HPI - PowerPoint PPT Presentation
1 / 33
Title: HPI
1
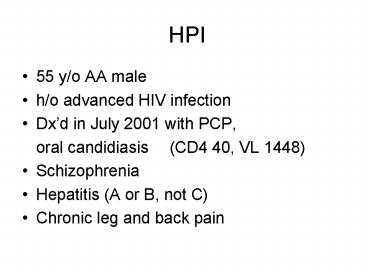
HPI
- 55 y/o AA male
- h/o advanced HIV infection
- Dxd in July 2001 with PCP,
- oral candidiasis (CD4 40, VL 1448)
- Schizophrenia
- Hepatitis (A or B, not C)
- Chronic leg and back pain
2
HPI
- has been in IDSC since August 2001
- Was started on CBV( 3TC AZT) and Efavirenz
- Did not Respond well to therapy but developed
pancytopenia in 5/02
3
HPI
- Regimen was changed to Tenofovir, Kaletra
(Lopinavir/ritonavir), and Stavudine - Responded well to therapy, VL undetectable
- Anemia resolved
4
HPI
- c/o tingling and numbness all extremities after
19 months of starting new regimen - Also c/o fatigue, poor appetite, and weight loss
35 lbs. in 3 months - No N/V, abdominal pain, F/C, night sweats
5
HPI
- Loose stool sometimes
- No h/o cancer in a family
- smokes marijuana occasionally
- NKDA
6
Physical Examination
- VS T 98.2 F P 97 RR 18 BP 118/68
- BW 128 lb
- GA A O x 3, afebrile, NAD, thin but not
cachectic, lipodystrophy of both cheeks - HEENT PERRLA, EOMI, no oral thrush
- LN Small LN at Rt axilla
- Chest CTA bilaterally
7
Physical Examination
- Heart RSR, nl S1, S2, no murmur or
gallops - Abd soft, not tender, BS present,
no organomegaly - Ext no pitting edema, palpable pulses
- Skin no rash
- Neurological examination decrease vibration
sense in both arms and feet
8
Diagnostic data
- CBC
- WBC 9 Hb 13.3 Hct 40.5 Platelet 224
- normal differential
- CMP
- CO2 24 AG 17 TB 1.3
- VL lt 50, CD4 340
- Testosterone, TSH, PSA- WNL
- PPD - negative
9
CT Chest, abdomen, and pelvis
- Mild cardiomegaly with left ventricular
enlargement - Small hiatal hernia
- Mild atherosclerosis
- Splenule
10
Problem Lists
- Weight loss
- Peripheral Neuropathy
11
- What is the etiology ?
12
Diagnostic data
- Lactic acidosis
- 4.9
13
Diagnostic data
- colonoscopy ordered
14
Clinical Course
- Stavudine was changed to Abacavir
- Still has good response to a new regimen
- Peripheral neuropathy- much improved
- Gained 7 lbs in 3 months after Stavudine was
stopped - Lactic acid came down to 4.3 then 3
15
Hyperlactatemia
- Associated with NRTIs
- In the majority of cases
- - transient and occur in the absence of symptoms
- Symptomatic hyperlactatemia is an uncommon
complication - -nonspecific, predominantly GI symptoms,
reproducible elevated lactate levels, hepatic
abnormalities, weight loss, fatigue.
16
Hyperlactatemia
- Slowly resolve over weeks to months upon
discontinuation of NRTI. - The proposed mechanism is mitochondrial toxicity
through inhibition of DNA polymerase gamma
(enzyme responsible for mitochondrial DNA
synthesis) .
17
Hyperlactatemia
- In vitro, the ability to cause mitochondrial
dysfunction is different - zalcitabine gt didanosine gt stavudine gt
zidovudine gt abacavir lamivudine tenofovir
Birkus G, Hitchcock JMH, Cihlar T. Assessment of
mitochondrial toxicity in human cells treated
with tenofovir comparison with other nucleoside
reverse transcriptase inhibitors. Antimicrob
Agents Chemother 2002, 46716723
18
Hyperlactatemia
- ? Reintroduce with the less mitochondrial toxic
NRTIs
19
Peripheral Neuropathy in HIV-infected
patients
- peripheral neuropathy can be
- - a complication of HIV infection
- - a complication of drug therapy
- - or a combination of both
- Most common is a distal, symmetric, predominantly
sensory polyneuropathy.
20
(No Transcript)
21
Peripheral Neuropathy in HIV-infected
patients
- Correlates with the degree of immunocompromise.
- Subclinical neuropathy, detected by
electrophysiologic or pathologic studies, can
occur during asymptomatic HIV infection. - Falling CD4 counts are associated with increasing
abnormalities of peripheral nerve function.
22
Peripheral Neuropathy in HIV-infected
patients
- Although other factors, i.e., aging, and weight
loss, likely also contribute. - Symptomatic neuropathy is uncommon in the early
stages of HIV infection when CD4 counts are gt400.
23
Distal symmetrical polyneuropathy
- Pathogenesis is unknown and may be
multifactorial. - ?Direct infection (HIV in peripheral nerve)
- ?Immunologic reaction to infection
- (macrophage and T cell infiltration of
peripheral nerves and dorsal root ganglia, and
activated cytokines are found in the dorsal root
ganglia)
24
Distal symmetrical polyneuropathy
- Screening blood test
- Liver function tests Vitamin B 12 and
folate levels Thyroid stimulating hormone
assay Blood glucose Blood urea nitrogen
and creatinine Serum protein electrophoresis
and - immunoelectrophoresis RPR
25
Drug-induced PN
- Indistinguishable clinically and
electrophysiologically from HIV-associated distal
symmetrical neuropathy. - Although the hands may be affected more often in
drug-induced cases. - Dose-dependent.
- Increases with the duration of drug exposure.
26
Drug-induced PN
- The onset is typically 7-9 weeks after beginning
therapy. - Associated with nucleoside reverse transcriptase
inhibitors (NRTIs) - - stavudine (d4T)
- - zalcitabine (ddC)
- - to a lesser extent, lamivudine (3TC),
- fialuridine (FIAU), and didanosine (ddI).
27
Drug-induced PN
- Zidovudine (ZDV) is not neurotoxic but causes
myopathy. - Vincristine, (used to treat Kaposi's sarcoma)
- Dapsone ( treat or prevent PCP)
- Thalidomide, INH, and ethambutol
28
Drug-induced PN
- Asymptomatic distal symmetrical polyneuropathy is
not a significant predictor of symptomatic
polyneuropathy. - Thus, the presence of asymptomatic polyneuropathy
currently is not a contraindication to the use of
potentially neurotoxic drugs, if needed.
29
NRTIs-induced PN
- Due to mitochondrial toxicity.
- Phosphorylated NRTIs have azido groups that
compete with thymidine triphosphate as substrates
for mtDNA synthesis.
Dalakas MC. Peripheral neuropathy and
antiretroviral drugs. J Peripher Nerv Syst. 2001
Mar6(1)14-20.
30
NRTIs-induced PN
- The following may help to distinguish NRTIs-
induced PN from HIV-related PN - a) Temporal association of symptom onset
- or rapid worsening of symptoms.
- b) Improvement of symptoms after cessation or
reduction of NRTIs dosage.
Dalakas MC. Peripheral neuropathy and
antiretroviral drugs. J Peripher Nerv Syst. 2001
Mar6(1)14-20.
31
NRTIs-induced PN
- c) Coasting- temporary (2-4 wks) worsening of
symptoms after D/C NRTIs followed by clinical
improvement.
Dalakas MC. Peripheral neuropathy and
antiretroviral drugs. J Peripher Nerv Syst. 2001
Mar6(1)14-20.
32
Treatment
- Exclude or eliminate other cause of PN
- Lower the dose of NRTIs
- Analgesics- NSAIDs, topical capsaicin, narcotics
- Antidepressants
- Anticonvulsants- Neurontin, Tegretol, etc.
Dalakas MC. Peripheral neuropathy and
antiretroviral drugs. J Peripher Nerv Syst. 2001
Mar6(1)14-20.
33
Treatment
- Riboflavin