaker (Amsterdam)
- EMA vd Veer (Amsterdam)
- ED Wolff (Rotterdam)
- R Zietse (Rotterdam)
38
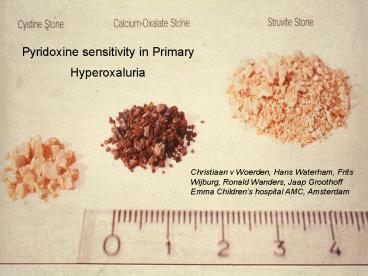
a kidney stone