Pharmacokinetics - PowerPoint PPT Presentation
1 / 47
Title:
Pharmacokinetics
Description:
Rotten egg smell, rapid onset olfactory fatigue. Upper airway & pulmonary irritant ... All anti-anxiety agents have sedative properties, many are anti-convulsants. ... – PowerPoint PPT presentation
Number of Views:730
Avg rating:3.0/5.0
Title: Pharmacokinetics
1
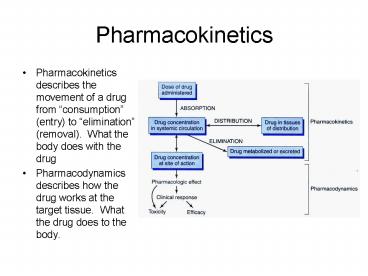
Pharmacokinetics
- Pharmacokinetics describes the movement of a drug
from consumption (entry) to elimination
(removal). What the body does with the drug - Pharmacodynamics describes how the drug works at
the target tissue. What the drug does to the
body.
2
Routes of administration
- The route of administration is determined
primarily by the properties of the drug and the
therapeutic objective. There are two major
routes of administration enteral parenteral. - Enteral
- Oral most common route, most complicated, most
variability first pass metabolism in both the
intestine and liver, gastric emptying
variability, acid lability, enteric coating, etc. - Sublingual Absorption directly into the systemic
circulation, rapid onset and avoids first pass
metabolism in the liver and intestine and the
acidic stomach. - Rectal (just like sublingual) but safer
- Parenteral
- IV avoids first pass effects, it allows the most
control over the circulating level of agent it
is invasive, requires intravenous access once
given IV drugs are difficult to remove (emesis,
charcoal). - IM
- Subcutaneous
- Other
- Topical
- Transdermal allows systemic distribution (vs.
topical), - Inhalation
- Intranasal
3
Paracetamol Absorption by various routes
4
Absorption of Drugs
- A) Transfer of drug from the GI tract
- Passive diffusion is driven by the concentration
gradient. Diffusion depends on lipid solubility,
hydrophilic drugs enter via aqueous channels.
Some passive transport involves a carrier protein
(facilitated diffusion). - Active transport involves a specific carrier
protein. Drugs resembling natural metabolites
are often transported via this energy dependent
mechanism. - Receptor mediated endocytosis
5
Absorption of Drugs
- B) Effect of pH on drug absorption
- Most drugs are weal acids or bases
- Acid HA?H A-
- Base B H ? BH
- Passage of an uncharged drug through a membrane,
movement of drug across the membrane is
proportional to the concentration of charged and
uncharged drug. Manipulation of the pH on either
side can promote drug movement. - Antacids, metabolic acidosis alkalosis may
alter the ratio of charged and uncharged drugs
leading to altered absorption.
6
- C) Physical factors influencing absorption
- Blood flow to the absorption site
- Total surface area available for absorption
- Contact time with the absorptive surface
7
Bioavailability
- A)Bioavailability is the fraction of administered
drug that reaches the systemic circulation this
is expressed as the fraction of drug in the
systemic circulation to drug administered - B) Factors influencing bioavailability
- 1st pass hepatic metabolism
- Drug solubility
- Chemical instability
- Nature of drug formulation
8
Drug Distribution
- Drug distribution is the process by which a drug
reversibly leaves the plasma and enters the
extracellular fluid to reach cells and tissues.
This process depends on - Blood flow to tissue
- Capillary permeability
- Drug solubility
- Degree of drug binding to plasma and tissue
proteins Albumin is the major drug binding
entity and acts as a reservoir of drug.
9
Volume of Distribution
- A hypothetical volume of fluid into which a drug
is distributed, its a useful to consider in
predicting effective drug dosages. - Once absorbed into the plasma a drug can be
distributed to one of three (or all three)
distinct fluid compartments. - Plasma compartment (6 body mass).
- Extracellular fluid (20 body mass).
- Total body water (60 body mass.
- Vd vol. of distribution
- Vd D/C D dose
- C plasma concentration
- Vd has an important influence on the half-life of
a drug because action elimination usually
depends on the amount of free drug at the cell.
10
- Binding of Drugs to Plasma Proteins
- Drugs bound to plasma proteins, usually albumin,
are inactive, only free drug can exert its effect
and be eliminated. - Binding capacity of Albumin
- Drugs bind reversibly to albumin, binding
capacity may be low (11) or high (51).
11
- Phase I reactions
- These reactions convert lipophilic molecules to
more polar molecules by unmasking a polar
functional group (-OH, -NH2, etc.). Phase I
reactions may increase, decrease or leave
unchanged a drugs pharmacologic activity, these
metabolites may be toxic. - Phase I reactions most often involve the
Cytochrome P450 system (MFO) - Drug O2 NADP H?Modified drug H2O
NADPH - Phase II reactions
- These are conjugation reactions. Phase I
reactions are frequently unable to create a
hydrophilic enough molecule for renal excretion.
- Phase II reactions involve conjugation with
glucuronic acid, sulfuric acid, acetic acid or an
amino acids. This usually creates a water
soluble inactive molecule. Glucuronidation is the
most common.
12
Enterohepatic Circulation
Renal Drug Interactions
Bile salts produced in the liver serve to aid in
digestion. 95 of bile acids are reabsorbed in
the ileum, each bile salt is cycled 20 times
before eventually being excreted. Some drugs also
undergo enterohepatic circulation resulting in
prolonged exposure and the production of
potentially toxic metabolites during multiple
passes through this pathway.
Bacterial population
13
Pharmacodynamics what drugs do to you
- Most drugs exert their effects by binding to
receptors the pharmacologic effect is mediated
through drug/receptor binding. - Receptors may be
- Enzymes
- Structures (nucleic acids)
- Membrane receptors
- The drug-receptor complex formation leads to a
biologic response, the magnitude of the response
is proportional to the number of drug-receptor
complexes. - Drug receptor ? drug-receptor ? biologic
effect - Receptors have specificity, they bind a
specifically shaped molecule (or part of a
molecule) but this specificity is not absolute.
The binding of ligand to receptor results in some
change within the cell (transduction). The
consequences of these changes (or lack of
changes) results in the pharmacologic effect of
the drug.
14
Receptor Desensitization
- To protect the cell from potential damage from
extensive stimulation receptors are desensitized
so that more ligand is required for the same
response (tachyphylaxis). - One mechanism involves receptor mediated
endocytosis of chronically activated receptors
endocytosed receptors may be degraded or recycled
to the cell membrane after a delay (insulin). - Graded dose response
- As the drugs concentration increases the
magnitude of the pharmacologic effect increases.
The relationship between dose and response is
continuous more drug ? more response. - Eventually a plateau is attained when
- 1. All receptors are occupied
- 2. For receptors with a large spare population
maximal cellular response is attained.
15
- 1. Potency This measures the amount of drug
necessary to produce an effect of a given
magnitude. A significant contributing factor to
potency is the affinity of a drug for the
receptor. - 2. Efficacy This is dependent on the number of
drug-receptor complexes formed and the efficiency
of coupling of receptor activation to cellular
response. The maximal effect is greater for more
efficacious drugs
16
- Agonists bind to a receptor and produces a
biologic effect that mimics the response of the
endogenous ligand. - Antagonists antagonists bind to the same
receptor as agonists but are unable to elicit
transduction. This binding occupies the receptor
preventing the binding of the endogenous ligand
or agonists thus blocking the drugs effect
(binding may be at the natural ligand binding
site or a different site). - Competitive inhibition When agonists bind
reversibly - Noncompetitive inhibition binding to a
non-agonist site that blocks agonist activity - Uncompetitive Irreversible binding (rare)
- Functional (Physiologic) antagonism When a drug
binds to a separate receptor but the response
opposes the response to an agonist (Epinephrine
bronchial ß2 receptors histamine bronchial H1
histamine receptors
17
- A) Therapeutic Index The therapeutic index of a
drug is the ratio of the dose that produces
toxicity to the dose that produces the desired
response - Therapeutic Index TD50/ED50
- TD50 toxic dose in 50 of patients
- ED50 effective dose in 50 of patients
- The therapeutic index is a sign of a drugs safety
18
Kinetics of Drug Metabolism
- 1st Order Kinetics
- The rate of drug metabolism is proportional to
the concentration of free drug, a constant
fraction is metabolized per unit time - Zero-order kinetics
- A few drugs (ASA, ETOH, Phenytoin) saturate their
catabolic pathways at therapeutic levels. Their
rate of elimination is constant and t1/2 is
dependent on drug concentration
19
Botanicals
- Echinacea (E. purpurea)
- May decrease the incidence /or duration of URI
symptoms when used prophylactically or with early
symptoms. - Caution indicated when used by those with hyper-
or hypo- immune function. - Garlic (Allium sativum)
- Active agent is alliin, converted to allicin
when clove is disrupted (allinase). - Allicin spontaneously degrades to diallyl
disulfide compounds, these are heat labile. - Cardiovascular effects
- 5 reduction in total cholesterol (HMG-CoA
reductase inhibition) - Decreased atherosclerotic plaque volume
- Decreased SBP DBP
- Anti-platelet effects
- Ginkgo (Ginkgo biloba)
- Some protective effect in animal models of
ischemia - Increased pain-free walking in mild-moderate PVD
- No effect in preventing the onset of Alzheimers
disease in a large RPCT.
20
- Milk Thistle (Silybum marianum)
- Silymarins (silybin, silychristin, silydianin)
- In animal models it limits hepatotoxicity from a
variety of toxins - Anti-neoplastic effects in-vitro in some human
tumor cell lines. - St. Johns Wort (Hypericium perforatum)
- Hypericin, hyperforin
- In-vitro causes reuptake inhibition for 5-HT, NE
DA. - Efficacious in mild to moderate depression,
concerns over self treatment. Combined with
prescription reuptake inhibitors may cause
adverse effects. - Induces photosensitivity in some.
- Saw Palmetto
- 5a-reductase inhibitor (blocks testosterone ?
DHT) - More effective than placebo for symptoms of mild
to moderate BPH symptoms. - Does not interfere with PSA monitoring.
21
Heavy Metals
- Arsenic
- Natural contaminant of drinking water
- Organic arsenic found in seafood is easily
excreted and has minimal toxic potential. - Wood preservatives may be a common source (dont
make picnic tables with pressure treated wood). - Impairs cellular respiration
- Pathognomonic skin changes in subacute
chronic exposure - Encephalopathy, respiratory failure, ARF, CV
instability - Lead
- CDC recommends universal screening, average
levels decreasing - Pediatric sensitivity normochromic normocytic
anemia, encephalopathy, cognitive dysfunction, GI
symptoms, renal disease - Reproductive fertility issues.
- Mercury
- 3 types
- Elemental quicksilver, inhalation, flu-like
symptoms, erethism, Parkinsonian symptoms.
- Inorganic batteries, corrosive, absorbed across
the GI tract, GI symptoms, ARF, erethism, CV
collapse
22
- Organic seafood, recommended limited intake of
certain sea food in pregnant, lactating women and
children. CNS effects, maternal exposure
producing CP-like syndrome, seizures, MR. - Cadmium (Zinc)
- Absent in neonates (does not cross placenta and
not excreted in breast milk) - BBB intact to Cd no encephalopathy
- Stored in kidney, liver and testis
- Sources
- Cigarettes 1º 2º smoke
- Cereal grains from herbicides, concentrated in
the germ - Root vegetables
- Water pipes leached by soft water
- Acts like zinc
- Enzyme cofactors
- Produces free radicals
- Acute exposure URI
- Chronic exposure- renal hypertension, renal
lithiasis leading to renal failure
23
Air Pollutants
- Byproducts of the incomplete combustion of
hydrocarbon fuels or contaminants - Implicated in the etiology of respiratory
diseases, cancer, CV disorders - Pre-existing respiratory CV disorders increase
risk - Synergy in effects among agents
- CO
- Binds to Hgb gt200 X O2
- Red dead
- HA, N, V (flu-like syndrome), confusion,
decreased VA, CV instability, coma seizure,
death. - Delayed encephalopathic effects which may not
remit. - Higher metabolic rate indicates greater
sensitivity (kids and pets). - Hyperbaric oxygen chamber for CNS or CV symptoms,
gt25 COHgb - Sulfur Dioxide
- Sulfur dioxide forms sulfurous acid on contact
with moist membranes - Irritant, most deleterious in upper airway,
bronchospasm
24
- Nitrogen oxides
- Deep lung irritant, pulmonary edema acutely
followed by pulmonary fibrosis of bronchioles. - Ozone
- Mucous membrane and lung irritant.
- Produces free radicals
- Direct and secondary lung injury resulting in
chronic bronchitis, bronchioloits and emphysema. - Particulate matter
- Most important predictor of the type severity
of pathology related to particle size smaller
size tends to be more injurious. - Cyanide
- HCN is a common product of combustion of
plastics/petrochemical polymers. - Impairs cytochrome oxidase function leading to
cellular hypoxia - CO cyanide concomitant exposure is common,
suspect in CO poisoning that does not respond
to 100 oxygen.
25
- Hydrogen Sulfide
- Rotten egg smell, rapid onset olfactory fatigue
- Upper airway pulmonary irritant
- Natural sources
- Cytochrome oxidase inhibitor
- Knockdown effect, single breath at 750-1000ppm
can cause unconsciousness and respiratory
depression. - Chloramine
- Bleach ammonia combination
- Contact with mucous membranes produces
hypochlorous acid, ammonia gas and oxygen free
radicals. - Pulmonary irritation, fatalities have resulted
from exposures in enclosed areas (BRs).
26
Pesticides
- Organochlorine pesticides- block axonal
transmission via Na channels - Organophosphates and carbamates block synaptic
transmission through Achesterase inhibition. - OCs- DDT, lipid soluble, Cl stabilizes
- Banned in 1st world, used in 3rd world
(effective, safe, cheap) - OPs carbamates
- Lower ecological toxicity, higher human toxicity
- Reversible Achesterase inhibition (Ops age)
- OP Carbamate Exposure
- SLUDGE plus cramps, fasiculations and seizures if
severe death
27
Ethanol
- Peak plasma levels 30 minutes after ingestion
(binge risk) - 90 metabolized in liver
- Metabolic pathway is usually saturated
(zero-order kinetics)
1. Alcohol dehydrogenase liver, brain stomach
(gt in ?), excess NADH promotes liver damage. 2.
MEOS Cytochrome P450 isoenzyme, inducible,
produces tolerance, excess NADPH promotes liver
damage, promotes metabolism of other drugs. 3.
Aldehyde dehydrogenase inhibited by disulfiram.
28
- Effects of ETOH
- Acute
- CNS Low dose-disinhibition, anxiolytic, impaired
judgment - Moderate dose-dysarthria, dyscoordination
- High dose-emesis, stupor, coma, respiratory
depression, death - Cardiac ? contractility
- Smooth muscle relaxation, vasodilatation
- Chronic
- Liver GI Oxidative stress (?ed reducing
equivalents), cirrhosis, steatosis, hepatitis,
pancreatitis - CNS Withdrawal (agitation, seizures, DTs)
- Toxicity- distal neuropathy, ataxia, dementia,
demyelination - Cardiovascular
- Cardiomyopathy- most common non-ischemic cause,
blocks effects of therapeutic agents - Arrthymias- associated with intoxication
(especially binge) withdrawal - Hypertension- 5 of hypertensives, the most
common remediable cause - Anemia nutritional deficiency, chronic GI loss
- Electrolyte abnormalities
29
- FAS- IUGR, microcephaly, impaired intellect,
facial malformations, jt. abnormalities. FAE-
cognitive impairment (mild-severe) appears dose
dependent. - Immune System- increased in liver pancreas,
decreased in lung and gut - Carcinogenesis
- ETOH-Drug interactions
- CNS depressants synergistic (BZDs)
- Hepatic metabolism (P450 induction, inhibition)
- ETOH in common OTCs
- Cough cold preparations (5-10)
- Mouthwashes (Listerine has 27)
- Flavor extracts contain 10-35 ethanol
30
Toxic Alcohols
- Methanol-sterno, windshield washing fluid
- Same metabolic pathway as ETOH, toxic agent is
formic acid (characteristic visual obscuration
snow storm, bradycardia, acidosis, seizures,
coma). - Ethylene glycol- antifreeze, wine adulterant
- Initial metabolism the same as ETOH, major toxic
agent is oxalic acid forms Calcium oxalate in
renal tubules leading to renal failure. - Treatment Alcohol dehydrogenase has a higher
affinity for ETOH, toxic agents produced are
adequately handled in small amounts. Fomepizole
blocks alcohol dehydrogenase.
31
Spiders, Snakes Animal Toxins
- Snake bites- not all bites of venomous snakes
inject venom - Pit Vipers- rattle snakes, cotton mouth,
- Local damage- proteolytic enzymes,
anti-coagulants - Pain local damage, can have systemic effects
(small body mass), rhabdomyolysis, renal failure,
resp. distress, coagulopathy - Coral Snakes
- Neurotoxin (paresthesias, weakness, CN
abnormalities, fasiculations, lethargy,
respiratory paralysis, death) - Often mild local findings
- Beware of dead snakes
32
- Spiders
- Loxosceles-bite usually involves crushing the
spider - Digestion externale (local necrosis, hemolysis,
coagulopathy, mirco-thrombosis - Immediate local response may progress to local
tissue necrosis over several days, may mimic 3rd
degree burn, decubitis ulcer - Lactrodectus-
- Potent neurotoxin causes uncontrolled release of
Ach NE - Often minor local reaction
- NM symptoms 30 min 6 hrs
- Local muscle spasm, cramps, fasiculations,
weakness, hypertension
33
Fish Toxins
- Ciguatera Fish Poisoning (Ciguatera toxin)
- The most common nonbacterial fish-borne
poisoning Gambierdiscus toxicus is the
dynoflagellate responsible for producing
ciguatera toxin. - Sources
- Amberjack, barracuda, dolphin fish, grouper, sea
bass, sturgeon fish, eel, red snapper, Spanish
mackerel. - Toxicity This toxin is heat stable and
unaffected by cooking temperature or stomach
acid. It is lipid soluble and does not affect
taste, color or odor of the fish. Larger fish
tend to have larger toxin loads. - The mechanism involves direct stimulation of
voltage gated Ca2 channels, phospholipase C and
nonselective cation channels. - The toxin exhibits both bioaccumulation
biomagnification - Presentation
- Onset of symptoms 1 hour -3 days after ingestion,
neurologic symptoms may persist for months. - GI, arthralgia, myalgia, vertigo, CN palsies,
hallucinations, seizures, coma. - CV instability (?HR, ?BP, arrhythmias)
- Resp. bronchospasm, respiratory failure
34
Fish Toxins
- Scrombroid Fish Poisoning (Scombrotoxin)
- Dark meat fish (high levels of histadine) tuna,
mahi-mahi, bluefish, sardines - Normal bacterial flora allowed to grow by
improper storage convert histadine to histamine.
Consumption of histamine results in mild
systemic reaction (flushing, angioedema,
tachycardia, HA, N, V, may induce
bronchoconstrictive effect. - Responds to antihistamines
- Tetrodotoxin
- Puffer fish (fugu)
- Impairs axonal and synaptic transmission
- Perioral paresthesias, muscular paralysis,
respiratory paralysis, death - No antitoxin
35
- Angina
- Stable
- Unstable
- Variant (Prinzmetal) angina
- Anti-anginal drugs
- Organic nitrates (NTG, Isosorbide dinitrate,
etc.) - Mechanism
- ? venous tone (? preload)
- ? arterial tone (?afterload)
- 1 2 result in ? O2 demand
- Coronary artery vasodilation
- Tolerance develops rapidly
- Side effects
- Sublingual NTG should cause a headache (if not
its not dilating) - Potentially bad combination with ED drugs
(Viagra, Cialis, etc.)
36
- Beta- Blockers (block beta-adrenergic receptors)
- Beta 1-antagonists
- Mechanism
- ? HR
- ?contractility
- ? PVR
- Lack of selectivity (ß1 vs. ß2, big problem for
asthmatics) - Abrupt withdrawal creates big problems
- Ca2 Channel Blockers
- Lower myocardial O2 demand by ? BP, ?CO ?
contractility - Nice table on anti-anginals and concomitant
diseases
37
- Anti-hyperlipidemics
- It is desirable to have low LDL, TG total
cholesterol but a high HDL. - Cholesterol levels are determined by endogenous
synthesis and dietary intake. - For any drug treatment to be successful it must
be accompanied by dietary changes - Many cholesterol lowering drugs have secondary
benefits. - Treatment options
- Mild-moderate elevations ? lifestyle
modifications - LDL gt 160 mg/dl with 1 ASCVD (atherosclerotic
cardiovascular disease) risk factor ? drugs - LDL gt 130 mg/dl with 2 ASCVD risk factors ? drugs
- Hypertriglyceridemia
- Niacin
- Fibric acid derivatives
- Anti-lipoprotein therapy
- ? lipoprotein production (these carry TG
cholesterol) - ? lipoprotein degradation
- ? cholesterol absorption (ezetimibe)
- ? cholesterol excretion (bile acid binding resins)
38
- STATINS HMG CoA reductase inhibitors
- Lower cholesterol levels
- Stabilize atherosclerotic plaques
- Improve coronary endothelial function
- Inhibit platelet thrombus formation
- Anti-inflammatory
- Recommended for
- Patients with CAD without hyperlipidemia
- Men with CAD
- Patients with average cholesterol levels without
known CAD - Adverse reactions are rare but serious
- Many of the beneficial effects are independent of
lower cholesterol levels
39
- Anti-hypertensives
- Lowering BP prevents vascular damage associated
with high BP, and the sequelae of that vascular
damage. - ? BP is asymptomatic until a complication (MI,
stroke, renal failure, etc,) develops. - 1/3rd of known ?BP is poorly controlled.
- Diuretics
- Short term ? in intravascular volume (this may
even increase BP) - Long term ? in PVR
- Thiazides- ? Na reabsorption,
- Loop diuretics- ? Na, K Cl- reabsorption,
function via renal PG synthesis - K sparing diuretics
40
- ß-Blockers
- ?BP by ?CO (?hr ?contractility) and ?CNS
sympathetic output (? rennin release
?aldosterone release). - ß1 selective blockers best at ?BP without side
effects of ß2 blockade (bronchiole smooth muscle
contraction) - All ß-Blockers bind to both 12 receptors to some
extent ß1 agents loose their selectivity as
their dose increases. - Acute withdrawal of ß-Blockers can be fatal.
- Ca2 Channel Blockers Second line therapy for
most hypertensives unless there is some
mitigating circumstance that precludes ß-Blocker
use (asthma, DM, PVD, angina) but these are
negative inotropes just like ß-Blockers.
41
- ACE-inhibitors
- Block angiotensin I ? angiotensin II conversion
- Angiotensin II causes
- Vasoconstriction
- Aldosterone secretion
- ADH secretion
- Thirst
- Direct Na and water retention
- These agents also block degradation of bradykinin
- Angiotensin II receptor blockers block all 2
above but not 3
42
Anxiolytics Hypnotics
- All anti-anxiety agents have sedative properties,
many are anti-convulsants. Short acting agents
produce anterograde amnesia. - BZDs (benzodiazepines)
- Open GABA receptor Cl- channels (? Cl- entry)
hyperpolarization of the neuron inhibits action
potential generation - a2 GABA receptor agonists produce antianxiety
effects muscle relaxant effects (via action at
spinal cord level) - a1 GABA receptor agonists produce sedation,
amnesia and anticonvulsant effects - BZDs used for insomnia tend to lack active
metabolites (except flurazepam (Dalmane)). Why? - Tolerance dependence develop quickly to BZDs.
- Withdrawal syndrome
- Very safe, fatal overdoses always involve a
combination with another CNS depressant (ETOH,
Barbiturates, Narcotics, etc.) The safety of
BZDs compared to barbiturates has eliminated
barbiturate use except for seizures.
43
- Non-BZD agents used for hypnotic effects, all
have short t1/2 - Ambien
- Sonata
- Lunesta the only sedative shown to be effective
for 6 months, others create tolerance after 2
weeks and become ineffective for insomnia. - BZD Antagonist
- Flumazenil reverses all BZD effects, very short
t1/2 so treatment of overdose may require
multiple administrations. This agent will produce
an acute withdrawal syndrome
44
- Insulin Oral hypoglycemics
- DM complications
- Macrovascular PVD, CAD, Cerebrovascular
disease - Microvascular Neuropathy, Nephropathy,
Retinopathy - Strict control (Glucose 120-150) is associated
with more frequent hypoglycemic episodes but
clearly significantly delays the onset severity
of DM complications. - Insulin release ? glucose ? ? ATP ? Blocks K
leak from cell ? Cell depolarizes? Ca2 influx ?
Insulin release from vesicles and ? insulin
production - Insulin The goal of insulin therapy is to mimic
both the basal and post-prandial release of
insulin this requires insulins with variable
onsets and durations of effect.
45
- Oral Hypoglycemics
- Insulin sensitizers Biguanides (Metformin)
- Insulin secretogogues
- Sulfonylureas (tolbutamide, glyburide, glypizide)
- Meglitinide analogues
- Glycosidase inhibitors block carbohydrate
degradation in the gut so slows decreases
absorption, obvious side effects. Acarbose. - Incretin therapy (Januvia) a new approach
- Peptide hormones released into the gut lumen when
carbohydrate is consumed stimulate the release of
insulin and block glucagon release, this is why
oral glucose raises blood glucose levels faster
than IV glucose. - Januvia blocks the enzyme that degrades incretins
in the gut so they have a longer duration of
action.
46
- Anti-inflammatory Agents
- Role of prostaglandins in normal and abnormal
function. - Aspirin as a prototype
- NSAIDs have fewer common side effects
- COX-1 COX-2 enzymes
- COX-1 COX-2 inhibitors
47
- Just say know?





















![[PDF] DOWNLOAD FREE Basic Clinical Pharmacokinetics (Basic Clinical Ph PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10075838.th0.jpg?_=20240710028)
![READ [PDF] Basic Pharmacokinetics and Pharmacodynamics: An Integrated PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10075841.th0.jpg?_=20240710029)
![DOWNLOAD [PDF] Biopharmaceutics and Clinical Pharmacokinetics: An Intr PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10075906.th0.jpg?_=20240710041)
![READ [PDF] Biopharmaceutics and Clinical Pharmacokinetics: An Introduc PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10075907.th0.jpg?_=20240711017)
![DOWNLOAD [PDF] Clinical Pharmacokinetics and Pharmacodynamics: Concept PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10076585.th0.jpg?_=20240711027)


![⚡Read✔[PDF] Pharmacokinetics and Pharmacodynamics Research Design and Analysis PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10094589.th0.jpg?_=20240809053)

