Hyperlipidemia Chapter 23 - PowerPoint PPT Presentation
1 / 90
Title:
Hyperlipidemia Chapter 23
Description:
Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults. ... CHD risk directly correlates with TC & LDL levels in graded, continuous fashion ... – PowerPoint PPT presentation
Number of Views:8006
Avg rating:1.0/5.0
Title: Hyperlipidemia Chapter 23
1
Hyperlipidemia Chapter 23
Pharmacotherapy A Pathophysiologic Approach
The McGraw-Hill Companies
2
Abbreviations
3
Overview
- Definition
- Background pathophysiology
- Classification
- Goals of therapy
- Risk factors
- Lifestyle modifications
- Treatment
- Hyperlipidemia in children pregnancy
- Monitoring
- Pharmacoeconomic considerations
4
Hyperlipidemia
- Elevated blood levels of lipoproteins
(cholesterol, triglycerides, phospholipids) - Lipoprotein abnormalities gt 1 of the following
- elevated total cholesterol (TC)
- elevated low-density lipoprotein (LDL)
- elevated triglycerides (TG)
- reduced high-density lipoprotein (HDL)
- National Guideline
- The National Education Program (NCEP) Adult
Treatment Panel III (ATP III) - ?TC, ? LDL, ?HDL reduces mortality/CHD events
Expert Panel on Detection E, and Treatment of
High Blood Cholesterol in Adults. Executive
summary of the third report of the National
Cholesterol Education Program (NCEP) Expert Panel
on Detection, Evaluation and Treatment of High
Blood Cholesterol in Adults (Adult Treatment
Panel III). JAMA 200128524862497.
5
Hyperlipidemia
- CHD risk directly correlates with TC LDL levels
in graded, continuous fashion - gt 50 of American adults total cholesterol gt 200
mg/dL - lt 50 of patients with established CHD are
receiving lipid lowering treatment - Lipid lowering drug therapy reduces risk of
cardiovascular/cerebrovascular events, death
5
Rosamond W, Flegal K, Friday G, et al. Heart
disease and stroke statistics2007 update A
report from the American Heart Association
Statistics Committee and Stroke Statistics
Subcommittee. Circulation 20071156.
6
Hyperlipidemia
- Hypercholesterolemia additive to nonlipid CHD
risk factors cigarette smoking, HTN, DM, low
HDL, electrocardiographic abnormalities - Presence of CHD, prior MI increases MI risk 5 to
7 times - LDL level significant predictor of
morbidity/mortality - 50 of MIs and gt 70 of CHD deaths occur in
patients with known CHD
Menotti A, Lanti M, Nedeljkovic S, Nissinen A,
Kafatos A, Kromhout D. The relationship of age,
blood pressure, serum cholesterol and smoking
habits with the risk of typical and atypical
coronary heart disease death in the European
cohorts of the Seven Countries Study. Int J
Cardiol 2006106157163.
Kannel WB. Range of serum cholesterol values in
the population developing coronary artery
disease. Am J Cardiol 19957669C77C.
7
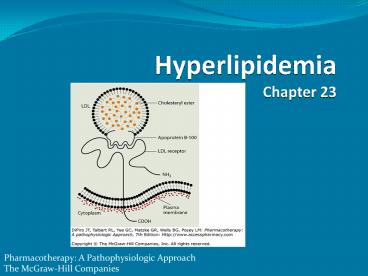
Background Pathophysiology
- Cholesterol essential for cell membrane
formation hormone synthesis - Lipids not present in free form in plasma
circulate as lipoproteins - 3 major plasma lipoproteins
- VLDL carries 10 to 15 of total serum
cholesterol carried in circulation as TG VLDL
TG/5 - LDL carries 60 to 70 of total serum cholesterol
IDL is also included in this group - HDL carries 20 to 30 of total serum cholesterol
reverse transportation of cholesterol
8
(No Transcript)
9
Background Pathophysiology
- VLDL secreted from the liver
- converted to IDL then LDL
- Plasma LDL taken up by receptors on liver,
adrenal, peripheral cells - recognize LDL apolipoprotein B-100
10
Background Pathophysiology
- LDL internalized degraded by these cells
- Increased intracellular cholesterol levels
inhibits HMG-CoA reductase decreases LDL
receptor synthesis - Decreases in LDL receptors plasma LDL not as
readily taken up broken down by cells - LDL also excreted in bile
- joins enterohepatic pool
- eliminated in stool
- can be oxidized in subendothelial space of
arteries
11
(No Transcript)
12
(No Transcript)
13
Background Pathophysiology
- Oxidized LDL in artery walls provokes
inflammatory response - Monocytes recruited transformed into
macrophages - results in cholesterol laden foam cell
accumulation - Foam cells beginning of arterial fatty streak
- If processes continue angina, stroke, MI,
peripheral artery disease, arrhythmias, death
14
Etiology
- Lipoprotein disorders 6 categories based on
phenotype - Specific genetic defects with disrupted protein,
cell, and organ function give rise to several
disorders within each family of lipoproteins - Elevated cholesterol not necessarily familial
hypercholesterolemia (type IIa) - cholesterol may be elevated in other lipoprotein
disorders - lipoprotein pattern does not describe underlying
genetic defect
15
Hyperlipoproteinemia Classification
Fredrickson-Levy-Lees Classification
IDL, intermediate-density lipoprotein LDL,
low-density lipoprotein VLDL, very-low-density
lipoprotein
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
16
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
17
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
18
Etiology
- Many genetic abnormalities environmental
factors lead to lipoprotein abnormalities - Current laboratory values can not define
underlying abnormality - 2 hyperlipidemia should be initially managed by
correcting underlying abnormality when possible
18
19
Lipoprotein Abnormalities 2 Causes
- Hypercholesterolemia
- hypothyroidism
- obstructive liver disease
- nephrotic syndrome
- anorexia nervosa
- acute intermittent porphyria
19
20
Lipoprotein Abnormalities 2 Causes
- Hypercholesterolemia
- medications
- protease inhibitors
- cyclosporine
- mirtazipine
- sirolimus
- progestins
- thiazide diuretics
- glucocorticoids
- ß-blockers
- isotretinoin
21
Lipoprotein Abnormalities 2 Causes
- monocolonal gammopathy multiple myeloma,
lymphoma - acute hepatitis
- systemic lupus erythematous
- Hypertriglyceridemia
- obesity
- DM
- lipodystrophy
- glycogen storage disease
- ileal bypass surgery
- sepsis
- pregnancy
21
22
Lipoprotein Abnormalities 2 Causes
- Hypertriglyceridemia
- medications
- asparaginase
- interferons
- azole antifungals
- mirtazipine
- anabolic steroids
- sirolimus
- alcohol
- estrogens
- isotretinoin
- ß-blockers
- glucocorticoids
- bile acid resins
- thiazides
23
Lipoprotein Abnormalities 2 Causes
- Hypocholesterolemia
- malnutrition
- malabsorption
- myeloproliferative diseases
- chronic infectious diseases
- acquired immune deficiency syndrome
- tuberculosis
- monoclonal gammopathy
- chronic liver disease
23
24
Lipoprotein Abnormalities 2 Causes
- Low high-density lipoprotein
- malnutrition
- obesity
- medications
- isotretinoin
- progestins
- non-ISA ß-blockers
- anabolic steroids
25
Clinical Presentation
- Most patients asymptomatic for years before
disease is clinically evident - Metabolic syndrome gt 3 of the following
- abdominal obesity
- atherogenic dyslipidemia
- increased BP
- insulin resistance glucose intolerance
- prothrombotic state
- proinflammatory state
26
Clinical Presentation
- Symptoms
- none
- severe chest pain, palpitations
- sweating
- anxiety
- SOB
- loss of consciousness
- speech or movement difficulty
- abdominal pain
- sudden death
27
Clinical Presentation
- Signs
- none
- severe abdominal pain
- pancreatitis
- eruptive xanthomas
- peripheral polyneuropathy
- HTN
- BMI gt 30 kg/m2
- waist size gt 40 in (men), gt 35 in (women)
28
Clinical Presentation
- Lab Tests
- ? TC
- ? LDL
- ? TG
- ? apolipoprotein B
- ? C-reactive protein
- ? HDL
29
Patient Evaluation
- Fasting lipid panel every 5 yrs adults gt 20 years
- if patient not fasting only TC HDL are reliable
- TC gt 200 or HDL lt 40 obtain follow-up fasting
lipid panel - Once lipoprotein abnormality confirmed assess
health CV risk factors - Initiate individualized LDL goals treatment
30
Clinical Controversy
- CHD events occur in healthy patients lt LDL goal
- hsCRP inflammatory biomarker, predicts future
vascular events independent of LDL - not currently recommended as a screening tool
- JUPITER study (Justification for the Use of
Statins in Prevention An Intervention Trial
Evaluating Rosuvastatin)
Ridker PM, Danielson E, Fonseca FA, et al.
Rosuvastatin to prevent vascular events in men
and women with elevated C-reactive protein. N
Engl J Med 20083592195-2207.
31
Clinical Controversy
- JUPITER
- rosuvastatin 20 mg vs placebo (n17,802)
- healthy patients with LDL lt 130 mg/dL, hsCRP gt
2.0 mg/dL - average LDL hsCRP reduction by 50 in
rosuvastatin group - Patients in this study would not have qualified
for lipid-lowering therapy according to NCEP
ATPIII - Long-term safety unknown
Glynn RJ, Danielson E, Fonseca FA, et al. A
randomized trial of rosuvastatin in the
prevention of venous thromboembolism. N Engl J
Med 20093601851-61.
Ridker PM, Danielson E, Fonseca FA, et al.
Rosuvastatin to prevent vascular events in men
and women with elevated C-reactive protein. N
Engl J Med 20083592195-2207.
32
Clinical Controversy
- JUPITER combined 1 endpoint MI, stroke, CV
death, arterial revascularization, unstable
angina hospitalization - combined 1 endpoint met early (1.9 years
planned to last 5 years) - substudy evaluated incidence of venous
thromboembolism - patients treated with rosuvastatin had
significantly lower incidence of CV events
symptomatic venous thromboembolism
Glynn RJ, Danielson E, Fonseca FA, et al. A
randomized trial of rosuvastatin in the
prevention of venous thromboembolism. N Engl J
Med 20093601851-61.
Ridker PM, Danielson E, Fonseca FA, et al.
Rosuvastatin to prevent vascular events in men
and women with elevated C-reactive protein. N
Engl J Med 20083592195-2207.
33
Classification
All values are mg/dL
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
34
Risk Factorsa
aDiabetes regarded as coronary heart disease
(CHD) risk equivalent. bHDL cholesterol gt60 mg/dL
counts as "negative" risk factor its presence
removes one risk factor from the total count.
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
35
Treatment Goals
- LDL predicts morbidity, mortality
- 1 treatment target
- More CHD risk factors or higher Framingham Global
Risk Score more stringent LDL goal
36
Goals Cutpoints
aSome authorities recommend use of LDL-lowering
drugs in this category if LDL cholesterol lt100
mg/dL cannot be achieved by therapeutic lifestyle
changes (TLC). Others prefer to use drugs that
primarily modify triglycerides and high-density
lipoprotein, e.g., nicotinic acid or fibrates.
Clinical judgment also may call for deferring
drug therapy in this subcategory. bAlmost all
people with 01 risk factor have a 10-year risk
lt10 thus,10-year risk assessment in people with
01 risk factor is not necessary.
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
37
Hyperlipidemia in Children
- Guidelines/goals of therapy different from adults
- NCEP does not provide cut points for TGs or HDL
in children adolescents - American Heart Association considers TG gt 150
HDL lt 35 abnormal for children/adolescents - Children should receive fasting lipid profile
after age 2 but no later than 10 years if - family history of dyslipidemia or premature CVD
- unknown family history
- overweight, DM, HTN, smoker
Daniels SR, Greer FR and the Committee on
Nutrition. Lipid Screening and Cardiovascular
Health in Childhood. Pediatrics
2008122198208.
38
Lipid Level Classification
- Children adolescents (age lt 20 yrs)
- acceptable
- TC lt 170 mg/dL
- LDL lt 110 mg/dL
- borderline
- TC 170-199 mg/dL
- LDL 110-129 mg/dL
- elevated
- TC gt 200 mg/dL
- LDL gt 130 mg/dL
American Academy of Pediatrics. National
Cholesterol Education Program report of the
expert panel on blood cholesterol levels in
children and adolescents. Pediatrics. 199289(3
pt 2)525-584
Daniels SR, Greer FR and the Committee on
Nutrition. Lipid Screening and Cardiovascular
Health in Childhood. Pediatrics
2008122198208.
39
Hyperlipidemia in Children
- Implement healthy lifestyle/diet in all children
gt 2 yrs - low-fat dairy products in children gt 1 year who
are overweight or family history of obesity,
dyslipidemia, CVD - Drug therapy not recommended age lt 8 years
- exception LDL gt 500 mg/dL such as seen in
homozygous familial hypercholesterolemia - Statins safe effective in children BARs,
absorption inhibitors may also be used
Daniels SR, Greer FR and the Committee on
Nutrition. Lipid Screening and Cardiovascular
Health in Childhood. Pediatrics
2008122198208.
40
Hyperlipidemia in Children
- Pharmacologic intervention considered in patients
age gt 8 years after failure of dietary therapy
when - LDL gt 190 mg/dL if no additional risk factors
- LDL gt 160 mg/dL if family history or gt 2
additional risk factors - LDL gt 130 mg/dL if patient has diabetes mellitus
Daniels SR, Greer FR and the Committee on
Nutrition. Lipid Screening and Cardiovascular
Health in Childhood. Pediatrics
2008122198208.
41
Lifestyle Modification
- Initial treatment for any lipoprotein disorder is
TLC (Therapeutic Lifestyle Changes) - restricted total fats, saturated fats,
cholesterol intake - modest increase in polyunsaturated fat
- increased soluble fiber intake
- exercise moderate intensity 30 min/day most days
- caution in high risk patients or those with CAD
- weight reduction (initial goal of 10) if needed
- smoking cessation
- treat HTN
42
TLC Dietary Recommendations
aCalories from alcohol not included. bComplex
carbohydrates (whole grains, fruits, vegetables).
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
43
Treatment
- Most patients should receive 3 month TLC trial
before initiating pharmacologic therapy unless
very high risk - If patient unable to reach goals with TLC alone
choose lipid-lowering drugs based on lipoprotein
disorder - Combination therapy may be necessary
- monitor closely increased risk of drug
interactions, adverse effects
44
Kastelein JJ, Akdim F, Stroes ES, et al.
Simvastatin with or without ezetimibe in familial
hypercholesterolemia. N Eng J Med
20083581431-1443.
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
45
Recommended Drug Treatment
aBile acid resins (BARs) not 1st line if TGs are
elevated at baseline hypertriglyceridemia may
worsen with BAR monotherapy. bFibrates
gemfibrozil, fenofibrate
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
46
HMG-CoA Reductase Inhibitors
- Lovastatin, pravastatin, simvastatin,
fluvastatin, atorvastatin, rosuvastatin - Inhibit HMG-CoA conversion to mevalonate
- rate limiting step in cholesterol synthesis
- Most potent TC/LDL lowering agents
- Dose dependent decrease in TC/LDL
- averages gt 30 when used with dietary therapy
- Short t½ except atorvastatin, rosuvastatin
- may account for higher atorvastatin
rosuvastatin potency
47
(No Transcript)
48
(No Transcript)
49
HMG-CoA Reductase Inhibitors
- Dosed once daily in evening
- hepatic cholesterol production peaks at night
- exceptions atorvastatin, rosuvastatin
- Rosuvastatin requires dosage adjustment in severe
renal impairment hepatic disease - Good compliance rate, low incidence of adverse
effects - Adverse effects
- elevated serum transaminases, myalgia, myopathy,
rhabdomyolysis, flu-like symptoms, mild GI
disturbance
50
Statin Pharmacokinetics
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
51
Bile Acid Resins
- Colestipol, cholestyramine, colesevelam
- Bind intestinal bile acid
- increase fecal bile excretion
- stimulate bile acid synthesis from cholesterol
- upregulate LDL receptors
- Normally 2nd-line agents when statins not
sufficient or not tolerated - May aggravate hypertriglyceridemia
- caution if TG gt 200 mg/dL
- contraindicated if TG gt 400 mg/dL
52
Bile Acid Resins
- Adverse effects
- GI distress, constipation
- titrate slowly, increase fluid intake, increase
dietary bulk, add stool softeners - hypernatremia, hyperchloremia
- impair fat soluble vitamin absorption
- A, D, E, K
- reduce bioavailability of other medications
- warfarin, levothyroxine, digoxin
- dose 6 hrs from other medications to avoid
interactions
53
Bile Acid Resins
- Low doses well-tolerated
- Often used in combination with other drugs
- With proper counseling dose titration many
patients tolerate higher doses - Tablet formulation may increase palatability
however, tablets are large - Mix powder with liquids or food such as orange
juice, oatmeal, applesauce - Colestipol odorless, tasteless
54
Nicotinic Acid/Niacin
- IR, SR, ER formulations
- OTC Rx (Niaspan)
- Decreases LDL TG
- Increases HDL
- May exacerbate gout DM
- monitor closely
- slow dose titration
- Contraindications active liver disease, severe
gout - Combination with statin or gemfibrozil therapy
increases myopathy risk
55
Nicotinic Acid/Niacin
- Adverse effects
- cutaneous flushing, itching
- ASA 325mg 30 min prior
- titrate dose slowly, avoid spicy foods/hot
beverages - GI intolerance
- acanthosis nigricans (marker for insulin
resistance) - elevated LFTs, hyperuricemia, hyperglycemia
- niacin associated hepatitis
- more common with SR
56
Clinical Controversy
- CETP (cholesterol ester transfer protein)
inhibition leads to elevation in HDL levels - The CETP inhibitor torcetrapib substantially
increased HDL decreased LDL - Torcetrapib resulted in increased BP CHD events
- Unknown whether lack of efficacy due to mechanism
of action or chemical specific events - Other means of raising HDL are being researched
tested
57
Fibric Acids
- Gemfibrozil, fenofibrate, clofibrate
- Reduce TG
- May result in concurrent increase in LDL
- TC remains fairly unchanged
- May increase HDL gt 10 to 15
- 20 to 25 LDL reduction in patients with
heterozygous familial hypercholesterolemia - Efficacy depends on lipoprotein type, baseline TG
58
Fibric Acids
- Gemfibrozil dosed BID 30 min before meals
- Fenofibrate can be taken without regards to food
- CI in renal failure
- Combination therapy with niacin or statins
increases risk of muscle toxicity
59
Fibric Acids
- Adverse effects
- GI complaints, rash, myalgia, headache, fatigue
- transient increase in transaminase alkaline
phosphatase - gallstones (clofibrate)
- enhanced hypoglycemic effects in patients on
sulfonylureas - may potentiate effects of oral anticoagulants
- monitor PT/INR closely in patients on
anticoagulants
60
Absorption Inhibitor
- Ezetimibe
- Inhibits cholesterol absorption across the gut by
23 to 50 hepatic LDL synthesis upregulation
partially offsets impaired absorption - Often used in combination with statins, other
drugs - Dosed once daily without regard to meals
- 18 LDL reduction
- Effect of ezetimibe on CV morbidity mortality
unknown
61
Clinical Controversy
- ENHANCE trial (Ezetimibe and Simvastatin in
Hypercholesterolemia Enhances Atherosclerosis
Regression) - Familial hypercholesterolemia patients
- autosomal dominant LDL receptor mutation
- severely elevated LDL
- premature atherosclerosis
- 2 groups (n720)
- simvastatin 80 mg placebo
- simvastatin 80 mg ezetimibe 10 mg
Kastelein JJ, Akdim F, Stroes ES, et al.
Simvastatin with or without ezetimibe in familial
hypercholesterolemia. N Eng J Med
20083581431-1443.
62
Clinical Controversy
- ENHANCE 1 outcome change in carotid
intima-media thickness (CIMT) after 24 months - no significant difference in CIMT between groups
- simvastatin ezetimibe group greater decreases
in LDL C-reactive protein - No differences in elevated liver enzymes,
myopathy - Limitations prior lipid-lowering therapy (many
patients had near normal CIMT at initiation) not
designed to evaluate differences in incidence of
vascular events
Kastelein JJ, Akdim F, Stroes ES, et al.
Simvastatin with or without ezetimibe in familial
hypercholesterolemia. N Eng J Med
20083581431-1443.
63
Clinical Controversy
- SEAS (Simvastatin and Ezetimibe in Aortic
Stenosis) - Simvastatin 40 mg ezetimibe 10 mg vs placebo
(n1873) - No change in clinical course of aortic stenosis
- Simvastatin ezetimibe increased incidence of
cancer - SHARP IMPROVE-IT trials in progress
- evaluating ezetimibe for vascular risk reduction
- interm analyses do not show increased cancer risk
Peto R, Emberson J, Landray M, et al. Analyses of
cancer data from three ezetimibe trials. N Eng J
Med 20083591357-1366.
Rosseb? AB, Pedersen TR, Boman K, et al.
Intensive lipid lowering with simvastatin and
ezetimibe in aortic stenosis. N Eng J Med
20083591343-1356.
64
Omega 3 Fatty Acids
- Diets rich in omega 3 fatty acids from oily fish
decrease TC, TG, LDL, increase HDL decrease CV
events - Rx fish oil Lovaza
- lowers TG 14 to 30
- raises HDL 10
- FDA approved as dietary adjunct for very high TG
levels (gt 500 mg/dL) - Thrombocytopenia, bleeding disorders potential
complication of high doses
65
Omega 3 Fatty Acids
- lt 3 g/day generally recognized as safe
- Until further research is done on nutraceuticals
it is recommended that patients get dietary EPA
DHA - 2 to 4 g of EPA DHA may be used for very high
TG - Adverse effects
- GI disturbance
- fishy aftertaste
- increased bleeding risk
- worsening glycemic control
- increased LDL
- abnormal LFTs
66
Hypertriglyceridemia
- Lipoprotein types I, III, IV, V associated with
hypertriglyceridemia - Exclude 1lipoprotein disorders underlying
diseases prior to implementing therapy - TLC
- achieve desirable body weight
- diet low in saturated fat, cholesterol
- regular exercise
- smoking cessation
- alcohol restriction
67
Hypertriglyceridemia
- Non-HDL total cholesterol HDL
- LDL VLDL
- 2 target when TG gt 200 mg/dL
- goal
- 30 mg/dL higher than LDL
- normal VLDL 30 mg/dL
Expert Panel on Detection E, and Treatment of
High Blood Cholesterol in Adults. Executive
summary of the third report of the National
Cholesterol Education Program (NCEP) Expert Panel
on Detection, Evaluation and Treatment of High
Blood Cholesterol in Adults (Adult Treatment
Panel III). JAMA 200128524862497.
68
Hypertriglyceridemia
- Borderline-high TGs CHD risk factors
- family history of premature CHD
- concomitant LDL elevation or low HDL
- genetic forms of hypertriglyceridemia associated
with CHD - familial dysbetalipoproteinemia
- familial combined hyperlipidemia
- consider initiation of niacin
- caution in DM patients
69
Hypertriglyceridemia
- Alternatives therapies
- gemfibrozil
- statins
- modest TG reduction HDL elevation
- higher doses may reduce HDL, LDL, TGs
- related to baseline concentration, dose
- fish oil
- fibrates
- may increase LDL
- monitor carefully with borderline-high
triglyceridemia
70
Hypertriglyceridemia
- Very high TGs (gt 500 mg/dL) associated with
pancreatitis - TG gt 500 mg/dL genetic form of
hypertriglyceridemia often coexists with other
causes (e.g. DM) - dietary fat restriction (10 to 20 of calories)
- weight loss
- alcohol restriction
- treat coexisting disorders
71
Hypertriglyceridemia
- Medications for TG gt 500 mg/dL
- gemfibrozil preferred in diabetics
- niacin
- higher-potency statins atorvastatin,
rosuvastatin, simvastatin - fenofibrate may be preferred in combination with
statins - does not impair glucuronidation
- minimizes potential drug interactions
- Successful treatment TG lt 500 mg/dL
Expert Panel on Detection E, and Treatment of
High Blood Cholesterol in Adults. Executive
summary of the third report of the National
Cholesterol Education Program (NCEP) Expert Panel
on Detection, Evaluation and Treatment of High
Blood Cholesterol in Adults (Adult Treatment
Panel III). JAMA 200128524862497.
72
Low HDL-C
- Low HDL strong independent CHD risk predictor
- ATP III low HDL-C lt 40 mg/dL
- No specific goal for HDL-C raising
- Causes of low HDL
- insulin resistance
- physical inactivity
- type 2 diabetes mellitus
- cigarette smoking
- very high carbohydrate intake
- certain drugs
73
Low HDL-C
- LDL remains ATP III 1 target
- ATP III recommendations
- weight reduction
- increased physical activity
- smoking cessation
- drug therapy
- fibric acid derivatives
- niacin
- potential for greatest HDL increase
- effect more pronounced with regular or IR forms
than SR
Expert Panel on Detection E, and Treatment of
High Blood Cholesterol in Adults. Executive
summary of the third report of the National
Cholesterol Education Program (NCEP) Expert Panel
on Detection, Evaluation and Treatment of High
Blood Cholesterol in Adults (Adult Treatment
Panel III). JAMA 200128524862497.
74
Diabetic Dyslipidemia
- Characterized by hypertriglyceridemia, low HDL,
minimally elevated LDL - DM ATP III CHD risk equivalent
- Small, dense LDL (pattern B) in DM patients is
more atherogenic than larger, more buoyant LDL
(pattern A) - 1target LDL
- Goal of treatment LDL-C lt 100 mg/dL
- LDL gt 130 mg/dL TLC drug therapy often
required - Statins often considered initial drugs of choice
Expert Panel on Detection E, and Treatment of
High Blood Cholesterol in Adults. Executive
summary of the third report of the National
Cholesterol Education Program (NCEP) Expert Panel
on Detection, Evaluation and Treatment of High
Blood Cholesterol in Adults (Adult Treatment
Panel III). JAMA 200128524862497.
75
Diabetic Dyslipidemia
- Collaborative Atorvastatin Diabetes Study (CARDS)
- LDL lowering for 1 CHD prevention in type 2 DM
- Randomized, double-blinded placebo controlled
- Atorvastatin 10 mg/day versus placebo (n2,838)
diabetes to reduce first CHD events - Baseline LDL 118 mg/dL LDL ? 46 mg/dL with
atorvastatin
Colhoun HM, Betteridge DJ, Durrington PN, et al.
Primary prevention of cardiovascular disease with
atorvastatin in type 2 diabetes in the
Collaborative Atorvastatin Diabetes Study
(CARDS) Multicentre randomised
placebo-controlled trial. Lancet
2004364685696.
76
Diabetic Dyslipidemia
- CARDS trial 37 reduction in composite 1end
point - 1 endpoint acute CHD death, nonfatal MI,
hospitalized unstable angina, resuscitated
cardiac arrest, coronary revascularization, or
stroke - Suggests diabetics should have target LDL much
lower than 100 mg/dL
Colhoun HM, Betteridge DJ, Durrington PN, et al.
Primary prevention of cardiovascular disease with
atorvastatin in type 2 diabetes in the
Collaborative Atorvastatin Diabetes Study
(CARDS) Multicentre randomised
placebo-controlled trial. Lancet
2004364685696.
77
Elderly Patients
- More susceptible to adverse effects of
lipid-lowering drug therapy - Start with lower doses, titrate slowly to
minimize adverse effects - Risks or benefits from cholesterol reduction not
well defined
78
Women
- Cholesterol important CHD determinant
- relationship not as strong as for women as men
- HDL may be more important predictor of disease in
women - No apparent difference between men women in
LDL/HDL genetic regulation
79
Hyperlipidemia in Pregnancy
- TC TG levels increase throughout pregnancy
- average cholesterol increase 30 to 40 mg/dL
around weeks 36 to 39 - TGs may increase as much as 150 mg/dL
- Drug therapy typically not initiated/continued
during pregnancy - TLC is the mainstay but BARs absorption
inhibitors may be considered in high risk
patients - ezetimibe category C
- Statins category X
80
Children
- Drug therapy not recommended age lt 8 yrs
- Different guidelines, goals
- Bile acid sequestrants 1st-line in the past
- GI adverse effects limit use
- New evidence shows statins are safe effective
in children - greater lipid lowering than BAR
- severe forms may require more aggressive
treatment - e.g., familial hypercholesterolemia
Daniels SR, Greer FR and the Committee on
Nutrition. Lipid Screening and Cardiovascular
Health in Childhood. Pediatrics
2008122198208.
81
Concurrent Disease States
- Nephrotic syndrome, end-stage renal disease,
nephrotic syndrome, HTN compound dyslipidemia
risks - may be difficult-to-treat
- Nephrotic syndrome lipoprotein metabolism
abnormalities - elevated TC, LDL-C, lipoprotein(a), VLDL, TGs
- Statins reduce TC LDL-C in nephrotic syndrome
- levels do not usually return to normal
- may slow declining renal function
82
Concurrent Disease States
- Renal insufficiency without proteinuria
hypertriglyceridemia, slightly elevated TC
LDL-C, low HDL - Polyunsaturated fatty acids may slow pregression
of renal disease CV complications - Bile acid sequestrants do not correct lipid
abnormalities seen in renal insufficiency
83
Concurrent Disease States
- Lovastatin or its active metabolite may
accumulate in renal insufficiency, use lower
doses to avoid adverse effects - Treat CKD patients to LDL goal lt 100 mg/dL
- lowering LDL to lt 70 in high risk patients not
supported by clinical trials
84
Clinical Controversy
- Atorvastatin 20 mg/day vs placebo (n1,200) in
diabetic patients on hemodialysis - No significant difference in 1 endpoints
(cardiovascular death, non-fatal MI, stroke) - Significantly greater risk of fatal stroke in
atorvastatin group - Treatment with statins not supported in this
patient population - Unknown how results would compare in non-diabetic
hemodialysis patients
84
Wanner C, Krane V, Marz W, et al. Atorvastatin in
patients with type 2 diabetes mellitus undergoing
hemodialysis. N Engl J Med 2005353238248.
85
Dyslipidemia in CKD Patients
DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells
BG, Posey LM Pharmacotherapy A Pathophysiologic
Approach, 7th Edition http//www.accesspharmacy.c
om
86
Concurrent Disease States
- Use gemfibrozil with caution
- pharmacokinetics unchanged
- lowers TGs
- increases HDL
- Combination statins fibric acid derivatives
increases risk of severe myopathy - monitor for myositis
- Niacin may be useful in nondiabetic patients with
renal insufficiency
87
Concurrent Disease States
- Hypertensive patients greater-than-expected
prevalence of hypercholesterolemia - Patients with hypercholesterolemia have a higher
than expected prevalence of HTN - caused by metabolic syndrome
- HTN management
- avoid drugs that elevate cholesterol
- diuretics
- a-blockers
- niacin may magnify vasodilator hypotensive
effects
88
Monitoring
89
Pharmacoeconomic Considerations
- Statin therapy cost-effective in patients with
CHD, CHD risk equivalents, or 10 year risk 10 to
20 - Depending on lipoprotein phenotype, compliance,
efficacy other drug therapies may also be cost
effective - Specialty lipid clinics more expensive than
usual care - project ImPACT (Improve Persistence And
Compliance with Therapy) showed pharmacist run
clinics result in improved persistence/compliance - nearly 2/3 patients achieved NCEP lipid goal
- other programs show similar benefits
Bluml BM, McKenney JM, Cziraky MJ. Pharmaceutical
care services and results in project ImPACT
Hyperlipidemia. J Am Pharm Assoc 200040157165.
90
Acknowledgements
- Writer Andrea Bourgoin, Pharm.D.
- Series Editor April Casselman, Pharm.D.
- Editor-in-Chief Robert L. Talbert, Pharm.D.,
FCCP, BCPS, FAHA - Chapter Author/Section Editor
- Robert L. Talbert, Pharm.D., FCCP, BCPS, FAHA