Chapter 12: GI GramNegative Rods - PowerPoint PPT Presentation
1 / 57
Title:
Chapter 12: GI GramNegative Rods
Description:
Facultative anaerobes; grow well in O2 presence. Contain LPS ... Aerobe/Facultative anaerobe. 2 clinically important species isolated form humans. E. coli ... – PowerPoint PPT presentation
Number of Views:345
Avg rating:3.0/5.0
Title: Chapter 12: GI GramNegative Rods
1
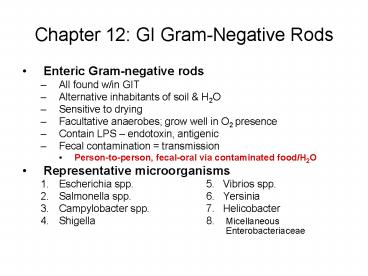
Chapter 12 GI Gram-Negative Rods
- Enteric Gram-negative rods
- All found w/in GIT
- Alternative inhabitants of soil H2O
- Sensitive to drying
- Facultative anaerobes grow well in O2 presence
- Contain LPS endotoxin, antigenic
- Fecal contamination transmission
- Person-to-person, fecal-oral via contaminated
food/H2O - Representative microorganisms
- Escherichia spp. 5. Vibrios spp.
- Salmonella spp. 6. Yersinia
- Campylobacter spp. 7. Helicobacter
- Shigella 8. Micellaneous
Enterobacteriaceae
2
Escherichia
- Family Enterobacteriacea
- Genus Escherichia
- Species Escherichia coli (E. coli)
Escherichia hermani (E. hermani) - General Genus Characteristics
- Gram-negative bacillus
- Escherichia-Shigella DNA homology 70-90
- Aerobe/Facultative anaerobe
- 2 clinically important species isolated form
humans - E. coli
- E. hermani
3
Escherichia
- General Genus Characteristics
- E. coli is the
- Most predominant facultative organism in human LI
- Part of normal flora pathogenic BOTH w/in and
outside GIT - Most frequently isolated enteric bacillus in
clinical laboratory - Subject of more experimental research than any
other organism
4
Escherichia
- Biochemical Cultural Characteristics
- Culture grows well on most media
- Typically ferment sugars
- E. coli ferments lactose (Lac)
- E. coli produces both acid gas during CHO
fermentation - Distinguishing Reactions (IMViC)
- Indol Methyl Red Voges-Proskauer Citrate
- - -
- Structure Physiology of E. coli
- Fimbriae/pili adherence to host mucosal
surfaces - Some strains motile (w/ flagella), others
non-motile (no flagella) - Motile w/ peritrichous flagella (distributed all
over the surface) - All strains are true facultative anaerobes
5
Escherichia
- Structure Physiology of E. coli
- All strains can ferment Glucose
- All strains are oxidase negative (lack enzyme
cytochrome oxidase) - Typing based of differences in 3 antigens O, H
and K - O Ag (somatic or cell wall Ag) part of
polysaccharide portion of LPS are heat-stable - H Ag associated w/ flagella only seen w/ motile
strains (flagellated) - K Ag associated w/ the capsule or, less often,
w/ fimbriae - Ex. E. coli O157H7 causes a severe hemorrhagic
colitis
6
Escherichia
- Pathogenesis
- 6 groups of E. coli strains intestinal
pathogens. - Each group w/ distinct characteristics, but share
the following - Virulence factors found on plasmids
- Interaction w/ intestinal mucosa
- Production of enterotoxins (EXCEPT EPEC)
- Classified w/in specific OH serotypes
7
Escherichia
- Clinical Significance Intestinal Disease
- Transmission m/c person-to-person fecal-oral
route via contaminated food H2O sources - 6 different types of E. coli Intestinal
Infections - Enterotoxigenic E. coli (ETEC)
- Enteroinvasive E. coli (EIEC)
- Enteropathogenic E. coli (EPEC)
- Enterohemorrhagic E. coli (EHEC)
- Enteroaggregative E. coli (EAggEC)
- Enteroadherent E. coli (EAEC)
8
Escherichia
- Enterotoxigenic E. coli
- infection of developing countries (rare in US)
Travelers diarrhea/Infant diarrhea - Transmission thru food H2O contaminated w/
human waste and person-to-person - Colonization of SI via pili
- Vibrio cholera like toxin (choleragen-like
toxin) enterotoxin causes watery diarrhea,
abdominal cramps, low-grade fever. - Prolonged hypersecretion of Cl- and H2O by
intestinal mucosal cells inhibition of Na
reabsorption - Result gut is full of H2O and watery diarrhea
ensues over several days. - Enterotoxin w/ heat-stable (ST) component and
heat-labile (LT) component (Fig 12.4 p. 113)
LT ? AC ? ? cAMP -
ST ? GC ? ? cGMP
9
Escherichia
- Enteroinvasive E. coli (EIEC)
- Endemic in less developed countries
- Inflammatory disease w/in LI
- Penetrates or invades epithelial lining of LI
- Very much like Shigella able to invade
intestinal mucosa, causing dysentery-like illness
(bloody stools mucous, severe abdominal cramps,
fever) - Shiga-like toxin is produced bloody diarrhea
- Def. Dysentery a term applied to various
intestinal disorders, esp. of the colon, marked
by inflammation of the mucous membrane
characterized by abdominal pain, tenesmus, and
diarrhea w/ passage of mucous or blood - Def. Tenesmus spasmodic contraction of anal
sphincter w/ pain and persistent desire to empty
the bowel, w/ involuntary ineffectual straining
efforts)
10
Escherichia
- Enteropathogenic E. coli (EPEC)
- Poorly defined
- Infant diarrhea in developing countries w/ poor
sanitation - Newborn gets infected during birth, or in utero
- Destruction of microvilli of intestinal tract
- Attachment to mucosal cells
- Characteristic lesions produced
- NO tissue invasion NO toxin produced
- Watery diarrhea, fever, vomiting
- Diarrhea can become chronic on rare occasions
11
Escherichia
- Enterohemorrhagic E. coli (EHEC)
- m/c strain E. coli O157H7
- Important epidemic problem in NA, SA, Europe
- Has been associated w/ increasing out-breaks in
U.S. over past 15 -20 yrs. - Transmission to humans from animals via
contaminated raw milk or undercooked meat - NORMAL INHABITANTS OF CATTLE (primary reservoir)
INTESTINES BUT INTESTINES CAN SPLIT OPEN IN
SLAUGHTER-HOUSES, ALLOWING FECAL CONTAMINATION OF
THE MEAT (GETS GROUND IN) - Must thoroughly cook hamburger/ground beef at
160F to kill E.coli pasteurization of milk
kills E. coli
12
Escherichia
- Enterohemorrhagic E. coli (EHEC)
- Bind to cells in LI produce exotoxin (Verotoxin
or Shiga-like toxin) - Attachment to intestinal mucosa (fimbriae)
- NO mucosal invasion of inflammation
- Clinical Disease
- Starts a watery diarrhea w/ abdominal pain (4
days post-exposure) develops into BLOODY
diarrhea (Hemorrhagic Colitis) 1-2 days later. - Recovery complete w/in 10 days
- 10 children lt5 yoa dis. develops into
Hemolytic-Uremic Syndrome (HUS) - Toxin causes direct kidney damage is life
threatening
13
Escherichia
- Enteroaggressive E. coli (EAggEC)
- Infant diarrhea in developing countries
- SA, CA, India
- Aggregate appearance in Hep-2 cells
- Enteroadherent E. Coli (EAEC)
- Cause a dysentery-like syndrome w/ fever and
bloody stools - Persistent watery diarrhea in children HIV pts
14
Escherichia
- Clinical Significance Extraintestinal Disease
- Source of infection is often patients own flora
individuals own E. coli is non-pathogenic in the
intestines. But, it can cause disease. - Urinary Tract Infections (UTIs)
- E. coli m/c cause of UTI, including cystitis
pyelonephritis - females at particular risk
- Uncomplicated cystitis (m/c UTI) d/t
uropathogenic strains of E. coli - Complicated UTI (pyelonephritis) obstructed
urinary flow d/t non-uropathogenic strains. - Neonatal Meningitis
- E. coli m/c cause w/in the 1st month
- Nosocomial infections
- Sepsis/bacteremia, endotoxic shock, pneumonia
15
Escherichia
- Laboratory Indentification/Dx
- Isolation identification
- Lactose fermenter
- Antigenic structure O, K, H antigens
- EIEC may be detected on MacConkey Agar
- EHEC may be detected on MacConkey Sorbitol Agar
- NOTE Lactose-fermenting, Gram-negative rods
(i.e., the Enterobacteriasceae) produce pink
colonies on MacConkey Agar. - - production of acids decrease the pH of agar
acidity causes pH indicator in the agar to turn
pink (fig. 4.8 p. 24) - - inhibits the growth of Gram-positive organisms
and some fastidious Gram-negative bacteria (i.e.,
Neisseria Haemophilus spp.)
16
Escherichia
- Treatment
- Antibiotics NOT recommended for intestinal
disease. Why? to prevent resistant strains - BEST Tx management of fluids electrolyte
balance prevention of dehydration - Let it run its course will eventually get
better - Resistance see with prior hx of antimicrobial
treatment - Prophylaxis recommended for travelers diarrhea
- Active/passive immunization not recommended
17
Salmonella
- Family Enterobacteriaceae
- Genus Salmonella
- Species Salmonella typhi (typhoid fever)
Salmonella enteritidis (GI) - Microscopic Morphological Appearance
- Gram-negative bacilli
- Non-spore formers
- Motile/non-motile
- Growth Conditions
- Non-selective media not fastidious
- Selective media additive bile salts (enterics
survive in gut bile salts) - Facultative anaerobe (survival w/ or w/o O2)
- Mesophile
- Most strains Lac-, and produce acid gas during
fermentation of glucose - Production of H2S
18
Salmonella
- Epidemiology
- Widely distributed in nature
- S. typhi human pathogen only other strains
associated w/ animals food (esp. eggs
poultry) - Mode of transmission fecal-oral
- HIGH RISK GROUPS young children elderly
- Pathogenesis
- Invasion of epithelial cells of SI
- Diseases remain localized or become systemic
(systemic foci)
19
Salmonella
- Clinical Disease (Salmonella infection
Salmonellosis) - Enteric Fever Typhoid Fever
- Disease of reticuloendothelial (lymphatic) system
- Causative agent S. typhi
- Transmission fecal-oral route
- Contaminated water or food
- Carrier food or beverage handler HIGHEST RATE
OF TRANSMISSION - Note carrier can be asymptomatic and shed the
bacteria in the stool bacteria can also hide in
GB
20
Salmonella
- Clinical Disease (Salmonella infection
Salmonellosis) - Enteric fever Typhoid Fever
- Mode of Infection
- Ingestion Acid Tolerance Response (ATR) gene
- ensures bacterial survival in acid pH of stomach
- Adherence/Penetration epithelial lining of SI
Peyers Patches (Lymphoid tiss) - Phagocytosis by Macrophages
- Multiplication Colonization w/in macrophages
(not killed by hydroytic enzymes) ? Primary
Virulence Factor! - ATR gene
- Catalase and superoxide dismutase
- Engulfment by macrophages ? carried to
mesenteric lymph nodes ? fixed macrophages
(liver, spleen and bone marrow) - Transfer from lymphatic system to bloodstream
21
Salmonella
- Clinical Disease (Salmonella infection
Salmonellosis) - Enteric fever Typhoid Fever
- Mode of Infection
- Lysis release of endotoxins cause of initial
sxs - Infectivity organs tissues d/t systemic
bacteremia - Initial Symptoms d/t release of Endotoxin
- Fever, malaise, lethargy, HA, aches and pains
- Later Symptoms continual invasion cyclical
pattern as bacilli enter the bloodstream - Fever - 104F
- Abdominal tenderness and distention
- rose spots maculopapular rash on trunk
chronic bacteremia stage - Diarrhea or constipation
- Vomiting
- Risk Groups Infants Elderly
22
Salmonella
- Clinical Disease (Salmonella infection
Salmonellosis) - Enteric fever Typhoid Fever
- Diagnosis Identification
- Isolation of S. typhi blood, feces, urine, left
over foods - Convalescence/Immunity
- Permanent
- Treatment
- 3rd generation Antibiotic Tx to decrease
febrile illness period - Carriers
- Antibiotic of choice ampicillin
- Administration period 3 months (b/c bacilli in
the macrophages) - Surgical removal of GB (harboring place for the
bacilli)? - Prevention/Control
- Pasteurization of milk
- Pure water supply
- Efficient disposal of sewage
- Sanitary control of food eating places
- Detection isolation of carriers
23
Salmonella
- Clinical Disease (Salmonella infection
Salmonellosis) - Gastroenteritis (enterocolitis)
- Causative agent S. enteritidis
- Transmission Fecal-oral route
- Contaminated food or water
- Carrier food/beverage handler
- Pets chicks/chicken or turtles
- Mode of infection Human infection limited to
lumen of intestine - Ingestion
- Multiplication Colonization lumen of SI
- Inflammation intestinal mucosa
- Cellular endotoxins released when bacteria
autolyse - Cytotoxin inhibits protein synthesis in
intestinal epithelial cells
24
Salmonella
- Clinical Disease (Salmonella infection
Salmonellosis) - Gastroenteritis (enterocolitis)
- Sudden Onset of Symptoms
- HA, chills, abdominal pain
- Later Symptoms
- Nausea, vomiting, watery diarrhea, low-grade
fever - Risk Groups
- Infants and elderly
- Occupational risk slaughter houses
- Diagnosis
- Isolation ID of bacteria from intestinal tract
in stool - Treatment
- Oral rehydration maintain fluid electrolyte
balance (supportive tx) - Antibiotic Tx not recommended, except in extreme
cases - Control/Prevention
- Maintenance of food and water supplies
- Proper refrigeration cooking
- Carrier detection
- Sanitary procedures in slaughter house
25
Shigella
- Family Enterobacteriaceae
- Genus Shigella
- Species Shigella dysenteriae
Shigella flexneri Shigella boydii
Shigella sonnei - NOTE All spp. are primarily pathogens of humans
all cause dysentery in humans - Recall Dysentery serious diarrhea accompanied
by mucus and blood in the stool along w/ severe
abdominal cramping.
26
Shigella
- Microscopic Morphological Appearance
- Gram-negative bacilli
- Non-spore former
- unencapsulated
- Non-motile Shigella has no flagella
- Growth Conditions
- Selective Media thiosulfate citrate bile agar
- Mesophile
- Facultative anaerobe
- NOT fastidious
- Shigella Infection (Shigellosis) sick gut
- Limited to GIT
27
Shigella
- Epidemiology
- Transmission person-to-person contact via
contaminated stools (major) fecal-oral route
flies and contaminated food water - Person-to-person via fecal-oral route by the 4
Fs - Fingers, food, feces, flies
- Shigellosis w/ low infectious dose
- lt200 viable organisms sufficient to cause disease
- S. sonnei causative agent of bacillary
dysentery (HIGHEST ) - S. dysenteriae cause most severe type of
dysentery lowest in US
28
Shigella
- Mode of Infection
- Ingestion (only low 200)
- PERISTALTIC action transfers bacteria from SI ?
LI - Attachment endothelial cells (M cells) that
line intestines attachment stimulates M cells to
phagocytize bacteria - Phagocytosis by macrophages Shigella lyses
macrophages - Multiplication colonization
- Shallow ulcers cell death/necrosis of
epithelial calls - Pseudomembrane formation mixture of cellular
debris, necrotic mucous membrane, bacteria,
fibrin clot formation - Scar Tissue consequence of healing
29
Shigella
- Pathogenesis Toxin production
- Enterotoxin early stages of infection
- Toxic lipopolysaccharide
- Released during autolysis
- Effect irritation of bowel watery diarrhea,
abdominal cramps fever - Exotoxin or Shiga Toxin later stages of
infection - Cytotoxic activity inhibits protein synthesis
get cell death - Effect inflammation of gut wall, local erosion
ulceration degeneration of intestinal villi
30
Shigella
- Early Symptoms (d/t enterotoxin)
- Abdominal cramps, fever, watery diarrhea
- Later symptoms (d/t Shiga toxin)
- Lower abdominal cramps, abundant pus blood in
stool - Recall EHEC produces Shiga-like toxin!
- Risk Groups
- Travelers travelers diarrhea
- Infants pediatric disease (1-10yoa)
- Institutional pts.
- Homosexuals gay bowel syndrome
31
Shigella
- Convalescence/Immunity
- Self-limiting infection recovery in 3-7 days
- Limited immunity
- Diagnosis Identification
- bacterial isolation from feces or intestinal
tract - Treatment for High Risk Groups
- Antibiotic therapy
- Fluid electrolyte replacement/balance
- Prevention/Control
- Sanitary control
- Isolation of pts disinfection of excreta
- Determination of subclinical cases food
handlers - No satisfactory vaccine
32
Shigella Salmonella Summary
33
Campylobacter
- Family Campylobacteriacae
- Genus Campylobacter
- Species Campylobacter jejuni
- Note Camplyobacter is the leading cause of
food-borne disease in US - Microscopic Morphological Appearance
- Gram-negative bacilli
- Curved, spiral, S-shaped or gull-winged pairs
- Motile darting mobility or corkscrew (short
jumping motion) - Microaerophilic require O2, but at lower
than atm - Transmission
- Fecal-oral via contaminated food (esp. poultry)
water supplies
34
Campylobacter
- Epidemiology
- Widely distributed in nature
- Reservoirs mammals and fowl, both wild
domestic - Gastroenteritis (Campylobacteriosis)
- Causative agent C. jejuni
- Infection of intestines causes ulcerative,
inflammatory lesions in jejunum, ileum or colon
bacteremia may occur - Mode of Infection
- Ingestion
- Adherence Multiplication intestinal mucosa of
SI - Enterotoxin or C. jejuni toxin (C.J.T.)
production - Exotoxin raises intracellular levels of cAMP and
stimulates secretory diarrhea - Same mechanism as w/ V. cholerae
35
Campylobacter
- Symptoms
- Malaise
- Fever
- Abdominal pain, painful abdominal cramping
- Watery and bloody diarrhea
- Risk groups
- Most severe in very young elderly malnourished
- Occupational risk - slaughterhouses
- Convalescence/Immunity
- Self-limiting infection in uncompromised pt (1
week) - Therapy recommended to reduce length and severity
of disease
36
Campylobacter
- Diagnosis Identification
- Isolation of bacteria in fecal samples
- Direct examination of fresh feces by dark field
or phase contrast microscopy look for
darting/corkscrew motility (characteristic) - Culture on selective Hektoen agar
- Treatment
- Rehydration electrolyte balance therapy
- Antibiotic therapy
- No vaccines
- Prevention/Control
- Sanitary control of water and milk supplies
- Careful hygiene, esp. avoiding transmission from
animals to food and H2O - Hygienic handling of raw meats
37
Vibrios
- Family Vibrionacea
- Genus Vibrio
- Species Vibrio cholerae Vibrio
parahaemolyticus Vibrio vulnificus - Microscopic Morphological Appearance
- Gram-negative bacilli
- Short, curved, rod-shaped
- Motile vibrating motion single polar flagellum
- Facultative anaerobes that utilize glucose as
source of E
38
Vibrios
- Growth Conditions
- Mesophile b/c infections in humans
- Non-selective media
- Selective media
- V. cholerae alkaline media containing bile (pH
9.0-9.5) thiosulfate citrate bile salts sucrose
(T.C.B.S.) yellow colonies - V. parahaemolyticus V. vulnificus Halophilic
bacteria (marine bacteria pathogens of sea
water found in association w/ seafood) media
supplemented w/ 2-7 NaCl
39
Vibrios
- Epidemiology/Transmission
- Fecal-oral route via contaminated water or food
- No known animal reservoirs
- N. Am. transmission of microbe by food or water
contaminated by carriers - Clinical Disease
- Cholera or Asiatic Cholera
- Acute enterotoxin-mediated infection
- Causative agent V. Cholerae 01 serotype
40
Vibrios
- Clinical Disease
- Cholera
- Mode of infection
- Ingestion large s (104)
- Adherence and Colonization of intestinal mucosa
of LI and SI ONLY organisms attach and
proliferate, but do NOT invade NO penetration
into tissues - Exotoxin Production Virulence of V. cholerae
- Exotoxin Choleragen Primary Virulence Factor!
- Produced by bacteria colonizing the intestinal
tract - Produces heat-labile enterotoxin, composed of 2
protein subunits (AB). - Toxin is bound to intestinal cell receptors by
Subunit B Subunit A then enters the cell and
activates AC
41
Vibrios
- Clinical Disease
- Cholera
- Exotoxin Production
- Choleragen stimulates activity of Adenyl
Cyclase (AC), which converts ATP into cAMP,
increasing of cAMP - ATP ? cAMP enz AC
- Increased cAMP stimulates secretion of chloride
(Cl-) and bicarbonate (HCO3-) ions - Shedding of electrolytes into the intestine is
followed by severe H2O loss from epithelial
cells watery stool - Acidosis d/t loss of HCO3-
- Dehydration d/t loss of fluids
- Increase in blood viscosity d/t fluid loss
- Shock
- Death d/t rapid dehydration and electrolyte
imbalance
42
Vibrios
- Clinical Disease
- Cholera
- Symptoms
- Vomiting
- Large amounts of watery diarrhea or secretory
diarrhea - rice water stools colorless and odorless,
flecks of mucus, epithelial cells and large of
bacteria - Fluid loss 1 L/hr. !!!
- Secondary Symptoms
- Extreme fluid loss, muscle cramps, severe thirst,
sunken eyes, apathy and circulatory involvement
(d/t loss of H20) - Overall Symptom
- Severe dehydration loss of 50 of body wt.
- Risk groups
- Children, weakened/debilitated (elderly)
43
Vibrios
- Clinical Disease
- Cholera
- Convalescence/Immunity
- Unknown
- Repeat attacks w/ different serotypes possible
- Diagnosis
- Usu. dxed by clinical observation look for
bacteria in stools - Stool sample recovery of organisms and growth
on selective alkaline media - Direct fluorescent Ab test on stool
- Treatment
- Prompt replacement of water/fluid and electrolyes
- Antibiotics decrease of bacteria present ?
?toxin production lessen duration volume of
diarrhea - Prevention/Control sewage treatment and H2O
purification
44
Vibrios
- Clinical Disease
- Gastroenteritis
- Causative agent V. parahaemolyticus pathogen
carried by seafood highest rate of transmission
d/t undercooked seafood common in costal sea
waters (10 NaCl) - Causative agent V. cholerae (non 01 serotype)
- Mode of Infection
- Ingestion of raw, partially cooked or
unrefrigerated seafood - Symptoms
- HA, low-grade fever, watery diarrhea, nausea,
vomiting, abdominal cramps - Convalescence/Immunity self-limiting infection
- Prevention/Control cook seafood well proper
refrigeration during transport storage - Outbreaks m/c cause of gastroenteritis in Japan
45
Vibrios
- Clinical Diseases
- Cutaneous Infection
- Causative agent V. parahaemolyticus
V. vulnificus - Both are marine bacteria Halophilic
- Mode of Infection
- Trauma to body site wound or burn
- Symptoms
- Swelling around wound, localized tiss.
involvement - Risk groups
- Occupational risk dock/ship workers, fishermen
- Convalescence/Immunity
- Self-limiting infection
- Treatment
- Antibiotics, possible debridement
46
Yersinia
- Family Enterobacteriaceae
- Genus Yersinia
- Species Yersinia enterolotica enterocolitis
Yersenia pseudotuberculosis
Yersenia pestis (etiological agent of bubonic
plague) - M/c disease in humans infection w/ Y.
enterolitica enterocolitis or gastroenteritis - Bacterium is associated w/ domestic animals
- Transmission to humans via contaminated
foodstuffs or directly from dogs or swine - Often transmitted in milk affect on large s of
people - Typically found in contaminated H2O food,
unpasteurized milk
47
Yersinia
- Microscopic Morphological Appearance
- Gram-negative bacilli
- Motile
- No capsule
- Pathogenesis Clinical Significance
- Infection from ingestion of food contaminated
thru contact w/ domestic animals, or raw meat
(esp. pork) - Result ulcerative lesions in ileum of SI,
necrotic lesions in Peyers patches, and
enlargement of mesenteric lymph nodes (mesenteric
adenitis) - Enterocolitis (Y. enterolitica)
- Characterized by fever, abdominal pain, diarrhea
(sometimes bloody) and HA resolution 1-3 weeks. - When accompanied by LRQ pain/tenderness
leukocytosis clinically indistinguishable from
appendicitis, leading to unnecessary removal of
appendices.
48
Yersinia
- Laboratory Identification
- Bacterium obtained from stool sample
- Isolation by selective media
- MacConkey agar
- Cefsulodin-irgasan-novobiocin
- Identification
- Based on biochemical screening there are gt50
serotypes - Serological testing anti-Yersinia Abs
- Treatment/Prevention
- Measures to limit contamination of meat proper
handling preparation - Antibiotic Therapy to tx systemic involvement
(Septicemia) ONLY
49
Helicobacter
- Family Enterobacteriaceae
- Genus Helicobacter
- Species Helicobacter pylori causes acute
gastritis AND peptic ulcers (duodenal gastric)
unusual ability to colonize the stomach. - Microscopic Morphological Appearance
- Gram-negative bacilli
- Curved or spiral rods
- Multiple polar flagella rapid corkscrew mobility
- Urease positive production of enzyme urease
- microearophilic
50
Helicobacter
- Epidemiology
- Infections are common w/ worldwide distribution
- Transmission thought to be person-to-person b/c
there has been no isolation from food or water - Untreated infections can become
chronic/life-long - Pathogenesis (fig. 12.16 p. 125)
- Colonization of gastric mucosal (epithelial)
cells in stomach also metaplastic gastric
epithelium of duodenum or esophagus - Survival in mucous layer that coats epithelium
causes chronic inflammation attracted to
chemotactic substances hemin and urea - Recruitment activation of inflammatory cells
- Release of Urease cleaves Urea (NH2CONH2),
producing Ammonia (NH3) ions that NUETRALIZE
stomach acid around the microbe. - Ammonia and the H. pylori cytotoxin cause
destruction of mucous-producing gastric cells
(Goblet cells), exposing the underlying CT to
stomach acid ? leads to ucleration (ulcer
formation)
51
Helicobacter
- Clinical
- Initially, acute gastritis w/ possibly diarrhea
lasts 1 week - Infection usu. becomes chronic w/ diffuse,
superficial gastritis epigastric discomfort - Doudenal Gastric Ulcers linked to infection
w/ H. pylori - Complications infection risk factor for
gastric carcinoma gastric B-cell lymphoma
(mucosa-associated lymphoid tumor or MALT)
52
Helicobacter
- Laboratory Identification/Dx
- Serologic tests (ELISA for serum antibodies to H.
pylori) For ELISA discussion, see pp 28-9. - Breath tests for urease
- Pt takes in radioactively labeled urea by mouth.
If microbe present, urease will split the urea to
CO2 (radioactively-labeled and detected upon pt.
exhalation) - NH2CONH2 H2O ? 2NH3 CO2
- Gastric biopsy (endoscopy)
- H. pylori detection from gastric specimens
histological analysis, cultural analysis, test
for urease - Treatment/Prevention
- Combination antibiotic therapy (2 or more Rxs)
53
Opportunistic Enteric Bacilli
- All organisms of Family Enterobacteriaceae
- Organisms collectively of low virulence, but are
opportunistic often nosocomial pathogens - Often present as normal transient inhabitants of
intestinal tract of animals humans, primarily
Large intestine - Some found in water, sewage and soil
- Representative species belong to genera
Enterobacter Klebsiella Serratia and Proteus,
Providencia and Morganella
54
Opportunistic Enteric Bacilli
- Enterobacter spp.
- Motile and Lac
- Cause human disease frequently colonize
hospitalized pts, esp. in association w/
antibiotic tx, indwelling catheters, invasive
procedures. - Can infect burns, wounds, and RT (causes
pneumonia) and UT (UTIs) - 5 clinically important species
- E. cloacae most commonly encountered
- Most frequently isolated form UTIs
- Produces enterotoxins (like E. coli)
- E. aerogenes UTIs
- E. agglomerans
- E. gergoviae
- E. sakazakii neonatal meningitis
55
Opportunistic Enteric Bacilli
- Klebsiealla spp.
- Large, non-motile bacilli, Lac
- Large, mucoid polysaccharide capsule
- Prevents phagocytosis
- Aids in colonization of Respiratory Tract
- Endotoxin Enterotoxin both identified
- 4 clinically important species
- K. pneumoniae m/c member of the genus Primary
Pneumonia - K. oxytoca
- K.ozaenae
- K. rhinoscleromatis
- K. pneumoniae K. oxytoca cause necrotizing
lobar pneumonia in individuals compromised by
alcoholism, diabetes or COPD. - K. pneumoniae also causes UTIs and bacteremia
meningitis
56
Opportunistic Enteric Bacilli
- Serratia spp.
- Motile
- slowly ferment lactose
- Most frequently encountered S. marcescens
- may cause pneumonia, cystitis, UTIs, lower RT
infections - Most clinical infections are of urinary tract or
burns
57
Opportunistic Enteric Bacilli
- Proteus, Providencia and Morganella
- Gram-negative bacilli
- Aerobe/faculatative anaerobe
- closely related members of normal bacterial flora
of bowel (Commensals of LI) - Ubiquitous distribution found in water, soil,
sewage, and intestinal tracts of animals and
humans - 2 clinically important species
- P. mirabilis majority of Proteus infections, gt
90 - P. vulgaris
- In urinary tract causes formation of calculi
(renal stones), UTI - Alkalization of urine damages renal epithelium
- Urease production correlates w/ the severity of
disease - UTIs both nosocomial and community acquired
- Proteus gt only bacteria the characteristically
swarms growth of bacteria takes up entire plate