Cantharidin - PowerPoint PPT Presentation
1 / 36
Title:
Cantharidin
Description:
1. Short Acting Warfarin. 2. Long Acting---Diphacenone, ... and progressive ataxia, paresis, hind leg paralysis, progressive CNS depression and coma. ... – PowerPoint PPT presentation
Number of Views:348
Avg rating:3.0/5.0
Title: Cantharidin
1
Cantharidin
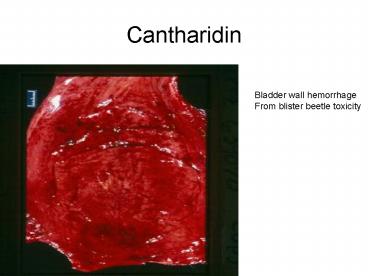
Bladder wall hemorrhage From blister beetle
toxicity
2
Horse Stomach
Blister Beetle poisoning in a young Horse. Multi
ple areas of hemorrhage and Necrosis of the
lining of the stomach
3
(No Transcript)
4
Toxicology 2Rodenticides
- Anticoagulant Rodenticides
- Rat Baits
5
Anticoagulant Rodenticides
- 1. Short ActingWarfarin
- 2. Long Acting---Diphacenone,Bromadiolone,
Pindone - Both short and long acting anticoagulant
rodenticides interfere with Vitamin K1. This
inhibits clotting factor synthesis
6
Signs usually Occur 2-5 days After ingestion
of Toxin. Sign are variable With slow
clotting times
7
Anticoagulant Rodenticides
- Symptoms
- Variable
- Petechiae (small bleeding under the skin)
- Bruising
- Blood in the Urine
- Hematomas
- Respiratory distress
- Paleness
- CNS signs if bleeding is in the brain
8
DiagnosisAnticoagulant rodenticides
- 1. Prolonged Clotting times
- 2. PT (prothrombin times)
- 3. Partial thromboplastin time (PTT)
9
TreatmentAnticoagulant Rodenticides
- 1. Induce emesis
- 2. Give activated charcoal
- 3. Vit K1 (up to 1 month) check PT times off
the medication - 4. Blood Transfusions
- 5. Oxygen Therapy
- 6. Preventing Trauma for several days while on
the antidote..
10
(No Transcript)
11
Vitamin K1 is Antidotal for Coumarin type Of rat
poisons Check the effect of Therapy by
doing Clotting tests PT and PTT
12
Bromethalin Rodenticides
- Bromethalin uncouples oxidative phosphorylation
(severely reducing cellular energy) Although
cells of many organs can be affected, damage to
neurons seems to be responsible for the clinical
signs exhibited by intoxicated animals. - cats are especially sensitive to bromethalin
rodenticides
13
Bromethalin Rodenticides
- Symptoms In high doses we can see acute signs of
- 1. Muscle Tremors
- 2. Hyper excitability
- 3. Vocalization
- 4. Running Fits
- 5. Seizures
- 6. Ataxia
14
Bromethalin Rodenticides
- Signs Cont
- More commonly the toxic syndrome is delayed
(12-24) hours and progressive ataxia, paresis,
hind leg paralysis, progressive CNS depression
and coma.
15
Bromethalin ToxicityDiagnosis
- No antemortem testing is available
- Can only be confirmed at special veterinary
laboratories on necropsy and analysis of kidney,
liver, fat or brain samples
16
Bromethalin Rodenticides
- Treatment (early)
- 1. Induce vomiting (if not seizuring)
- 2. Activated charcoal
- 3. Control cerebral edema, mannitol,
dexamethasone - 4. Anticonvulsive medications
- Prognosis is poor for severely affected animals
17
(No Transcript)
18
Rodenticides PoisoningCholecalciferol (vitamin
D3)
- Available in granules, flakes, tablets, cakes,
and briquettes under a variety of trade names
19
Cholecalciferol (Vitamin D3)Pathophysiologic
findings
- The major toxic effect in cholecalciferol-intoxica
ted animals is hypercalcemia. - Hypercalcemia-induces effects on excitable
tissues and can result in soft tissue
mineralization.
20
CholecalciferolToxicity
- Anorexia
- Weakness
- Depression
- PU/PD
- Vomiting
- /- diarrhea with blood
- Symptoms develop 12-36 hours post ingestion
21
CholecalciferolLaboratory Findings
- 1. Hypercalcemia
- 2. Hyperphosphatemia
- 3. Azotemia
- Necropsy findings Soft tissue mineralization
22
CholecalciferolTreatment
- Treatment is aimed at lowering the serum calcium
- 1. Diuretics (Lasix)
- 2. Prednislone
- 3. IV Saline Solutions .9NACL
- Prognosis is guarded as the Hypercalcemia can
lead to renal failure
23
Zinc Phosphide
- Acutely toxic, onset of poisoning is 15-60
minutes after ingestion - Formulated is a grain-based or scrap bait, paste
of powder - The toxic nature of this product is phosphine
gas, released by the acidic environment of the
stomach - Phosphine gas acts like a general protoplasmic
poison. The gas smells like acetylene gas.
24
Zinc PhosphideSymptoms
- Vomiting
- Aimless running
- Howling
- Convulsions
- Death
25
Zinc PhosphideDiagnosis/Prognosis
- No definable tests exist for live patients
- Post mortems analysis of stomach contents for
Zinc Phosphate - Prognosis guarded, No antidote is available,
Supportative care
26
AcetaminophenTylenol Toxicity
27
PathophysiologyTylenol Toxicity
- CatsThe chemical induces oxidative damage to the
erythrocytes leading to a hemolytic anemia. - Oxidation of heme iron resulting in methemoglobin
production - Methemoglobinemiathe heme iron in hemoglobin is
oxidized from the ferrous (Fe2) to ferric (Fe3)
state and is unable to bind and transport oxygen
28
Tylenol ToxicityPathophysiology
- The methemoglobin can occur minutes to hours
after toxin exposure in cats. - As little as 1 65mg tablet can be toxic to a sick
cat and an extra strength tablet toxic to a
healthy cat.
29
Tylenol ToxicityCats
- Symptoms
- 1. Shortness of breath
- 2. Cyanotic mucous membranes
30
Tylenol ToxicityTreatment
- 1. Oxygen
- 2. Methylene Blue
- 3. N-acetylcysteine (Mucomyst)
31
Aspirin Toxicity
- Primarily seen in cats and immature dogs
- Drugs Benefits
- 1. anti-inflammatory
- 2. anththrombotic
- 3. analgesic
- 4. antipyretic
32
Aspirin
- From Willow Bark (for centuries the bark was
known to have antipyretic (fever effects) - Salicin was the active ingredient in the bark.
- In 1829, sodium salicylate was isolated from
salicin - Bayer first prepared acetylsalicylic acid
(aspirin) which was first marketed around 1900 - Aspirin has a variable ½ life in different
species - The ½ life in dogs is 8 hours, the cat is 38 hours
33
Aspirin
- Aspirin in readily absorbed from the gi tract and
is hydrolyzed to salicylic acid. The salicylate
is later conjugated with glucuronate and glycine
and excreted in the urine. - Cats have a relative deficiency of glucuronate
which accounts for the prolonged elimination of
the drug
34
Aspirin Toxicity
- Symptoms
- Gastritis with focal hemorrhage and metabolic
acidosis - Platelet problems (bruising, bleeding)
35
Aspirin Toxicity
- Treatment
- 1. Induce vomiting
- 2. NaHCO3 for acidosis
- 3. Increase renal production, IV fluids
36
Aspirin ToxicityPrognosis
- GI ulcerations can occur in dogs with long term
usage. - Generally the prognosis is good if treated
aggressively and quickly