Gastric Cancer - PowerPoint PPT Presentation
1 / 26
Title:
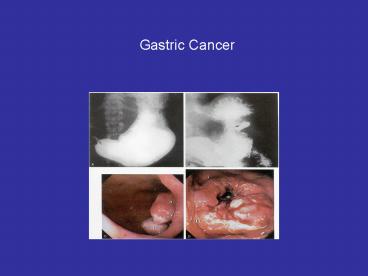
Gastric Cancer
Description:
Adjuvant Therapy for Gastric Cancer. Radiation Therapy: Gastric cancer is ... Adjuvant RT does not increase survival after curative resection. Chemotherapy: ... – PowerPoint PPT presentation
Number of Views:6471
Avg rating:3.0/5.0
Title: Gastric Cancer
1
Gastric Cancer
2
S.M.
70 yo AA man Antrectomy/Vagotomy/BII 1960s for
peptic ulcer disease Right 99 then left 01
lobectomy for primary lung ca Followed for 4
years by endoscopy for benign hyperplastic polyp
distal stomach (proximal to gastrojejunostomy) (l
ast EGD 2 years before current presentation) Seve
ral months wt loss, vague upper abdominal
pain Repeat upper endoscopy reveals ulceration of
previous polyp site, biopsy now positive for
adenocarcinoma CT and PET/CT reveal primary
gastric tumor and hot nodule in lung, but no
clear mets or nodes EUS primary tumor confined
to mucosa
3
Almost total gastrectomy (rim of stomach left
intact at EG junction) and Roux-en-Y
gastrojej Pathology T2b N0 M0 Tumor invades
muscularis propria, not serosa 0/11 LN negative
for tumor No additional therapy for gastric
cancer Scheduled for VATS /- lobectomy
4
R.G.
74 yo C woman Substernal/epigastric
pain Progressed to dysphagia to solids then
liquids 10-15 pound wt loss EGD- ulcerated
lesion gastric cardia, biopsy positive adenoca
with signet ring cell characteristics CT
(chest/abd/pel) diffusely thickened proximal
stomach no mets/involved nodes
5
Exploratory laparotomy reveals leather bottle
stomach extending from the EG junction distally,
involving grossly 80 of the stomach. 2mm
implant in L paracolic gutter positive for
poorly diff adenoca Underwent palliative
radical esophagogastrectomy Pathology T3N2M1
(peritoneal implant) 8/35 LN positive Proximal
(continuous) and distal (noncontinuous) margins
positive Adjuvant chemotherapy
6
L.H.
47 yo AA woman Previous R breast lumpectomy ALND
XRT then completion mastectomy and
chemo Reflux sx, progressive solid food
dysphagia, 20 wt loss EGD 2-3cm ulcerated
lesion gastric cardia Bx positive adenoca w/
signet ring cell features CT chest/abd/pelvis
and PET negative mets- primary tumor contiguous
with tail of pancreas
7
Exploratory laparotomy revealed large
mass cardia, extending posteriorly and
laterally to involve tail of pancreas and left
crus EG junction grossly uninvolved Underwent
resection with total gastrectomy,
distal pancreatectomy, splenectomy with
Roux-en-Y esophagojejunostomy Esophageal margin
positive on frozen section R1 resection Final
pathology?
8
Gastric Cancer Incidence/Epidemiology
- 21,900 new cases 12,200 deaths in United States
in 2003 - Peak incidence 40-70 years old
- 21 MaleFemale ratio
- ? Proximal adenocarcinoma becoming more common
than distal cancers
9
Etiology
- Risk Factors
- Low socioeconomic status
- Fruit/Vegetable poor diet
- Alcohol/Tobacco
- Salt/Smoke food preservation
- Genetics
- HNPCC
- Type A blood
- Precursor Conditions
- Helicobacter pylori
- Chronic atrophic gastritis
- Intestinal metaplasia
- Pernicious anemia
- partial gastrectomy for benign disease
- Gastric adenomatous polyps
10
Classification of Gastric Cancer
- Adenocarcinoma
- 90 of gastric cancer
- Subdivided into 2 types (Lauren Histological
Classification) - Intestinal Type
- More common in areas with high incidence
- Develop in distal third of stomach
- Strongly associated with environmental factors
- Abnormalities of epidermal growth factor
receptors (erbB2, erbB3) - Diffuse Type
- Areas of lower risk/incidence
- Proximal stomach/GE junction (reflux and
Barretts related) - worse prognosis
- Abnormalities of fibroblast growth factors (K-sam
oncogene)
11
Cancer Staging American Joint Committee on
Cancer System
T0- no primary tumor. Tis- Carcinoma in situ. No
invasion of lamina propria. T1-Invasion of lamina
propria or submucosa T2- Invasion of muscularis
propria or subserosa. T3-Penetration of
serosa. T4- Invasion of adjacent structures.
12
Cancer Staging American Joint Committee on
Cancer System
Number of involved lymph nodes critical to
staging. Must sample at least 15 regional nodes.
Location is not important. N1 1-6 regional nodes
N2 7-15 regional nodes N3 gt 15 regional
nodes M1 Distant metastases or involvement of
non regional nodes.
13
5-YEAR SURVIVAL RATES AFTER GASTRECTOMY WITH
COMPLETE (R0) RESECTION (Cancer 2000, 88921-32)
AJCC stage U.S. Japan Japanese-Americans I
A 78 95 95 IB 58 86 75 II 34 71
46 IIIA 20 59 48 IIIB 8 35 18 IV
7 17 5 Overall 28 NR 42
gt 15 lymph nodes resected
14
(No Transcript)
15
Surgical Management Gastrectomy and
Lymphadenectomy
- Need 6 cm margin.
- 10 incidence of tumor margin if only 4-6 cm
gross margin is taken. - 30 incidence of margin if 2 cm gross margin is
taken.
16
Classification Staging of Lymph Node Groups
- Japanese Gastric Cancer Assoc. (JGC)
- N1 1, right paracardial 2, left paracardial
3, lesser curvature 4, greater curvature 5,
suprapyloric 6, infrapyloric. - N2 7, left gastric artery 8, common hepatic
artery 9, celiac artery 10, splenic hilus 11,
splenic artery. - N3 12, hepatic pedicle 13, retropancreatic
14, mesenteric root - N4 15, middle colic artery 16, para-aortic
- Dissection of Stations 1-6 (D1), 1-11(D2), 1-14
(D3), and 1-16 (D4)
17
DOES EXTENDED LYMPHADENECTOMY IMPROVE SURVIVAL?
Study Year Pts 5-yr survival (D1 v.
D2) Kodama/ 1981 850 19 v. 38 Japan Wanebo/ 1
996 18,346 30 v. 26 USA Bonenkamp/ 1999 711
45 v. 46 Netherlands Cuschieri/ 1999 400 35
v. 33 UK Siewert/ 1998 1654 45 v.
47 Germany Jatzko/ 1995 345 25 v.
42 Austria
18
Why are the Results Different?
- Different patient populations and disease
biology, East v. West. - Differences in staging/earlier detection may bias
japanese results
19
Dutch Gastric Cancer Group Trial
- Long term follow-up of largest randomized study
of D1 D2 dissection - 1078 eligible patients, 711 well-matched patients
were randomized to D1 or D2 resection median
follow-up 11 years - In-hospital mortality was 4 D1 group and 10
(p0.004) for D2 group - Univariate analysis of subgroups on selected
prognostic variables (age, pathologic stage,
lymph node stage, total vs partial gastrectomry)
demonstrated no difference in survival rates
between D1 D2 resections
20
Survival Probability (A) and Relapse Risk (B) of
patients (711) treated with curative intent
- Survival rates at 11 years were 30 for D1 and
35 for D2 (p0.53) - Risk of relapse was 70 for D1 and 65 for D2
(p0.43)
Hartgrink et al, J Clin Oncol 222069-2077
21
Survival of patients treated with curative intent
according to N stage. (A) N0 (B) N1 (C) N2 (D)
N3
- D2 dissection did tend to benefit patients with
N2 disease, offering the only possible cure - N2 disease can, at the moment, only be
determined postoperatively after histologic
examination
Hartgrink et al, J Clin Oncol 222069-2077
22
DCG Conclusions
- No long-term overall survival benefit from an
extended lymph node dissection in Western
patients w/ gastric cancer - Associatied higher postoperative mortality may
offset any long-term effect in survival - Extended lymph node dissection may offer cure to
patients with N2 disease but difficult to
identify - Focus should instead be placed on performing a
complete D1 lymphadenectomy, researching new
adjuvant and neoadjuvant protocols and increasing
efficacy of radiation therapy
23
Adjuvant Therapy for Gastric Cancer
- Radiation Therapy
- Gastric cancer is often resistant
- Locally recurrence
- palliation only no survival benefit
- Adjuvant RT does not increase survival after
curative resection - Chemotherapy
- 5-FU provides 20 response rate
- Other drugs with reported activity mitomycin,
cisplatin, doxorubicin, methotrexate, CPT-11,
paclitaxel, taxotere - Meta-analyses of chemotherapy after curative
resection vs resection alone find only modest
survival benefit (see figure)
24
(No Transcript)
25
Adjuvant Chemoradiotherapy
SWOG9008/INT0116 study of adjuvant
chemoradiaiton 556 pts randomized to surgery
alone or surgery adj CRT Gastric resection
with D2 lymphadenectomy recommended 5 days 5-FU
plus leucovorin then 4500 cGy XRT at 180 cGy per
day (5 days/week for 5 weeks) in conjunction
with dose- reduced 2nd and 3rd cycles of chemo
Critics argue 54 of pts underwent less than D1
lymphadenectomy High local (29) and regional
(72) relapse rates in surgery alone
26
Neoadjuvant Chemotherapy
Theorectical Advantages better tolerated,
down-sizing improves resectability,
early treatment of systemic disease Preliminary
results of UK Medical Research Council MAGIC
trial 503 pts stage II and III gastric cancer
randomized to surgery alone or 3 cycles preop
epirubicine, cisplatin, and fluorouracil
(ECF) followed by surgery then 3 additional
post-op ECF cycles Higher proportion of smaller
or T1/T2 tumors resulting in higher
perceived resectability (79 vs 69) based on
surgeons description NOT pathologic R0 vs R1
designation. 2-year survival 48 neoadjuvant
group vs 40 surgery alone (p0.063). Definitive
answers await pathologic data and 5-year survival
results