Agencies and Organizations Involved with International Health - PowerPoint PPT Presentation
1 / 34
Title:
Agencies and Organizations Involved with International Health
Description:
... and specificity of palpation are low, particularly in ... Palpation ... Correspondence Between U/S and Palpation - Nepal. PVP = 28.3% PVN = 83.2 ... – PowerPoint PPT presentation
Number of Views:1231
Avg rating:3.0/5.0
Title: Agencies and Organizations Involved with International Health
1
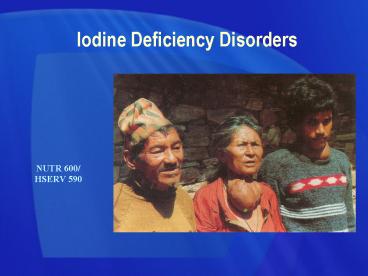
Iodine Deficiency Disorders
NUTR 600/ HSERV 590
2
Iodine Deficiency Disorders
- The single most preventable cause of mental
retardation and brain damage in the world - Control programs are in place in most countries
of the world, primarily through salt iodization - Scientific data are required to demonstrate that
adequate amounts of iodine are reaching the
target population and having an impact. - However, there has been a lack of clarity in
indicators (and criteria) for tracking progress
3
Iodine Deficiency Disorders
- World Health Assembly (1990) adopted the goal of
the elimination of IDD as a public health problem
by the year 2000 - Progress towards the elimination of IDD can only
be demonstrated if it is measured - This requires the selection of appropriate
indicators of both process and impact
4
Causes of Iodine Deficiency
Snow
Atmosphere
Rain
Iodine is not available in the soil, since it is
washed away by rain and snow, mostly in mountain
areas and plains
Lake
River
Sea
Iodine
5
Daily Iodine Requirements
Just a teaspoon in a lifetime
Daily physiological requirements for adults
100-150 ?g Assumed daily per capita salt
consumption 10 grams Fortification level of
elemental iodine 15 ppm
6
Spectrum of Iodine Deficiency Disorders
Fetus Abortion Still Birth Congenital
Anomalies Increased Perinatal and Infant
Mortality Cretinism (Neurological and
Myxedematous)
- Neonatal Neonatal Hypothyroidism
Childhood Impaired mental and physical
development
Adult Complications of Goiter Iodine-induced
hyperthyroidism (IIH)
All ages Goiter Hypothyroidism
NUTR 600/ HSERV 590
7
Population with Iodine Deficiency
At risk of mental impairment 1.6 billion
WHO (1999)
8
Population with Iodine Deficiency
Goitre 655 million
At risk of mental impairment 1.6 billion
WHO (1999)
9
Population with Iodine Deficiency
Brain damage 26 million
Goitre 655 million
At risk of mental impairment 1.6 billion
WHO (1999)
10
Population with Iodine Deficiency
Cretinism 6 million
Brain damage 26 million
Goitre 655 million
At risk of mental impairment 1.6 billion
WHO (1999)
11
Population with Iodine Deficiency
Cretinism
Brain damage
Goitre
At risk of mental impairment 1.6 billion
WHO (1999)
12
Population with Iodine Deficiency
Cretinism
Brain damage
Goitre
At risk of mental impairment 1.6 billion
WHO (1999)
13
Function of the Thyroid Hormones
Brain
Pituitary
TSH
Thyroid gland
Thyroid
hormones
Muscle
Heart
Kidneys
Liver
14
Enlargement of thyroid gland
15
Indicators of IDD in a Population
- Process of adequately iodized salt at
production level - of adequately iodized salt at household level
- of iodized salt at household level
- Impact Goiter
- Urinary iodine excretion (UIE)
- Thyroid hormones
16
Indicators of IDD - Process
- Salt iodine levels
- Two methods
- Rapid test kits (semi-quantitative)
- Titration
- Salt monitoring systems
- Ensure adequate iodine levels at all points of
distribution from Production to Household - Where problems are identified, take corrective
action
17
Indicators of IDD - Impact
- Goiter
- Total goiter prevalence
- Grade 0 No palpable or visible goiter
- Grade 1 Palpable goiter
- Grade 2 Visible goiter
- Urinary iodine excretion (UIE)
- Best marker of recent dietary intake of iodine
- Most iodine absorbed in the body eventually
appears in urine
18
Indicators of IDD - TGR
- Total Goiter prevalence
- WHO, UNICEF, ICCIDD (2001)
- Prevalence Significance of Public Health Problem
- lt 5 No IDD
- 5-19.9 Mild IDD
- 20-29.9 Moderate IDD
- ? 30 Severe IDD
19
Iodine Deficiency - Goiter
Visible goiters pretty easy to diagnose
20
Iodine Deficiency - Goiter
Palpable goiters are much more problematic
- WHO revised criteria for palpable goiter
- 1960 lobes larger than ends of thumbs
- 1994 an enlarged thyroid that is palpable, but
not visible - In Tanzania, change in clinical definition led to
a 25 increase in the prevalence of palpable
goiter - Comparability may become problematic and lead to
smaller decreases over time, or actual increase
in goiter in spite of IDD control efforts
21
Assessment of Enlarged Thyroid
- Clinical observation of the thyroid by palpation
has been the conventional method to assess goiter - Ultrasound (U/S) has become more widely used to
provide a more precise measurement of thyroid
volume. - U/S is particularly important when the prevalence
of visible goiters is low - Problem with U/S is the lack of normative
reference data (from iodine replete population)
22
Inter-observer variation in palpation
- The sensitivity and specificity of palpation are
low, particularly in grades 0 and 1 due to high
inter-observer variation. - In studies of trained endocrinologists, there is
as much as 30-40 disagreement in the
classification with ? lt 0.40
23
Correspondence Between U/S and Palpation - Nepal
- As part of National MN Survey
- Sub-sample of 403 SAC (8-10 years of age)
- U/S measured by single trained examiner (gold
standard) using a SonoAce 600 portable U/S
machine - Palpation performed by field teams
- Thyroid volume calculated based on measurements
of the width, depth and length using standard
formula - Thyroid volume compared to standard thyroid
volume-for-age values and dichotomised normal
(lt 97th centile) and enlarged (gt 97th centile)
24
Correspondence Between U/S and Palpation - Nepal
PVP 28.3 PVN 83.2 Se 69.1 Sp 46.6
Gorstein (2001)
25
Indicators of IDD - UIE
- Population IDD Status
- WHO, UNICEF, ICCIDD (2001)
- Median value Iodine Status
- lt 20 ?g/l Severe iodine deficiency
- 20-49 Moderate iodine deficiency
- 50-99 Mild iodine deficiency
- 100-199 Ideal iodine intake
- 200-299 More than adequate intake (may pose
risk of IIH) - ? 300 Excessive iodine intake
- In populations with longstanding iodine
deficiency and rapid improvement in iodine
intake, median values above 200 ?g/l are not
recommended
26
IDD IndicatorsDepends on the status of control
program
- It is now accepted that thyroid volume is less
useful in assessing current IDD status during
implementation of USI and soon after achieving
USI - Prior to any intervention, the prevalence of low
UI and goiter will be in agreement with each
other indicating IDD - Once USI is phased in (over months or years), the
prevalence of low UI will fall faster than the
prevalence of goiter
27
Appropriateness of IDD IndicatorsDepends on
control program status
28
Changes in IDD IndicatorsChina clinical trial,
Jiangsu Province
- IDD endemic area
- Households provided with iodised salt at 25 ppm
- Baseline and follow-up at 6,9,12 and 18 months
after initiation of intervention - At baseline, the severity of IDD was mild (based
on UIE) and moderate (based on TGR and U/S) - After six months, UIE had increased to adequate
levels, while thyroid size measures still
indicated moderate IDD - After 18 months, all three measures indicated
adequate iodine status
Sullivan, et. al., 2001
29
IDD IndicatorsDepends on the status of control
program
- Just as it takes years for goiter to develop in
school children, it takes years for the thyroid
to return to normal size after iodine
sufficiency is achieved - The amount of time it takes for the UI and
thyroid size to be in agreement will depend on
the severity of IDD at baseline and the length of
time it takes to phase in the USI program
30
Correspondence between Indicators
UNICEF, 1997
31
Criteria for IDD Elimination - 2000
WHO, UNICEF ICCIDD (2001)
32
Implications
- Urinary iodine is responsive to improvements in
iodine intake - However, the criteria for adequacy of USI
programs may be too rigid and does not take into
account differences in salt consumption - In many developing countries (including Nepal),
more than 10 grams of salt are consumed per day
and therefore lower levels of iodine in salt
(ppm) may be necessary
33
Control of IDD through Universal Salt Iodisation
(USI)
- Today
- Some 70 per cent of households in the developing
world are using iodized salt, compared to less
than 20 per cent at the beginning of the decade.
- As a result, 91 million newborns are protected
yearly from significant loss in learning ability
- Unfinished Business
- There are still 35 countries where less than half
the households consume iodized salt
34
Coverage of Iodized Salt by Region
Source UNICEF (2002)
35
Levels of Iodized Salt Coverage
90 or more
50 to 89
Less than 50
Source UNICEF (2002)
No recent data
36
Major Increases in Iodized Salt Coverage
Source UNICEF (2004)
37
41 Million Newborns Still Unprotected from
Learning Disabilities
Source UNICEF (2002)