Patient Characteristics - PowerPoint PPT Presentation
1 / 1
Title: Patient Characteristics
1
Infection and Colonization Among Small Bowel and
Multivisceral Transplant Recipients in
the Thirty-Day Post Operative Period
Jennifer Primeggia, MD Peter Karacki, MD Joseph
Timpone, MD
Department of Medicine, Georgetown University
Hospital, Washington, DC
Georgetown University
Abstract
Results
Discussion
- Patient Characteristics
- Gender 40 Female, 60 Male
- Average age at time of transplant 39
- Comorbid Conditions
- CAD (N2), HTN (N6), DM (N5)
- Hypercoagulable State (N5)
- Type of Transplant Received SB 28 (67)
- MV
13 (31) - SB
Kidney 1(2)
- Infection
- 23 patients with at least 1 infection (55)
- 11 patients with de-novo infection (26)
- Median time to first infection 9.65 days
- Among 23 patients, 35 episodes of infection
were identified - 13 patients 1 episode of infection
- 7 patients 2 episodes of infection
- 3 patients 3 episodes of infection
- Previous studies have demonstrated infection
rates as high as 94 in the first month after
transplant, with blood stream infections noted as
the most common source.3,4 - At GUH, we report an infection rate of 55,
with intra-abdominal collections as the most
common source. - The primary etiology of infection was
bacterial, as was confirmed in previous
studies.3,4 - Gram negative organisms were most commonly
identified as the cause of infection - When gram positive organism were found to cause
infection, they were more likely to be resistant
(ex. MRSA, VRE) - We also observe a colonization rate of 52.
However, culture data was not uniformly obtained
in all patients. - In a subset of patients, we speculate that
colonization with more resistant organisms may
predict future infection, though a larger cohort
is needed to draw more definitive conclusions.
Introduction Over the past 20 years, an
increased number of small bowel transplants have
been performed with improving survival rates.
Overall success of this procedure has been
limited by the high rates of post-operative
infections. Methods At Georgetown University
Hospital (GUH), 42 patients (age gt 16) have
undergone small bowel and multivisceral
transplants between 4/2004 and 11/2008. We
conducted a retrospective chart review to
determine the incidence and characteristics of
bacterial and fungal infections in these patients
in the 30 day post-operative period. Results and
Discussion We report an overall infection rate
of 55 and a colonization rate of 52.
Additionally, 21 of patients demonstrated
neither an episode of infection nor colonization.
Bacteria accounted for majority of infectious
and colonization episodes, compared to yeast.
Gram positives were most commonly identified as
colonizers while gram negatives were most
commonly identified as the cause of infection.
Rates of resistance among organisms that caused
infection include Pseudomonas 21, Enterococcus
65, and S. aureus 88. Additionally, when gram
positives were identified in the setting of
infection, these organisms were more likely to
demonstrate resistance. Finally, for 5 patients,
colonization with a resistant organism preceded
infection with the same organism. Conclusions
These findings demonstrate the complex nature of
infection in this unique patient population and
the need to find an optimal perioperative
antibiotic regimen.
Malabsorption (1)
Trauma (4)
Motility disorder (4)
Re-XPLT (4)
Gardners (3)
Other Congen. Defect (1)
Radiation enteritis (1)
Crohns (5)
Others (5)
Volvulus (1)
Kabuki Syndrome (1)
Short gut 2 to surgery (9)
Ischemia (7)
Table 3. Most common organisms to cause infection
Introduction
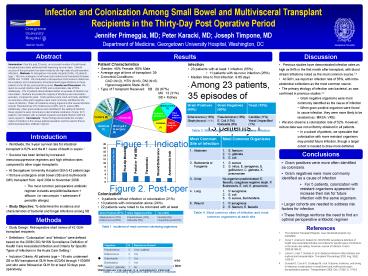
Figure 1. Indication for Transplant
- Worldwide, the 3-year survival rate for
intestinal transplant is 62 and the 1 cause of
death is sepsis.1 - Success has been limited by increased
immunosuppressive regimens and high infection
rates compared to other organ transplants. - At Georgetown University Hospital (GUH) 42
patient (age gt16) have undergone small bowel (SB)
and multivisceral (MV) transplant from April
2004 to November 2008. - The most common perioperative antibiotic
regimen includes ampicillin/sulbactam diflucan
(or vancomycin aztreonam if penicillin
allergic) - Study Objective To determine the incidence and
characteristics of bacterial and fungal
infections among SB and MV recipients in the 30
day post-operative period.
Conclusions
Post-Op Bleeding
Partial or Full SBO
Wound Dehiscence
- Gram positives were more often identified as
colonizers. - Gram negatives were more commonly identified as
a cause of infection - For 5 patients, colonization with resistant
organisms appeared to increase their risk for
future infection with the same organism. - Larger cohorts are needed to address risk
factors for infection - These findings reinforce the need to find an
optimal perioperative antibiotic regimen
Anastomotic leak
Intraadominal Collection
Thrombosis
Figure 2. Post-operative complications
Table 4. Most common sites of infection and most
common organisms at each site
Methods
Table 1. Incidence of most common colonizing
organisms
References
- Study Design Retrospective chart review of 42
GUH transplant recipients - Definitions Colonization and Infection
were defined based on the 2008 CDC/ NHSN
Surveillance Definition of Health Care Associated
Infection and Criteria for Specific Types of
Infections in the Acute Care Setting.2 - Inclusion Criteria All patients (age gt 16) who
underwent SB or MV transplant at GUH from 4/22/04
through 11/30/09 and who were followed at GUH for
at least 30 days post-operatively.
- The Intestinal Transplant Registry.
www.intestinaltransplant.org. 4/20/2009. - Horan T, Andrus M, Dudeck M. CDC/NHSN
surveillance definition of health care-associated
infection and criteria for specific types of
infections in the acute care setting. American
Journal of Infection Control 200836309-32. - Loinaz C, Kato T, Nishida D, et al Bacterial
infections after intestine and multivisceral
transplantation. Transplant Proceedings 2003
Aug 35(5) 1929-30. - Guaraldi G, Cocchi S, Codeluppi M, et al
Outcome, incidence, and timing of infectious
complications in small bowel and multivisceral
organ transplantation patients. Transplantation
2005 Dec 2780(12) 1742-8.
Table 2. Colonizing organisms later involved in
infection