Vaginal isolates - PowerPoint PPT Presentation
1 / 60
Title: Vaginal isolates
1
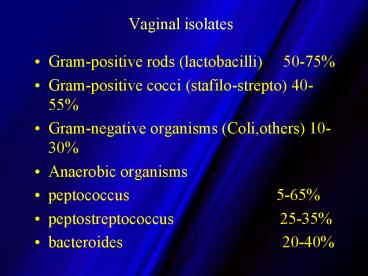
Vaginal isolates
- Gram-positive rods (lactobacilli) 50-75
- Gram-positive cocci (stafilo-strepto) 40-55
- Gram-negative organisms (Coli,others) 10-30
- Anaerobic organisms
- peptococcus
5-65 - peptostreptococcus
25-35 - bacteroides
20-40
2
Epidemiologia
Infezioni vaginali (CDC 2000)
Visits (in thousands)
anno
SOURCE National Disease and Therapeutic Index
(IMS America, Ltd.)
3
Epidemiologia
MST (CDC 2000)
Percentuale dei ceppi
anno
Mod da Sexually Transmitted Surveillance 2000 -
CDC report Dic 3, 2001
4
Eziologia delle vulvovaginiti
COMUNE vaginosi batterica candidosi
vaginale Trichomoniasi MENO COMUNE infezione
batterica secondaria in pz. con vaginite
atrofica infezione batterica secondaria a corpo
estraneo Vaginite desquamativa infiammatoria
(sensibile alla clindamicina) Vaginite
streptococcica (Gruppo A) Vaginite ulcerativa
associata a S aureus e toxic shock
syndrome Vaginite idiopatica in pazienti HIV
Cause infettive
5
Epidemiologia
Vaginiti sintomatiche (N3661)
6
STD III Other Agents Bacterial G. vaginalis
Gardnerella vaginalis is associated with
non-specific vaginitis/urethritis Found with
resident anaerobes within the vaginal tract
(Bacteroides spp.) Clue cells in vaginal smear
is diagnostic for non-specific vaginitis--bacteria
l vaginosis (BV) BV characterized
by -excessive malodorous discharge -vaginal
pH gt4.5 -clue cells -fishy, amine-like odor
7
(No Transcript)
8
STD III Other Agents Bacterial G. vaginalis
Women with BV have a resident increase in both G.
vaginalis and Bacteroides spp. G. vaginalis is
also found in 20-40 of healthy
women Pathogenesis of BV is still unclear -loss
of vaginal acidic pH -due to disruption of the
vaginal flora? -precipitated by sexual
transmission?
9
STD III Other Agents Bacterial Mycoplasma
Etiologic agents Mycoplasma hominis Ureaplasma
urealyticum Found in genital tracts of sexually
active men and women Not found as often in
populations who are not sexually
active Associated with NGU, especially U.
urealyticum -urethritis and prostatitis in
men Both organisms are susceptible to
tetracyclines
10
(No Transcript)
11
STD III Other Agents Mycotic Candida
C. albicans normal vaginal flora For unknown
reasons, growth increases dramatically
commensurate with increase in vaginal pH Range
of disease is mild (normal) to severe
(immunocom-promised) Presents as irritating
vaginitis with cheesy/thick discharge Can be
accompanied by urethritis and dysuria
(UTI) Balanitis--infection of male is rare and
usually asymptomatic
12
STD III Other Agents Mycotic Candida
Diagnosis Microscopic examination of vaginal
discharge or culture can confirm diagnosis
Treatment Oral Fluconazole or Topical
Nystatin
13
STD III Other Agents Protozoal Trichomonas
Etiologic agent Trichomonas vaginalis Found in
vaginal tract in women and urethra (and sometimes
the prostate) of men Spread during
intercourse In women, infection results in
vaginitis with a copious, foul-smelling
discharge -intense vaginal itch -foamy white/
green In men, mild urethritis rarely pathogenic
14
Trichomonas
- Parasite isolated in 30-40 of partners
- Highly contagious (two third infected after a
single contact) - More prevalent in black race
- Reportedly associated with other STD (HIV!)
15
Pelvic inflammatory disease
16
Epidemiology
- Definition- ascending infection of upper female
genital tract unrelated to pregnancy/surgery - Incidence-gt1million women In USA 1 in 9 1
- Impact on health-ectopic, infertility8
after1,20 after2, 40 aftergt3, pelvic pain,
menstrual irregularity - Financial impact-gtUS 4.2bn(USA),gt200m(UK) per
yr - Predisposing factors-Smoking, sexual behaviour,
IUD etc - Types-_at_ organs involvement,
- _at_ duration of illness
- 1.Price B, Martens M.Outpatient management of
pelvic inflammatory disease. Curr Womens health
Rep 20011(1) 36-40
17
RISK FACTORS-PID
- Frequent sexual activity
- Multiple sex partners
- Adolescence
- Presence of IUD
- Gonococcal or chlamydial infection
- Previous history PID
- Untreated male partner
- Bacterial Vaginosis
18
Unique Risks for Adolescents
- Non- barrier methods of contraception
- Multiple partners (4.6 fold increase risk PID)
- Increased ectropian and estrogenization of cervix
associated with normal adolescent female and OCP
use
19
Unique Risks for Adolescents
- PID risk 15 year old- 1in 8 compared gt24
year old- 1 in 80 - Experience more dysfunctional uterine bleeding
20
HISTORY-PID
- Pain
- low abdominal, pelvic pain
- recent gradual onset
- usually bilateral
- intensity variable
- dyspareunia
- often occurs post menses
21
HISTORY-PID
- Post-coital bleeding
- Vaginal discharge
- /- fever
22
Pelvic inflammatory disease
Hospitalizations of women 15-44 years of age
United States, 19801999
Note The relative standard error for the
estimates of the overall total number of PID
cases range from 6 to 9. SOURCE National
Hospital Discharge Survey (National Center for
Health Statistics, CDC)
23
Microbiology-endo/exogeneous
- Chlamydia
- Neisseria gonorrhoeae
- Escherichia coli
- Bacteroides
- Beta haemolytic streptococci
- Actinomyces israelli,Prevotella
sp,Peptostreptococci1 - Mycoplasma hominis, Gardnerella vaginalis-
24
Incidence of Sexually Transmitted Diseases in U.S.
25
STD III Other Agents Bacterial
1. Pathogenic Chlamydia Obligate intracellular
pathogen developmental lifecycle C.
psittaci pneumonia C. pneumoniae acute
respiratory disease atherosclerosis? C.
trachomatis trachoma STD LGV Chlamydia
trachomatis Leading cause of bacterial STD in
United States NGU--Non-gonococcal
urethritis Asymptomatic (particularly in
women) 3 catagories of serovars associated with
disease
26
STD III Other Agents Bacterial C. trachomatis
Chlamydia trachomatis serovar catagories
27
STD III Other Agents Bacterial C. trachomatis
Trachoma is the leading preventable cause of
blindness in developing countries. serovars A,
B, and C Most C. trachomatis infections are
genital and acquired during intercourse. serovars
D-K (most common in U.S.) serovars L1, L2, and
L3 (LGV) (more common in Africa, Asia, and
both Central and S. America than U.S.)
28
STD III Other Agents Bacterial C. trachomatis
Properties of the bacterium Gram negative
bacteria lacking a cell wall -do not respond to
b-lactam antibiotics -many cross-linked
molecules on surface protein-protein sulphydryl
groups Two primary phases of lifecycle EB
elementary body (infectious) RB reticulate
body (fragile)
29
STD III Other Agents Bacterial C. trachomatis
Developmental lifecycle
30
STD III Other Agents Bacterial C. trachomatis
Developmental lifecycle
EB spore-like metabolically less active RB
bacteria-like metabolically active
31
C. trachomatis Trafficking
32
STD III Other Agents Bacterial C. trachomatis
Pathogenesis and clinical features Entry C.
trachomatis enters via small abrasions in the
mucosal surfaces Attachment bind to specific
receptors taken up by parasite-induced
endocytosis Intracellular inhibit fusing of
lysosomes differentiate from EB to RB RB
replicate RB differentiate back to EB Lysis of
cell release reinfect additional
cells released into bloodstream, lymph can
spread systemically
33
STD III Other Agents Bacterial C. trachomatis
Pathogenesis and clinical features
(continued) C. trachomatis disease (serovars
D-K) is clinically similar to gonococcal
infection SYMPTOMS males usually
symptomatic in addition to urethritis can
develop an orchitis and epididymitis Reiter
s syndrome females often asymptomatic
salpingitis (ectopic pregnancy) PID newbor
ns conjunctivitis pneumonia
34
Diagnosis of Chlamydia
- Swab-endocervical, urethral
- First voided urine sample(FVU)
- Methods-culture, EIA(enzyme immunoassay), DNA
Probe,DFA ( direct fluorescent antibodies), NAA(
nucleic acid amplification), serology
35
Swabs
- Endocervical-
- Clean the mucus/discharge
- 1-2 cm deep
- rotated several turns to obtain columnar cells
- Urethral-
- (10-23 infected in the urethra only!)
- male patients-2-4 cms deep
- Vulval or vaginal-
- even self-obtained can be alternative way to
collect sample for nucleic acid amplification
assay( NAA)
36
Urine specimen
- FVU-
- an excellent sample for NAA
- no need to clean the urethra or perineum prior
to collection. - NOT mid stream urine as first bit will contain
epithelial cell which might contain Chlamydia.
37
Culture
- Only swabs, urine not suitable for culture
- use cotton, dacron, rayon on plastic/metal shaft
for collection of swab - NOT wooden spatula as it is toxic to cells.
- Use transport media-FlexTrans, M4
- Keep refrigerated, trasport at 40C
- Innoculation within 48hrs
38
Nucleic acid amplification assay (NAA)
- Polymerase chain reaction(PCR)
- Ligase chain reaction(LCR)
- Transcription-mediated amplification
- strand displacement amplification
- -excellent tool for public screening
- -specimen needed-FVUCx swab for female,
FVU for male
39
PATHOPHYSIOLOGY-Several theories
- PID starts as GC or CT cervicitis
- ascension into upper genital tract
- Polymicrobial infection occurs without GC or CT
- GC and/or CT initiate tubal inflammatory reaction
- Primes tubal mucosa for infection by endogenous
flora of lower genital tract
40
Diagnosis- Acute
- Symptoms-severe lower abd pain, worse on
movement,offensive vag discharge, generally
unwell and feverish/pyrexial - Sign-fever, tachycardia,may be hypotensive-if
septic,tender lower abd-guarding/rebound
tenderness, - Pelvic exam-tender both adnexae, cervical
excitation tenderness marked,? a palpable mass
41
Diagnosis-chronic
- Symptoms-general malaise, fatigue, backache,lower
chronic abd pain, constant with occasional
exacerbations(typically during menstruations),
intermittent offensive vaginal discharge, deep
dyspareunia - Sign-generalised lower abd tenderness esp on deep
palpation, pelvic esp cervical excitation
tenderness,bulky tender uterus, and/or tender
adnexal mass of tubo-ovarian origin - Investigation-FBC,Bacteriology-swabs-endo-cervical
, high vaginal, urethral, rectal-CS, laparoscopy
42
MINIMUM CRITERIA FOR CLINICAL DIAGNOSIS OF PID
- Lower abdominal tenderness
- Bilateral adnexal tenderness
- Cervical motion tenderness
43
DIAGNOSTIC/LAB TESTS PID
- Wet mount
- Cervical gram stain
- Endocervical tests- GC and CT
- HCG
- /-UA, CBC, sed rate(dependent on s/s)
- /- Postural BP, Psupine and seated
44
Diagnosis of PID
45
Laparoscopy-gold standard?
- Pitfalls-surgeons bias,carbonic anhydrase on
tubes, early chlamydial infection - 50 sensitive, 80 specific( Sellors etal, 1991)
- Hagers criteria for diagnosis and grading-Mild,
moderate, severe.
46
Image folder-USS as diagnostic tool!/lap view
47
Image folder specific chronic PID-Tubercular
48
Image folder Tubo-ovarian abscess
49
PID Fitz-Hugh-Curtis
50
Treatment-Principle -CDC, AGUM, RCOG-
- Prevention-health education-barrier
contraception, OCP, Identifying risk
factor-smoking, douching, IUCD-RR1.5-2.6 lt
20days, - Treatment directed against chlamydia, neisseria
and anaerobes - High suspicion
- Early treatment before bacteriological results
- Aggressive treatment in adolescents
51
OUTPATIENT REGIMEN
- Regimen A
- Ofloxacin 400mg po bid for 14 days
plus - Metronidazole 500mg po bid for 14 days
52
OUTPATIENT REGIMEN
- Regimen B
- Cefriaxone 250 mg IM once, or
- Cefoxitin 2g IM plus Probenecid 1 g orally in
single dose concurrently once or - Parenteral third-generation cephalosporin
plus - Doxycycline 100 mg po bid for 14 days
53
OUTPATIENT REGIMEN
- Regimen B
- Theoretical limitations in anaerobic coverage may
require addition of metronidazole - Alternate Oral Regimens
- Amoxacillin/clavulanic acid plus doxycycline-
limited clinical trials - Azithromycin- data insufficient to recommend for
PID
54
MINIMUM CRITERIA FOR ADMISSION
- Severe peritonitis
- Unable tolerate oral meds
- Temperature gt 38C
- Adnexal abscess or mass(gt6cm)
- Uncertain diagnosis
- Failure to respond to outpatient therapy
- Pregnancy
55
Treatment-contd
- Laparoscopy-
- grading of PID
- bacteriological culture from peritoneal fluid,
- drainage of infective pelvic collection,
- removal sequelae of PID
- Genitourinary Medicine Clinic referral- for
- test of cure,
- sexual health counselling
- contact tracing
56
Sequelae
- Chronic pelvic pain
- Tubal infertility
- Ectopic pregnancy
- Recurrences
57
PID consequences
Risk of ectopic pregnancy increased by 9 times
58
PID consequences
Tubal infertility from 9 to 25 of
patients Number and severity of episodes
59
PIDconsequences
The rate of recurrence approach 40
60
PID consequences
The risk of chronic pelvic pain is increased by
10 times
61
Salient points
- PID a threat to female reproductive health
- Secret agents-chlamydia, neisseria
- Misdiagnosis in about 35 cases
- Laparoscopy-still a gold standard in diagnosis
- Microbiological and cinical cure do NOT guarantee
restored normal reproductive function - Tubal factor infertility is dependent on the
number and severity of PID - Delay t/t for 3 days to ? likelihood of ectopic
and infertility by 3 times!! - Effective t/t contact tracing and treatment of
sexual partner/s test of cure.