Paget - PowerPoint PPT Presentation
Title:
Paget
Description:
Keep legs close together to prevent abduction. Teach crutch-walking and wheelchair transfer. Prepare stump for prosthesis. Stump must be conditioned for proper fit. – PowerPoint PPT presentation
Number of Views:51
Avg rating:3.0/5.0
Title: Paget
1
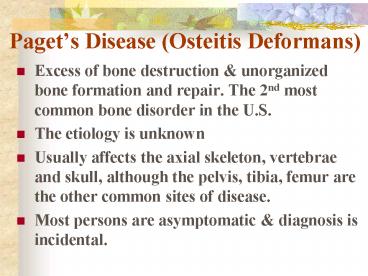
Pagets Disease (Osteitis Deformans)
- Excess of bone destruction unorganized bone
formation and repair. The 2nd most common bone
disorder in the U.S. - The etiology is unknown
- Usually affects the axial skeleton, vertebrae and
skull, although the pelvis, tibia, femur are the
other common sites of disease. - Most persons are asymptomatic diagnosis is
incidental.
2
Pagets Disease (Osteitis Deformans)
- Vascularity is increased in affected portions of
the skeleton. Lesions may occur in one or more
bones, does not spread from bone to bone. - Deformities bony enlargement often occur.
Bowing of the limbs spinal curvature in persons
with advanced disease. - Bone pain- is the most common symptom. Is is
usually worse with ambulation or activity but may
also occur at rest. Involved bones may feel
spongy warm because of increased vascularity. - Skull pain is usually accompanied with headache,
warmth, tenderness enlargement of the head.
3
Pagets Disease (Osteitis Deformans
- Pathologic fractures- because of the increased
vascularity of the involved bone-bleeding is a
potential danger. - Alkaline phosphatase levels- markedly elevated as
the result of osteoblast activity. - Serum calcium are normal except with generalized
disease or immobilization. - Gout and hyperurecemia may develop as a result of
increased bone activity, which causes an increase
in nucleic acid catabolism.
4
Pagets Disease (Osteitis Deformans
- Radiograph reveals radiolucent areas in the bone,
typical of increased bone resorption. Deformities
fractures may also be present. - Goals of the treatment- to relieve pain prevent
fracture deformities. - Pharmacologic agents are used to suppress
osteoclastic activity. Bisphosphonates
calcitonin are effective agents to decrease bone
pain bone warmth also relieve neural
decompression, joint pain lytic lesions. - Use of analgesics NSAIDs. Assistive devices,
including cane, walker.
5
Pagets Disease (Osteitis Deformans
- Deformities may be corrected by surgical
intervention (osteotomy). ORIF may be necessary
for fractures. - The patient may benefit from a PT referral. Local
application of ice or heat may help alleviate
pain. - A regular exercise should be maintained walking
is best. Avoid extended periods of immobility to
avoid hypercalcemia. - A nutritionally adequate diet is recommended.
Assistance in learning to use canes or other
ambulatory aids. - The Arthritis Foundation Paget Foundation are
useful resources for patients their families.
6
Osteomyelitis
- Infection of the bone, most often of the cortex
or medullary portion. Is is commonly caused by
bacteria, fungi, parasites viruses. - Classified by mode of entry- Contiguous or
exogenous is caused by a pathogen from outside
the body or the by the spread of infection from
adjacent soft tissues. The organism is Staph
aureus. Example- pathogens from open fracture.
The onset is insidious initially cellulites
progressing ti underlying bone.
7
Osteomyelitis
- Hematogenous- caused by bloodborne pathogens
originating from infectious sites within the
body.Ex sinus, ear, dental, respiratory GU
infections. The infection spreads from the bone
to the soft tissues can eventually break
through the skin, becoming a draining fistula.
Again, Staph aureus is the most common causative
organism. - Acute Osteomyelitis left untreated or unresolved
after 10 days is considered chronic. Necrotic
bone is the distinguishing feature of chronic
osteomyelitis.
8
Osteomyelitis
- The pathophysiology is similar to that infectious
processes in any other body tissue. - Bone inflammation is marked by edema, increased
vascularity leukocyte activity. - The patient report fever, malaise, anorexia,
headache. The affected body may be erythematous,
tender, edematous. There may be fistula
draining purulent material. - Blood test- increase WBCs, ESR, C-protein
levels.
9
Osteomyelitis
- Treatment is difficult costly. The goal are
complete removal of dead bone affected soft
tissue, control of infection elimination of
dead space (after removal of necrotic bone). - The nursing management-use of aseptic technique
during dressing changes. Observed for S/S of
systemic infection, administered antibiotic on
time. - ROM exercises are encouraged to prevent
contractures flexion deformities
participation in ADL to the fullest extent is
encouraged.
10
Tumor of the MSS
- MSS constitute 3 of all malignant tumors.
- Malignant tends to cause more bone destruction,
invasion of the surrounding tissues metastasis. - Benign tumors- tend to be less destructive to
normal bone. - The cause of bone tumors is unknown.
- The tumor is defined as a new growth or
hyperplasia of cells. This growth is in response
to inflammation or trauma.
11
Tumor of the MSS
- Osteosarcoma- A malignant tumor originating from
osteoblast (bone-forming cells). Occurs twice as
frequently in males as in females. - Usually located at the end of the long bones
(metaphysis). Most frequently seen at the distal
end of the femur or the proximal end of the
tibia. - Lungs, a common site of metastasis.
- Pain and swelling at the site limitation of
movement. - Bone biopsy is used to confirm the diagnosis.
- X-ray films, CT scans, MRI bone scans show
tumor location size. - Historically, the treatment of choice is
amputation.
12
Tumor of the MSS
- Ewings sarcoma- A malignant tumor of the bone
originating from myeloblasts with early
metastases to lung, lymph nodes, other bones. - Usually located on the shaft of the long bones.
Femur, tibia, humerus are common sites. - Poor prognosis. Common in persongt 40 years old.
Affect males more than females. - Pain increased with weight bearing. May complain
of weight loss, malaise, or anorexia. - Causes pathologic fractures.
- Treatment Palliative, radiation, chemotherapy.
13
Tumor of the MSS
- Chondrosarcoma- Usually affects persons 50-70
years old. Accounts for 20 of all bone tumors - Affect males than females.
- Slow growing, insidious onset. Most common in
humerus, femur, pelvis. - Localized pain, swelling. May have palpable mass.
Severe, persistent pain. May infiltrate joint
space soft tissue metastasize to the lungs. - Treatment Surgical incision, amputation.
14
Tumor of the MSS
- Fibrosarcoma- Usually affects persons 30- 50
years old. Affects females than males. - Occurs in bony fibrous tissue of femur tibia.
- Accounts for 4 of primary malignant bone tumors.
- May result from radiation therapy, pagets
disease or chronic osteomyelitis. - Night pain, swelling, possible palpable mass. May
cause pathologic fractures. - May metastasize to the lungs.
15
Fractures
- A break in the continuity of bone caused by
trauma, twisting or as a result of bone
decalcification. Results when the bone is unable
to absorb the stress. Result of an accident or
injury, stress fracture occur as a result of
normal activity or after minimal injury. - Causes of Fracture Fatigue- muscles are less
supportive to bone, therefore, cant absorb the
force being exerted. Bone neoplasms- cellular
proliferations of malignant cells replace normal
tissue causing weakened bone. Metabolic
disorders-poor mineral absorption hormonal
changes decreases bone calcification which
results in a weakened bone. Bedrest or disuse-
atropic muscles osteoporosis causes decreased
stress resistance.
16
Fractures (types)
- Greenstick- A crack bending of a bone with
incomplete fracture. Only affects one side of the
periosteum. Common in skull fractures or in young
children when bones are pliable. - Comminuted Bone completely broken in a
transverse, spiral or oblique direction (
indicates the direction of the fracture in
relation to the long axis of the fracture bone).
Bone broken into several fragments. - Open or compound Bone is exposed to the air
through break in the skin. Can be associated with
soft tissue injury. Infection is common
complication due to exposure to bacterial
invasion.
17
Fractures (types)
- Closed or simple Skin remains intact. Chances
are greatly decreased for infection. - Compression Frequently seen with vertebral
fractures. Bone has been compressed by other
bones. - Complete Bone is broken with disruption of both
sides of the periosteum. - Impacted one part of fractured bone is driven
into another. - Depressed Usually seen in skull or facial
fractures. Bone or fragments of bone are driven
inward. - Pathological break caused by disease process.
- IntracapsularBone broken inside the joint.
- Extracapsular Fracture outside the joint.
18
Fractures (stages of bone healing)
- Occurs over several weeks
- New bone tissue occurs in region of break
- Repair is initiated by migration of blood vessels
and connective tissue from periosteum in break
area. - Dense fibrous tissue fills from periosteum in
break area. Osteoblast near the broken area.
Chondroblast further away from broken area. - Cells deposit cartilage between broken surfaces
- Cartilage is slowly replaced by mineralized bone
tissue, which completes repair.
19
Fractures (signs symptoms)
- Pain or tenderness over involved area.
- Loss of function of the extremity
- Crepitation sound of grating bone fragments
- Ecchymosis or erythema
- Edema
- Muscle spasm
- Deformity Overriding Angulation- limb is in
unnatural position.
20
Fractures (Emergency care)
- Immobilize affected extremity to prevent further
damage to soft tissue or nerve. - If compound fracture is evident, dont attempt to
reduce it. Apply splint. Cover open wound with
sterile dressing. - Use splint External support is applied around a
fracture area to immobilize the broken ends.
Material used wood, plastic (air splints),
magazines. - Function of the splinting Prevent additional
trauma, reduce pain, decrease muscle spasm, limit
movement, prevent complications, such as fat
emboli if long bone fracture. - Provide specific care for fracture treatment
traction, cast. Surgical intervention.
21
Traction
- Force applied in two directions to reduce and/ or
immobilize a fracture, to provide proper bone
alignment and regain normal length, or to reduce
muscle spasm. - Closed reduction Manual manipulation. Usually
done under anesthesia to reduce pain relax
muscles, thereby preventing complications. Cast
is usually applied following closed reduction. - Open reduction Surgical intervention. Usually
treated with internal fixation devices (screws,
plates, wires). Cast application.
22
Traction
- Skeletal Traction Mechanical applied to bone,
using pins (Steinmann), wires (Kirscher), or
tongs (Crutchfield). Most often used in fractures
of femur, tibia, humerus. - Skin traction applied by use of elastic
bandages, moleskin strips, or adhesive. Used most
often in alignment or lengthening (for congenital
hip displacement) or to relieve muscle spasms in
preop hip clients. Most common types are
Russell, Bucks, Cervical (used for whiplashes
cervical spasm), -pull is exerted on one plane
used for temporary immobilization Pelvic
traction (used for low back pain).
23
Traction(Principles)
- The line of pull must be maintained. Center the
patient in the bed place in good alignment. - The pull of traction must be continuous. Remove
or add weights only with MD order. - The ropes weights must be free of friction. Be
certain the weights hangs free at all times
that the ropes are over the center of the pulley. - There must be sufficient countertraction
maintained at all times. Keep the patient from
sliding to the foot of the bed.
24
Cast Care
- After application of cast, allow 24 to 48 hours
for drying. For synthetic cast, allow 30 minutes - Cast will change from dull to shiny substance
when dry. - Dont handle cast during dying process, because
indentation from fingermarks can cause skin
breakdown under cast. - Keep extremity elevated to prevent edema.
- Provide for smooth edges surrounding cast. Smooth
edges prevent crumbling and breaking down of
edges. Stockinet can be pulled over edge
fastened down with adhesive tape to outside of
cast. - Observe casted extremity for signs of circulatory
impairment. Cast may have to be cut if edematous
condition continues. - Always observe for sign symptoms of
complications pain swelling, discolaration,
tingling or numbness, diminished or absent pulse,
paralysis, cool to touch.
25
Cast Care
- If there is an open, draining area on the
affected extremity, a window (cut out portion of
cast) can be utilized for observation and/or
irrigation of wound. - Keep cast dry. Breaks down when water comes in
contact with plaster. Use plastic bags or Chux
during bath or when using bedpan, to protect cast
material. - Utilize isometric exercises to prevent muscle
atrophy to strengthen the muscle. Isometrics
prevent joint from being immobilized. - Position client with pillows to prevent strain on
unaffected areas. - Turn every 2 hours to prevent complications.
Encourage to lie on abdomen 4 hours a day.
26
Cast (complications)
- Respiratory complications have client cough DB
q 2 hours. Turn q 2 hours if not contraindicated. - Thrombus embolic formation. Apply SCD. Start
anticoagulation therapy if needed. Observe for
S/S of pulmonary and/or fat emboli. - Contractures Start ROM exercises to affected
joints. Provide foot board. - Skin breakdown- massage with lotion once a day to
prevent drying. Alternate pressure mattress,
sheepskin. Use stryker boots or heel protectors. - Prevent urinary retention and calculi. Encourage
fluids. Monitor intake output.
27
Cast (complication)
- Prevent constipation Encourage fluids, Provide
high-fiber diet. Administer laxative or enema as
ordered. - Provide psychological support Allow to ventilate
feelings of dependence. Encourage independence
when possible. Encourage visitors for short time
periods. Provide diversionary activities.
28
Fractures (Complications)
- Compartment Syndrome An increase in the pressure
within the a fascial muscle compartment - Tissue damage can occur within 30 minutes
elevated pressure for more than 4 hours can
result in irreversible damage limb loss. - Signs symptoms 6 Ps. Pain-severe,
unrelenting, unrelieved by analgesia increased
by elevation of the extremity. Pallor- coolness,
slow capillary refill. Pulselessness-diminished
or absent pulses. Increase pressure and
paresthesia paralysis. - Goals of treatment decreasing tissue pressure,
restoring blood flow preserving function of the
limb. - Diagnosis Intracompartment pressure gt 30 mm hg.
29
Fractures (Complications)
- Treatment Fasciotomy-open the affected
compartment, decrease the pressure restore
normal perfusion. The wound is covered with wet
saline dressing. - Fat embolism syndrome (FES)-fat globules tissue
thromboplastin are released from the bone marrow.
The fat molecules enter the venous circulation,
travel to the lungs embolize the small
capillaries arterioles. - S/S hypoxemia, tachypnea, fever, chest pain
altered mental status.The presence of unexplained
fever, accompanied by a change in mental status
petechiae, shld. Alert the caregiver to the
possibility of FES. The MD shld. Be notified
immediately.
30
Fractures (Complications)
- Infection leading cause of delayed union
nonunion, occurs primarily in open or compound
fractures. The most symptoms occur within 4 weeks
of the injury. - S/S Pain, erythema edema.
31
HIP fractures
- High incidence in elderly group-most common cause
of traumatic death after age 75. - Fractures caused by brittle bones (osteoporosis)
7 frequent falls in the elderly. - Elderly with hip fractures frequently have
associated medical conditions (CAD, renal
disorders). - Assessment Intracapsular-bone broken inside the
joint-treated by internal fixation-replacement of
femoral head with Austin Moore prosthesis. - Placed in skin traction first for immobilization
relief of muscle spasm.
32
HIP fractures
- Extracapsular trochanteric fracture outside the
joint. - Can be treated by balanced suspension traction.
Full weight-bearing usually in 6 to 8 weeks, when
healing takes place. - Surgery usually internal fixation with wire.
- Intertrochanteric fracture extends from medial
region of the junction of the neck lesser
trochanter toward the summit of the greater
trochanter. Treated initially with balanced
suspension traction. Internal fixation used with
nailplate, screws wire. Not allowed to flex hip
to the side, on the side of the bed, or in a low
chair. When hip is flexed, displacement can occur.
33
Total hip replacement
- Replacement of both the acetabulum the head of
the femur with metal or plastic implants. - Used in degenerative diseases or when fracture of
the head of femur has occurred with nonunion. - To prevent flexion, keep operative leg in
abduction by use of pillow or abductor splints. - Keep hemovac in place until drainage has subsided
(24 to 96 hours). - Prevent edema readjust SCD at least every 4 to 8
hours. - Prevent infections- monitor prophylactic
antibiotic.
34
HIP fractures
- Continuous passive motion (CPM) first day postop
with increasing degree of flexion to 90 degrees. - Ambulate client carefully at bedside-first or
second day. Dont allow to bear weight on
affected hip. Up with walker 2nd post.op day. - Prevent thrombus formation from venous
stasis-promote leg exercises-flexing feet
ankles. - Start physical therapy asap.
- Instruct not to use low chairs or sit on edge of
bed. Use commode extenders, high stools, no
bending over activities.
35
HIP fractures
- Observe for neurovascular problems in affected
leg Color and temperature, edema in leg, pain on
passive flexion of foot, numbness-ability to move
leg, pedal pulses capillary refill.
36
Total Knee Replacement
- Implantation of a metallic upper portion that
substitutes for the femoral condyles a high
polymer plastic lower portion that substitutes
for the tibial joint surfaces. - Continuous passive motion(CPM) may be ordered
postop.-moderate flexion extension-increase
circulation movement. - Perform quad-setting straight-leg raising
exercises every hour. - Perform ROM.
- Do not dangle to prevent disclocation.
37
Total Knee Replacement
- Hemovac is inserted to drain excessive blood and
drainage. Maintain accurate I/O. Observe for
hemorrhage infection. - Instruct client for crutch walking.
- Complications wound infection, DVT, Pulmonary
and fat embolism, dislocation of the prosthesis.
38
Amputations
- The surgical removal of a limb, a part of a limb,
or a portion of a bone elsewhere than at the
joint site. - Removal of a bone at the joint site is termed
disarticulation. - More than 110,000 are performed each year in the
U.S. 91 of them are lower extremity
amputations. - Occurs in patients with diabetes 15 times more
frequently than in other patients with chronic
arterial occlusive disease.
39
Amputations (types)
- Below the Knee (BKA)
- Above the knee (AKA)
- Amputations of the foot and ankles (symes)
- Amputation of the foot metatarsus and tarsus
(heys or lisfrancs) - Hip disarticulation-removal of the limb from the
hip joint. - Hemicorporectomy- removal of half of the body
from the pelvis and lumbar areas.
40
Amputations (Assessment)
- Evaluate dressing for signs of infection or
hemorrhage. - Observe for signs of a developing necrosis or
neuroma in incision. - Evaluate for phantom limb pain.
- Observe for signs of contractures.
- Provide preop. nursing care management. Have
client practice lifting buttocks off bed while in
sitting position. Provide ROM to unaffected leg.
Inform about phantom limb sensation- pain
feeling that amputated leg still there caused by
nerves in the stump.
41
Amputations
- Provide post. Op. care. Observe stump dressing
for signs of hemorrhage infection. - Observe for symptoms of a developing necrosis or
neuroma in area of incision. - Provide stump care rewrap ace bandage 3 to 4
times daily. Wash stump with mild soap water.
If skin is dry, apply lanolin or vaseline to
stump. - Teaching related stump care. BKA-dont hang stump
over edge of bed. Dont sit for a long periods of
time. - Above the knee-prevent external or internal
rotation of limb. Place rolled towel along
outside of thigh to prevent rotation.
42
Amputations
- Position in prone position to stretch flexor
muscle to prevent flexion contractures of hip.
Done usually after first 24 to 48 hours postop.
Place pillow under abdomen 7 stump. Keep legs
close together to prevent abduction. - Teach crutch-walking and wheelchair transfer.
- Prepare stump for prosthesis. Stump must be
conditioned for proper fit. Shrinking shaping
stump to conical form by applying bandages or an
elastic stump shrinker. A cast readies stump for
the prosthesis. - Provide care for temporary prosthesis which
applied until stump has shrunk to permanent
state. - Recognize respond to clients psychological
reactions to amputation. Feelings of loss,
grieving, loss of independence, lowered
self-image, depression. - Continue discussing phantom limb pain with client.




![[PDF] PAGET'S DISEASE OF THE NIPPLE: A Guide for Women Living with Paget's Disease and Their Caregivers: The Path to The breast Health Paperback – February 2, 2024 Android PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10084273.th0.jpg?_=20240724123)

























