Diagnosis of Acute PE - PowerPoint PPT Presentation
1 / 13
Title:
Diagnosis of Acute PE
Description:
... explained by another condition (pneumonia, bronchitis), radiography explained by ... Good for revealing other cause for dyspnea, etc. (mass, pneumonia, COPD, etc) ... – PowerPoint PPT presentation
Number of Views:120
Avg rating:3.0/5.0
Title: Diagnosis of Acute PE
1
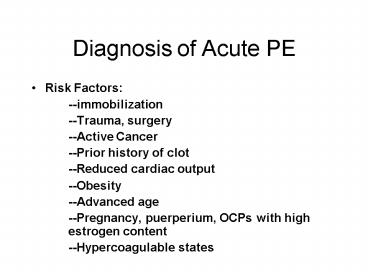
Diagnosis of Acute PE
- Risk Factors
- --immobilization
- --Trauma, surgery
- --Active Cancer
- --Prior history of clot
- --Reduced cardiac output
- --Obesity
- --Advanced age
- --Pregnancy, puerperium, OCPs with high
estrogen content - --Hypercoagulable states
2
Pathophysiology of Acute PE
- Presentations acute minor (dyspnea, pleuritic
pain, hemoptysis normal PAP and RAP) - Acute massive right heart strain with or without
hemodynamic compromise - Subacute massive progressive dyspnea and right
heart strain - Mechanism(s) of hypoxemia VQ mismatch
(unembolised areas are relatively overperfused
with insufficient ventilation to match), Shunting
(areas of atelectasis or infarction), low mixed
venous oxygen saturation (if CO reduced), loss of
surfactant
3
Estimating the pretest probability
- High (85 likely) otherwise unexplained sudden
onset of dyspnea, tachypnea, or chest pain and at
least TWO of the following - --significant risk factor present, syncope with
signs RV strain, signs of possible leg DVT,
radiographic signs of infarction, plump hilum, or
oligemia - Low (dyspnea and tachypnea and chest pain, OR these
are present but can be explained by another
condition (pneumonia, bronchitis), radiography
explained by another process, anticoagulated - Intermediate (15-85 likely) neither low nor
high
4
Diagnostic Strategies
- D-dimer only useful in ruling out PE in the
outpatient setting with low clinical likelihood. - V/Q scan most useful when chest radiograph is
normal. A normal scan virtually rules out PE. A
nondiagnostic scan, when combined with clinical
likelihood - Pre-test Prob
- Result low intermediate high
- Low 4 16 56
- Intermediate 16 28 88
- High 40 66 96
- (percentage probability of existing PE)
5
Diagnostic Strategies
- Spiral CT sensitivity and specificity overall
are in the low 90 range. Drops off for
peripheral PE. Good for revealing other cause
for dyspnea, etc. (mass, pneumonia, COPD, etc) - If CT is negative and clinical suspicion still
high, need to pursue other tests dopplers,
pulmonary angiography, MRI, etc
6
Treatment of Acute PE
- Suspect PE and no strong contraindication for
heparin begin Heparin - Pain control
- Supplemental 02
- Hypotension in RV failure the CO is highly
dependent on preload. Infuse volume. Norepi is
catecholamine of choice if needed - Avoid vasodilators as this will drop preload and
worsen the problem
7
Heparin
- Efficacy depends on achieving a critical
therapeutic concentration within the first 3
hours of treatment (aPTT 1.5-2.5x) - Use weight based nomograms
- Does not lyse clot, but prevents new fibrin
deposition on the existing thrombus - Prompt anticoagulation with heparin followed by
at least 3 mo. Oral anticoagualtion results in
80-90 risk reduction for recurrent PE
8
Heparin
- When the workup is positive the correct duration
of heparin treatment in the literature is at
least a week - Can switch to LMWH which allows subQ
administration (outpatient) monitoring only
needed in renal failure or extreme obesity (Anti
factor Xa assay). - Overlap with oral 5days
- Hemorrhagic complications up to 15, serious
- Risk factors bleeding diathesis, uremia, age,
recent surgery/trauma, hypertension, GI bleed,
antiplatelet drugs - If contraindication to heparin lepirudin
9
Thrombolytics
- Initial study Goldhaber et al 1993 looked at
patients with RV dysfunction and hemodynamic
compromise and showed a mortality benefit - Later, one small study looked at pts with RV
dysfunction on an echo and no hemodynamic
compromise. - This study showed significant benefit in
resolution of echo findings (RV strain, etc) but
did not show any benefit in mortality.
10
Thrombolytics
- One large nonrandomized registry of 719 pts
showed that in the group that got lytics the
mortality at 30 days was significantly lower
(4.7 v 11.1) - Recurrent PE also less frequent (7.7 vs. 18.7)
- Inclusion criteria clinical, echocardiographic,
or right heart cath findings of hypotension,
shock, RV dysfunction, pulm HTN, together with
() lung scan OR - Positive lung scan with three of the following
syncope, tachycardia, tachypnea, hypoxemia, EKG
findings of RV strain
11
Thrombolytics
- What about catheter directed lytics? No data,
studies to date indicate central or peripheral
admin is the same - Unlike MI, the window for lytics in PE is longer,
with benefit up to 10-14 d after onset of
symptoms
12
Pulmonary embolectomy
- Emergency situations (i.e. to prevent death)
- Mortality in the range of 33 without arrest,
43-84 in those resuscitated - Catheter techniques still developing, mortality
during extraction 30, rotational devices for
mechanical thrombolysis are experimental
13
Oral Anticoagulation
- No preexisting risk factor 6 months
- Active tumors, thrombophilic d/o, recurrent
thromboembolism, pulm HTN lifelong - Other risk factors that may be modified (estrogen
use, immobilization) duration may be shortened - Filters failed adequate anticoagulation, or
cannot anticoagulate