Joe, Jennifer, MD, Verbalis, Joseph, MD - PowerPoint PPT Presentation
1 / 1
Title:
Joe, Jennifer, MD, Verbalis, Joseph, MD
Description:
Hyponatremia is the most common electrolyte abnormality experienced in clinical practice. ... Abnormalities of Water Homeostasis in Aging. Endocrinol Metab ... – PowerPoint PPT presentation
Number of Views:121
Avg rating:3.0/5.0
Title: Joe, Jennifer, MD, Verbalis, Joseph, MD
1
Dangerous Hyponatremia during an URI
Consequences of Routine Hydration Recommendations
Joe, Jennifer, MD, Verbalis, Joseph, MD
Department of Medicine, Georgetown University
Hospital, Washington, DC
Georgetown University
Abstract
Case Description
A 73 y/o healthy, ambulatory white male with
chronic hyponatremia (about 130 mEq/L) presented
to our ER with serum sodium of 117 in the setting
of an acute upper respiratory infection. He was
diagnosed as an acute exacerbation of chronic
syndrome of inappropriate antidiuretic hormone
secretion (SIADH) that responded to fluid
restriction, with an increase in serum sodium
from 117 to 128 over 6 days. Older
individuals, even very healthy ones, are more at
risk for having chronic hyponatremia. General
medical advice commonly given to younger
patients, such as increasing fluid intake for the
common upper respiratory infections should be
made with caution in the older population,
especially those with known chronic SIADH.
PATIENT A 73 y/o healthy white male with chronic
SIADH for 5 years (serum Na130) presented
with constipation. Incidentally, severe
hyponatremia (serum Na 117, Posm240) was
discovered and was the reason he was
hospitalized. With this level of hyponatremia,
the patient was alert and oriented,
conversational, ambulatory, and neurologically
showed only a flat affect with slow and hesitant
speech. The patient reported strictly drinking
only the recommended 2 liters of water a day.
The week preceding his hospitalization, the
patient was treated for an upper respiratory
infection. He was started on a Z-pak and told to
drink more water. The patient reports that he
had faithfully increased his water intake from 2
to 3 liters a day for the week preceding his
hospitalization. HOSPITAL COURSE Initially, 1
L of NS was administered IV in the ER, which did
not change his serum Na. The patient was then
placed on a 1 L/day fluid restriction. The Z-pak
and niaspan were discontinued in the hospital.
The patient had a negative HIV test, normal
Cosyntropin test, normal TSH level, normal renal
and liver function, and normal chest
x-ray. RESULTS With this fluid restriction, the
patients serum Na increased to 128 over 6
days, close to his baseline of 130. With the
increased sodium concentration, the patients
affect became less flat, and he became more
animated and spoke more rapidly.
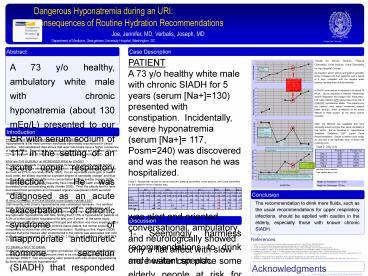
Trends for Serum Sodium, Plasma Osmolality, Urine
Sodium, Urine Osmolality for the Hospital
Course As expected, serum sodium and plasma
osmolality slowly increased with fluid
restriction over a period of 6 days, consistent
with the negative water balance resulting from
the fluid restriction. In SIADH, urine sodium is
expected to be above 30 mEq/L. But as described
in Verbalis Whole-Body Volume Regulation and
Escape from Antidiuresis, both water retention
AND solute losses occur with in CHRONIC
hyponatremic states. This explains why this
patients urine sodium sometimes dropped below
10mEq/L, which is reflective of the bodys
attempt to retain sodium, as the serum sodium
corrected. Often, the literature has suggested
that urine osmolality should be higher than serum
osmolality in true SIADH. But as described in
Hyponatremia Treatment Guidelines 2007 Expert
Panel Recommendations, SIADH is defined more
simply as urine that is not maximally dilute, or
below 100 mOsm/kg H2O.
1 L fluid restriction
Only values that fulfill traditional ideas of
SIADH, where urine Na is greater than 30, and
urine Osm is greater than plasma Osm
Introduction
Expected Sodium Dumping (high urine Na
excretion generally occurs in SIADH)
PREVALENCE OF HYPONATREMIA IN THE
ELDERLY Hyponatremia is the most common
electrolyte abnormality experienced in clinical
practice. Well established data shows that older
individuals have a higher prevalence of
hyponatremia. Depending on the study, prevalence
figures are between 15 and 22 for inpatient and
10.5 and 11 for outpatient elderly (Hodak
2005). WHY are THE ELDERLY at INCREASED RISK for
SIADH? The literature suggests 3 main reasons
that increase the elderlys risk for SIADH.
First, the elderly have altered body composition,
mainly reduced plasma volume, by as much as 21
in one study (Davy 1994). For an equivalent
acute gain or loss of body water, the elderly
experience a greater degree of osmolality change,
and thus more clinically significant shifts in
the concentration of body solutes (Hodak 2005).
Second, kidneys in the elderly frequently have
impaired free water excretion and decreased urine
concentrating ability (Hodak 2005). Third, the
elderly tend to have decreased thirst perception
and increased arginine vasopressin (AVP)
secretion (Hodak 2005). IS MILD CHRONIC
HYPONATREMIA in the Elderly HARMLESS? Until
recently, mild chronic hyponatremia was
considered harmless. In a sentinal paper, Mild
Chronic Hyponatremia is Associated with Falls,
Unsteadiness, and Attention Deficits, Renneboog
(2006) first showed the high association of
asymptomatic hyponatremia with falls, finding
that 21.3 of hyponatremic patients vs. 5.3 of
control had been hospitalized for falls over 3
years. In the same study, Renneboog went further
and showed that gait and attention was more
impaired in the mild hyponatremic patients than
in controls (same patient, but normal sodium),
comparable to worse than mild alcohol
intoxication. Building on this, Kegne (2008)
showed that bone fracture after incidental fall
in the elderly was associated with mild
hyponatremia, unadjusted OR 3.47, 95 Cl
2.09-5.79, and adjusted OR 4.16 95 Cl
2.24-7.71. TO DRINK or NOT TO DRINK Given that
elderly people have a higher prevalence of
hyponatremia, the important question is raised
Do elderly persons need to be encouraged to
drink more fluids (Lindeman 2000)? Can
encouraging older persons with mild chronic
hyponatremia tip them into dangerous hyponatremia?
Table 2 Daily I/Os
Confusing picture as body goes into positive
sodium balance and tries to retain sodium
Escape from antidiuresis (Pt is - 3 liters by Day
6)
Less than 24 hour collection Note negative
about 1L/day
Urine osm is greater than maximamally dilute (ie
greater than 100 mOsm/kg H2O). Definition of
SIADH does not require urine osmolality to be
greater than plasma osmolality (Verbalis 2007)
Table 1 Sequential values for serum sodium,
plasma osmolality, urine sodium, and urine
osmolality for the patients entire hospital stay.
Weight on Admission137.5 lbs Weight on
Discharge138 lbs
Conclusion
The recommendation to drink more fluids, such as
the usual recommendations for upper respiratory
infections, should be applied with caution in the
elderly, especially those with known chronic
SIADH.
Discussion
1- Seemingly harmless recommendations to drink
more water can place some elderly people at risk
for developing hyponatremia. 2- The clinical
manifestations of low sodium can be subtle. In
this case, it was a flat affect and slowed
speech. 3- Chronic hyponatremia is typically
thought of as predominantly due to water
retention. But recent literature (Verbalis 2006)
has also described increased solute losses. This
explains why our patient started retaining
sodium, as reflected by his low urine sodium,
about half way through his hospitalization.
References
- Davy KP, Seals DR. Total blood volume in healthy
young and older men. J Appl Physiol
199476(5)2059-62. - Decaux G. Is Asymptomatic Hyponatreamia Really
Asymptomatic? Am J Med 2006119(7A)S79-S82 - Hodak SP, Verbalis JG. Abnormalities of Water
Homeostasis in Aging. Endocrinol Metab Clin N Am
2005341031-1046 - Kengne GF, Andres C, Sattar L, et al. Mild
hyponatremia and risk of fracture in the
ambulatory elderly. Q J Med 2008101583-588 - Lindeman RD, Romero LJ, Liang HC. Do Elderly
Persons Need to Be Encouraged to Drink More
Fluids? J Gerontol 200055A(7)M361-M365 - Renneboog B, Musch W, Vandemergel X, et al. Mild
Chronic Hyponatremia is Associated with Falls,
Unsteadiness, and Attention Deficits. Am J Med
200611971.e1-71.e8 - Verbalis JG. Whole-Body Volume Regulation and
Escape from Antidiuresis. Am J Med
2006119(7A)S21-S29 - Verbalis JG, Goldsmith SR, Greenberg A, et al.
Hyponatremia Treatment Guidelines 2007 Expert
Panel Recommendations. Am J Med
2007120(11A)S1-S21
Acknowledgments Thank you to Dr. Verbalis, Dr.
Gonin, Dr. Jonklass, and the Georgetown Endocrine
and Nephrology departments.