DRUG DISPOSITION - PowerPoint PPT Presentation
1 / 47
Title:
DRUG DISPOSITION
Description:
4. Describe how drugs are removed from the body. ... definition of prodrug an inactive form of a drug that is converted to active form in the body. ... – PowerPoint PPT presentation
Number of Views:2090
Avg rating:3.0/5.0
Title: DRUG DISPOSITION
1
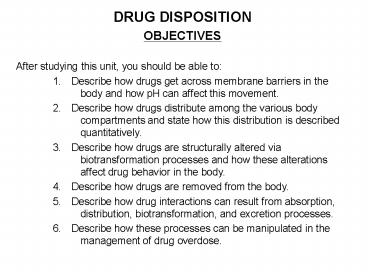
- DRUG DISPOSITION
- OBJECTIVES
- After studying this unit, you should be able to
- 1. Describe how drugs get across membrane
barriers in the body and how pH can affect
this movement. - 2. Describe how drugs distribute among the
various body compartments and state how this
distribution is described quantitatively. - 3. Describe how drugs are structurally altered
via biotransformation processes and how these
alterations affect drug behavior in the body. - 4. Describe how drugs are removed from the body.
- 5. Describe how drug interactions can result from
absorption, distribution, biotransformation,
and excretion processes. - 6. Describe how these processes can be
manipulated in the management of drug
overdose.
2
PROTOTYPE DRUGS
- We will not discuss specific drugs in this
section but rather some general types - 1. Organic acid drugs, e.g. those containing an
ionizable carboxyl group (R-COOH). - 2. Organic base drugs, e.g. those containing an
ionizable amino group (R-NH2, R2NH, R3N). - 3. Organic neutral non-ionizable drugs.
- 4. Large molecule drugs, e.g. polypeptides and
proteins.
3
I. INTRODUCTION
- Our objectives in drug therapeutics are to
administer a drug, to get it to its site of
action in sufficient quantity to exert its effect
for some useful period of time, and then
ultimately terminate its action and remove it
from the body. - What happens to the drug in this process is
termed drug disposition which includes drug
absorption, distribution, biotransformation, and
excretion. In this section we will consider
these processes qualitatively. - Subsequently, Dr. Walle will discuss the
quantitative description of drug disposition,i.e.
pharmacokinetics. - The processes involved in drug disposition are
depicted schematically in the diagram below which
will be referred to throughout this section.
4
(No Transcript)
5
II. DRUG ABSORPTION
- Drug absorption is the process of getting the
drug into the body most often this is synonymous
with getting the drug into the blood. - A. Movement of Drugs Across Biological Membranes
- Movements Into (Absorption), as well as Within
(Distribution, Biotransformation) and Out
(Excretion) of the body involve drug moving from
one compartment to another by crossing membrane
barriers (a cell membrane or a layer of cells). - Physical properties determine the movement of
drugs across membranes. - Transfer of drugs across membranes occurs by
- 1. Passive transfer processes
- a. Passive diffusion
- 1) Lipid solubility required to dissolve in
membrane - (a function of polar and non-polar groups)
- a) Polar groups (e.g. COOH, NH, OH, charged
groups) increase water solubility - b) Nonpolar groups (e.g. CH2, CH3, aromatic
rings) - increase lipid solubility - 2) Ionization (organic acids and bases)
increase polarity - 3) Requires concentration gradient for net
transport - b. Filtration
- 1) Molecular size
6
II. DRUG ABSORPTION
- 2. Carrier mediated transfer processes
- a. Active transport
- 1) Discrete transporter proteins finite
number, therefore saturable - 2) Structurally selective competitive
inhibition - 3) Energy requiring can transport against
concentration gradient - 4) Examples
- (a) amino acid transport amino acid analog
drugs - (b) P-glycoprotein multidrug resistance
- (c) acid and base transport in renal tubule
- b.Receptor mediated endocytosis
- 1) Involves membrane receptors
- 2) Transport of large polypeptides and
proteins - 3) Likely to become increasingly important
with the use of bioengineered proteins as
drugs
7
Transfer of small molecules across membrane
barriers
8
Transfer of large molecules by receptor
mediated endocytosis
9
Passive DiffusionPrinciple of Non-ionic
Diffusion
- Only the nonionized form of a drug diffuses
across the lipid membrane - The more lipophilic the drug is, the faster is
the diffusion - 3. At equilibrium the concentration of the
nonionized form is the same on both sides of the
membrane
10
pH Partition Effects
If the drug is an ionizable acid or base, the
concentration of total drugon each side of the
membrane can be vastly different if there is a pH
gradient across the membrane
1. Acid drugs tend to concentrate on the high pH
side of the membrane.
2. Basic drugs tend to concentrate on the low pH
side of the membrane.
11
pH Partition Effects
- The ionization tendency of a drug is indicated by
its pKa. - The pKa is the pH at which the drug is half
ionized. (Note that the pKa does not tell you if
a drug is an acid or a base it only tells you
how strongly it tends to ionize.) - pH pKa equal concentration of ionized and
nonionized (ratio 11) - acid drugs are increasingly ionized as pH goes
up (more basic) - basic drugs are increasingly ionized as pH goes
down (more acidic) - for each pH unit away from the pKa, the ratio
increases tenfold - pH has no effect on neutral, nonionizable
drugs)
12
B. Absorption of Drugs from the Gastrointestinal
Tract via Oral Dosing
- The drug must first dissolve in the gastric and
intestinal fluids. - a) The pharmaceutical preparation can affect
dissolution - b) Different salt forms of a drug have
different solubilities - c) Other materials present can render
dissolved drug nonabsorbable
13
- Properties of the drug affect its absorption.
- a) Lipophilicity
- b) Ionization
- some examples Ratio - Nonionized Ionized
- Stomach Intestine Plasma
- pH 1.4 pH 5.4 pH
7.4 _______ _______ _______ - Acidic drug (Probenecid) pKa 3.4 100 1 1
100 110,000 - Basic drug (Amitriptyline) pKa 9.4 1 10
8 1 10 4 1100
14
- Properties of the drug affect its absorption
(cont.) - For drugs with very low Nonionized Ionized
ratios (
lipophilic absorption will be poor. - There is very poor absorption of completely
charged drugs, e.g. quaternary ammonium
compounds. - 3. Properties of the absorbing surface which
affect absorption - a) area of surface
- b) blood circulation to absorbing surface
- 4. Other factors which affect absorption
- a) concentration of dissolved drug
- b) contact time with the absorbing surface
15
- C. Absorption of Drugs Administered via Other
Routes - 1. Alimentary tract
- a. Oral mucosa - rapid absorption, small
surface area (used for potent drugs to - relieve anginal pain) avoids immediate exposure
to liver - b. Rectal mucosa - suppository dosage alternate
route for nauseated patient - only ca. 50 passes immediately through the
liver - 2. Parenteral routes - bypassing G.I. tract and
immediate exposure to the liver - a. Routes which still entail an absorption
process - (absorption rate can vary depending upon the
vehicle) - 1) subcutaneous
- 2) intramuscular
- b. Routes which bypass the absorption
process - 1) intravenous
- 2) intraarterial
- 3) intrathecal (into the spinal subarachnoid
space) - 3. Pulmonary endothelium (volatile anesthetics,
aerosols)
16
- DRUG DISTRIBUTION
- (see the general diagram on page 2)
- Tissue distribution of drugs is usually not
uniform throughout the body - drug concentration at the site of action
determines the pharmacologic effect. - A. Differential Distribution of Drugs into
Different Body Compartments - An example - Concentrations of the
antihypertensive drug propranolol in tissues 3 hr
- after an i.v. dose (Walle, et al.)
- Blood 0.13 µg/g
- Aorta 0.18 µg/g
- Muscle 0.38 µg/g
- Heart 0.60 µg/g
- Lung 8.29 µg/g
- Liver 0.49 µg/g
- Brain 1.64 µg/g
How can we examine drug distribution in man when
only blood concentrations can readily be measured?
17
Apparent Volume of Distribution (Vd) - the
volume the drug appears to be distributed in, at
the same concentration as in blood Vd
Amount of Drug in the Body___
Concentration of Drug in the BloodAn
analogy
Example - Give 70 mg of drug to a 70 kg (70
liters volume) patient. If the drug is evenly
distributed in blood and all tissues, then the
blood concentration 70 mg./70 liters 1
mg/l. Vd 70 mg / 1 mg/l. 70 liters the
actual volume
18
- Example (continued) If the drug is highly bound
in certain tissues (analogy - stuck to bottom of
container), less is in the blood leading to a
lower blood concentration and a higher Vd. - Vd 70 mg / 0.1 mg/l. 700 liters a
larger apparent volume - If (in this example) the blood concentration
(Cb) is - into tissues and preferentially bound there.
- If (in this example) Cb 1 mg/l, the drug is
distributed into a smaller volume than the - total body volume (e.g. a drug might distribute
only into body water). - For perspective - some typical volumes for a
normal 70 kg person - Body volume 70 liters
- Body water 41 liters
- Extracellular water 12 liters
- Whole blood 6 liters
- Plasma 3 liters
19
- Distribution of Drugs within the Blood
- (refer to general diagram on page 2)
- 1. Drug is present both free in solution and
bound to plasma proteins - protein binding is a reversible process. An
equilibrium is established which - depends upon the affinity of the drug for the
binding sites. - a. Only free drug can cross membranes to
enter other tissues - b. Only free drug can bind to receptors.
- Thus, a change in free drug blood concentration
can lead to a - transient change in pharmacological response
and in the Vd. - Note - most blood level determinations for drugs
measure both bound - and unbound.
- 2. The free drug concentration is determined by
binding to plasma proteins. - Acidic drugs bind mainly to albumin.
- Basic drugs bind mainly to ?1-acidglycoprotein.
Lipophilicity also important.
20
- Distribution of Drugs within the Blood (cont.)
- 4. Historically, textbooks have emphasized
plasma protein binding displacement - interactions as clinically significant. Most
such clinical effects are now - recognized as due primarily to other
interactions, e.g., inhibition of metabolism. - 5. Binding interactions likely to be clinically
significant only in few cases, particularly
where - a. Drug is very highly bound 90
- b. Drug has very low therapeutic index (toxic
conc./therap. conc.) - c. Drug has a low hepatic extraction
- d. Drug is given intravenously.
- C. Distribution of Drugs in Other Tissues
- 1. Binding can be functional (i.e. to receptors)
or nonfunctional - sequestration to tissue proteins.
- 2. Binding to tissue proteins is reversible, but
may be rate limiting in - elimination. Highly lipophilic drugs tend to be
highly bound.
21
- C. Distribution of Drugs in Other Tissues
(cont.) - Fat as a storage depot - highly lipid soluble
drugs accumulate in adipose tissue (important for
toxic chemicals, e.g. polychlorinated organics). - Time course of tissue distribution (drug
redistribution) - Distribution - equilibrium occurs in stages due to differences
in perfusion of different tissues - a. Highly vascularized tissues (e.g. brain,
visceral organs) equilibrate - first (e.g. for the short acting anesthetic,
thiopental, peak - concentration in brain is reached 30 sec after
intravenous dose.) - b. Less vascularized tissues (e.g. muscle, skin)
equilibrate more slowly - (for thiopental, 15 - 30 min).
- c. Poorly vascularized tissues (adipose, bone)
equilibrate last (may require several hours). - d. Some drug effects may be terminated by
redistribution rather than - actual elimination (biotransformation or
excretion) of the drug.
22
- D. Distribution Across Some Particular Barriers
- 1. Blood Brain Barrier
- a. There are tight junctions between
endothelial cells of brain capillaries and few
transendothelial channels - thus, passage of
drugs from the blood into the central nervous
system is severely restricted. - b. Drugs cross the blood brain barrier by
- Passive diffusion - highly lipid soluble drugs
cross rapidly (peak concentration reached in
minutes). Very polar, highly water soluble drugs
do not cross at all. - Active transport - e.g. transport of amino acid
type of drugs - (methyldopa, L-dopa)
- iii) Endocytosis - engineered chimeric proteins
can exploit natural receptors to transport
proteins into CNS (experimental Alzheimers
disease therapy uses transferrin receptor
antibody conjugated to nerve growth factor).
23
1. Blood Brain Barrier (cont.)
- Strategies for delivery of highly water soluble
drugs - i) Invasive - intrathecal or intraventricular
injection. - ii) Transient disruption of the barrier with
mannitol. - iii) Prodrugs - metabolized to active form
within the CNS. - (definition of prodrug an inactive form of a
drug that is converted to active form in the
body. - Prodrugs are used to achieve more desirable
absorption/distribution when the actual
active form is deficient in desired
properties.
24
- 2. Placental "Barrier"
- a. Exhibits all modes of transfer of molecules
across membranes. Passive diffusion due to
lipid solubility is probably most important.
Thus, there is no protective barrier. - b. Drug exposure is especially risky to the
fetus due to susceptibility to teratogenic
effects in early development. Metabolites can
accumulate in the fetus due to lower lipid
solubility of the metabolites compared to parent
drug.
25
IV. BIOTRANSFORMATION (DRUG METABOLISM)
Biotransformation leads to structural alteration
of the drug molecule by the action of a variety
of enzymes. This alteration generally
facilitates excretion of lipid soluble drugs by
making them more water soluble
- A. Drugs often undergo two step ( biphasic)
metabolism, e.g. - 1. Phase I biotransformation reactions
chemically modify the drug - via oxidation, reduction, hydrolysis, etc.
which, in addition to changing the physical
properties of the molecule (e.g. water
solubility), results in - a. Inactivation (detoxification) of the
drug. A portion of the chemical structure,
essential to the pharmacological effect, has been
altered. - b. Conversion of active drug to active drug
metabolite. A portion of the - chemical structure, not essential to the
pharmacological effect, has - been altered.
26
1. Phase I biotransformation (cont.)
- c. Conversion of inactive drug compound (e.g.
prodrug) to active drug. - e.g. Enalapril (an inactive ester with good
absorption properties) is hydrolyzed - to a biologically active carboxylic acid
metabolite. - Generation of a chemically reactive metabolite
(reactive intermediate). - e.g. The anesthetic halothane is oxidized to
trifluoroacetyl chloride which - can subsequently react chemically to form a
covalent bond to proteins.
- Phase I reactions yield metabolic products which
are generally more polar than the parent ug and
are therefore more easily excreted.
27
2. Phase II biotransformation reactions add a
conjugating group to the drug molecule which
(almost always) results in a.
Pharmacologically inactive metabolites. b.
Highly ionized, polar, water soluble metabolites.
Examples acetaminophen (a weak acid with pKa
10) yields more acidic sulfate and glucuronide
conjugates
28
c. Exception Acetylation (e.g. of
sulfonamides) yields less soluble metabolites
2. Phase II biotransformation (cont.)
29
3. Many drugs undergo both Phase I and Phase II
metabolism, e.g. propranol
D distribution coefficient between organic and
aqueous phases, a measure of lipophilicity.
30
Metabolic sites a. Liver (most important site
of drug metabolism) - factors affecting
hepatic clearance of drugs include i. acti
vity of the drug metabolizing enzymes ii. h
epatic blood flowIn some cases, hepatic
clearance can be sufficiently high to remove most
of the drug from the blood passing through the
liver. This effect is called presystemic or
first-pass hepatic elimination.
B. Drug Metabolizing Enzymes
31
Definition Extraction Ratio
b. Drug metabolism also occurs in many other
tissues (e.g. intestine, lung, kidney)
32
- 2. Liver microsomal metabolism (Microsomes are
isolated smooth endoplasmic reticulum) - The smooth endoplasmic reticulum contains two
particularly important drug metabolizing enzyme
systems the Cytochrome P450 (CYP) complex and
the UDP-glucuronyl transferase system. - a. Cytochrome P-450 (CYP) complex
- i. iron-heme monoxygenase enzyme with
associated NADPH - CYP - oxidoreductase require molecular oxygen
and NADPH - ii. large number of CYP isoenzymes gene
superfamily - iii. wide range of substrates - isoenzymes
oxidize particular structural types - iv. CYPs also involved in endogenous
metabolism e.g. steroids - Net reaction
- Drug - H O2 2NADPH ? Drug - OH
H2O 2NADP - b. UDP-glucuronyl transferase - forms
glucuronic acid conjugates (See p. 13)
33
3. Nonmicrosomal enzymes - in liver, other
tissues and in plasma a. Phenolsulfotransferase
s - form sulfate conjugates (See p.13) b.
Alcohol dehydrogenase c. Mitochondrial
monoamine oxidase (MAO) d. Esterases e.
Amidases
34
1. Biotransformation is responsible for
termination of pharmacological effects of
lipophilic drugs.2. Large variability in
biotransformation yields large variability in
drug response.
C. Significance of Biotransformation
D. Variability in Biotransformation
1. Variability Among Individuals a. Genetic
differences i. Cytochrome P-450 (CYP)
isoenzymes Drug oxidations - Bimodal
distribution
35
D. Variability in Biotransformation (cont.)
1. Variability Among Individuals a. Genetic
differences
- There are multiple cases of known genetic
polymorphism with respect to CYP genes for drug
metabolizing enzymes. The classical test for
CYP2D6 phenotype is the debrisoquin polymorphism
test wherein the ratio of parent drug to
metabolite is determined in patients following a
test dose of debrisoquin. Gene chip tests are
now available to determine genotype of multiple
CYP genes. - Different population groups exhibit different
genetic distributions. - ii. Some other drug metabolizing enzymes are
known to exhibit genetic polymorphism - a) N-acetyl transferase Bimodal or trimodal
distribution - b) Pseudocholinesterase (hydrolysis of muscle
relaxant succinylcholine) - Trimodal
distribution
b. Age differences i. Biotransformation
enzyme activities low in neonates. Newborns are
often deficient in glucuronidation
ability. ii. Elderly are heterogeneous
due to different rates of deterioration of enzyme
and elimination systems. No blanket statement
can be made regarding dosage adjustment
36
D. Variability in Biotransformation (cont.)
1. Variability Among Individuals (cont.)
- c. Sex differences. Females metabolize many
drugs slower than males. Metabolism rate of
some drugs is correlated with testosterone
levels. - d. Pathology. e.g. liver disease
- e. Species differences - important in new drug
development.
2. Variability Within A Given Individual
a. Enzyme induction i. Stimulation of
metabolism by other substances (very common).
Smoking, alcohol, pesticides, other drugs, diet
(brussel sprouts, charcoal-broiled meat, high
protein) ii. Stimulation of drug's own
metabolism (autoinduction) - Blood levels fall
during chronic therapy (tolerance). Induction
is a slow process. b. Enzyme
inhibition One drug inhibits the metabolism of
another via competition at the same site of an
enzyme.
37
2. Variability Within A Given Individual (cont.)
b. Enzyme inhibition (cont.)
- Examples
- Cimetidine (anti-ulcer) inhibits the metabolism
of warfarin (anticoagulant). - Some antifungals and antibiotics inhibit CYP3A4
which oxidizes - terfenadine leading to excessive blood levels
and arrhythmias. - Fluoxetine (Prozac) is an inhibitor of
microsomal oxidation (CYP2D6). - Grapefruit juice inhibits metabolism of
cyclosporin.
38
3. Variability with Regard to the Drug Itself -
Differential Metabolism of Optical Isomers
(Enantiomers). e.g. The biologically
inactive (R)-ibuprofen is converted to the
active (S)-form via metabolic conversion to a
coenzyme A ester.
Many drugs are now marketed as single enantiomers
(e.g., Nexium is single enantiomer of Prilosec).
39
Elimination of drug and metabolites from the body
- since excreta (e.g. urine) are more waterlike
than the body as a whole, water soluble forms of
the drug are required. A. Renal Excretion
V. DRUG EXCRETION
40
A. Renal Excretion (cont.)
- 1. Glomerular filtration - Only unbound (free)
drug in blood. - 2. Proximal tubular transport - secretion into
urine. - a. Two systems involved
- i. one for organic acids
- ii. one for organic bases
- b. Competition for transport mechanism.
- Example. Probenecid and penicillin, to
retain penicillin in the body - 3. Distal tubule.
- a. Reabsorption by passive diffusion
- b. Can be modulated by pH of urine
- i. Enhance excretion of acids by increasing
urine pH .
41
1. Active transport of polar molecules,
especially anionic (i.e. negatively charged)
molecules, into bile. 2. Drug metabolites
eliminated by biliary excretion tend to be
comparatively large (molecular weight 300)
molecules glucuronic acid conjugates in
particular.
B. Biliary Excretion
3. Enterohepatic recirculation a. tends to
prolong duration of drug in the body b. can
be interrupted by diarrhea, antibiotic therapy
Enterohepatic recirculation
42
SUMMARY OF CLINICAL SIGNIFICANCE OF DRUG
DISPOSITION EFFECTS A. Some clinically
significant drug disposition effects which can
lead to variability in drug blood levels and
therefore variability in pharmacological
response 1. Binding to materials in GI tract
(reduces absorption). 2. Plasma protein
binding (protein concentration, competition
effects). 3. Biotransformation (induction,
inhibition, genetic variation). 4. Renal
active transport competition. 5. Hepatic and
renal blood flow effects. 6. Urinary pH
effects. 7. Hepatic and renal disease
effects. 8. Alterations of gut flora.
43
B. Treatment of drug overdose
- 1. Supportive treatment - treating the
patient, not the poison. - 2. Antidotal treatment - available for
relatively few drugs. - 3. Treatment based on altering drug
disposition - a. Retard absorption by
- i. emesis
- ii. gastric lavage
- iii. charcoal
- iv. catharsis
- b. Alter distribution - little can be done
- c. Alter biotransformation - retard formation
of toxic metabolite - (to be discussed in Toxicology section).
- d. Enhance urinary excretion
44
- REVIEW QUESTIONS
- ___1. Active transport of an acid drug from blood
to urine in the proximal tubule - a. may be increased by lowering the pH of the
urine - b. may be inhibited by administering another
acid drug - c. decreases the systemic clearance compared to
a drug which is not actively transported - d. increases the elimination half life compared
to a drug which is not actively transported - e. increases the apparent volume of distribution
compared to a drug which is not actively
transported. - ___2. Biotransformation of a drug most generally
leads to - a. a decrease in the pKa
- b. a decrease in water solubility
- c. a decrease in molecular weight
- d. a decrease in biological activity.
- e. a decrease in the duration of the drug in the
body - ___3. A drug of structure CH3(CH2)4CH(CH3)-NH2
, pKa 9.4, would be, - a. predominantly in the nonionized form in pH
1.4 gastric juice - b. more than half ionized in pH 7.4 plasma
45
- ___5. A patient on chronic therapy with an
anticoagulant drug eliminated by P450 (CYP)
oxidation is started - on therapy with an antiulcer medication known to
inhibit P450 (CYP) oxidative metabolism. The
likely result is - a. a need to increase the dose of anticoagulant
- b. a reduced antiulcer effect compared to
patients not on an anticoagulant - c. an excessive anticoagulant effect
- d. a shorter half life for the anticoagulant
- e. a lower than normal dose of the antiulcer
medication since it inhibits its own metabolism. - ___6. Urinary excretion of a basic drug could be
- a. increased by aspiration of gastric juice
- b. increased by raising the pH of the urine
- c. increased by inhibiting the proximal tubular
active transport of bases from blood to urine - d. increased by lowering the pH of the liver
interstitial fluid - e. none of the above
- ___7. One hundred percent of an oral dose of drug
X is excreted within 24 hours as metabolites in
the urine. - Drug X
- a. has a bioavailability of 100
- b. is extensively metabolized on its first pass
through the liver
46
- ___9. Which of the following are required to get
net transfer of a drug across a - membrane barrier by passive diffusion?
- a. a higher concentration of total drug on one
side of the membrane - b. a higher concentration of nonionized drug on
one side of the membrane - c. an ionizable group on the drug molecule
- d. a drug carrier protein in the membrane
- e. all of the above
- ___10. Since phenytoin is less bound to plasma
proteins in the uremic patient, the dose - needed to achieve therapeutic effect would be
expected to be - a. higher than in the normal patient
- b. the same as in the normal patient
- c. lower than in the normal patient
- d. lower or the same as the normal patient
dependent upon whether or not the - patient was a slow oxidizer phenotype
- e. higher or the same as the normal patient
dependent upon whether or not the - patient was a slow oxidizer phenotype
47
ANSWERS TO REVIEW QUESTIONS1. b. 6. e.2. e. 7
. c.3. b. 8. b.4. e. 9. b.5. c. 10. c.





























![[PDF] Handbook of Drug Metabolism, Third Edition (Drugs and the Pharmaceutical Sciences) Free PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10079870.th0.jpg?_=20240717015)
![[PDF] SAR: Side Effects and Drug Design (Medicinal Research Series, Vol. 11) 1st Edition Kindle PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10096837.th0.jpg?_=202408120312)