1) SMAs - PowerPoint PPT Presentation
Title: 1) SMAs
1
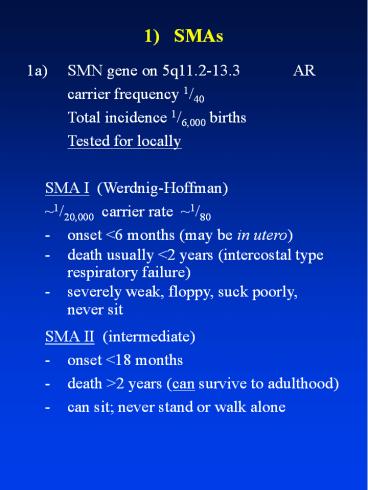
1) SMAs
- 1a) SMN gene on 5q11.2-13.3 AR
- carrier frequency 1/40
- Total incidence 1/6,000 births
- Tested for locally
- SMA I (Werdnig-Hoffman)
- 1/20,000 carrier rate 1/80
- - onset lt6 months (may be in utero)
- - death usually lt2 years (intercostal type
- respiratory failure)
- - severely weak, floppy, suck poorly,
- never sit
- SMA II (intermediate)
- - onset lt18 months
- - death gt2 years (can survive to adulthood)
- - can sit never stand or walk alone
2
1) SMAs
- SMA III (juvenile - Kugelberg-Wielander)
- - onset gt18 months
- - death - adult (can have normal lifespan)
- - walk alone
- - proximal distal weakness, legs gt arms
- All 3 have
- - symmetrical muscle weakness/wasting (proximal
gt distal) - - decreased or absent DTRs
- - fasciculations tongue, but not EOM, facial,
diaphragmatic or myocardial involvement - - tremor hands
- (These distinguish them from distal SMAs.)
- - normal SNAPS, and motor NCVs gt70 N
- (These distinguish them from CMT2.)
3
1) SMAs
- Genetic mechanism
- - In mice, SMN deletion is embryonic lethal
(mice have only 1 copy of SMN). - - In SMA I, 95 have SMNt exon 7 (and 8)
deletions but SMA II and III can as well. - - Deletion of SMNc has no effect.
- - Is a tight correlation between level of SMN
protein expression and phenotype. - - SMNc produces an alternatively
spliced protein, lacking exon 7. In SMA
III, SMNt gene is converted to an SMNc gene,
partially rescuing the phenotype.
4
1) SMAs
- 1b) Other forms of SMA
- - SMA IV (adult)
- - much rarer. Can be AR or AD.
- - distal SMA (childhood/adult)
- - 10 of all SMA 15 of peroneal
muscular atrophy - - (many other rarer kinds described)
- - adult onset GM2 gangliosidosis (Tay- Sachs)
- cerebellar disease Ashkenazim.
5
1) SMAs
- 1c) X-linked bulbo-spinal muscular
atrophy (Kennedys syndrome) - Tested for locally
- Clinically
- - onset of wasting typically 30-50 years slow
progression (decades) - - muscle cramps almost universal can precede
wasting by 20 years - - limb girdle weakness/wasting, usually in lower
limbs first most develop milder distal weakness
later - - bulbar involvement - tongue, facial,
jaw muscles - - prominent tongue fasciculations
- - myokymia of chin (?fasciculation)
- - may ultimately aspirate
6
1) SMAs
- - postural tremor 50-100
- - DTRs decreased or (usually) absent
- - may have mild distal sensory loss
great majority (gt85) have abnormal SNAPs - - gynaecomastia in 50 sexual function usually
normal, though testicular size may be reduced - Genetic mechanism
- - CAG triplet repeat expansion in exon 1 of
androgen receptor gene - - not just loss of function this
causes testicular feminisation - - probably combination of gain of novel function
plus partial loss of function
7
2) ALS
- Background
- - about 5-10 of ALS is dominant (FALS)
- - about 20 of FALS is due to SOD1 mutations
(21q22.1) - about 2-7 of sporadic ALS is also due to SOD1
mutations (SOD1 mutations testable in Perth
(? and Sydney)) - - 50 penetrance by age 46 90 by age 70
- Clinical features
- - identical to sporadic ALS (see El Escorial
criteria), but pathologically FALS may have
more posterior column damage - (Do not confuse with X-linked BSMA, or
FTDP-17.)
8
2) ALS
- Genetic mechanism
- Over 50 point mutations in Cu-Zn SOD
- (SOD1) gene
- - some characteristic genotype-phenotype correlat
ions - e.g.
- - A4 V/T - lower limb onset, rapid
progression - - I 113T - often sporadic - ?low
penetrance - - D90A - high prevalence
- (2) northern Sweden
- - behaves recessively (but
dominantly elsewhere)
9
2) ALS
- Not due to loss of SOD1 activity
- - transgenics vs. knockouts
- - SOD1 mutants may result in decreased, normal
or increased SOD1 activity - - no deletion or premature stop
codon (nonsense) mutations recorded - - may be due to aggregation of abnormal protein,
or increase of peroxidation capacity
10
3) Inherited Neuropathies
- 1) CMTs ( HMSNs) 1/2,500
- a) CMT1 ( HMSN1)
- median motor NCV ?38 m/sec.
- (? ?42) m/sec.
- (females with CMTX may have normal NCVs)
- Locus Gene Mechanism
- CMT1a 17p11.2-12 PMP22 AD Duplication (80)
(tested locally - FISH)/point (lt1)
mutation (tested Sydney) - CMT1b 1q22-23 P0 AD Point mutation (6)
(tested Sydney) - CMT1c 10q21.1-22.1 EGR2 AD Point mutations
- CMTX Xq13.1 CX32 XR/D Point mutations (12)
- (may have NCV ?43 m/sec. (tested Sydney)
- in males)
- Others
- Note that occasional patients with CX32
mutations and - some specific P0 mutations may have a CMT2
phenotype.
11
3) Inherited Neuropathies
- Clinical
- - distal weakness commencing peroneal muscles
and progressing to remainder of distal leg and
hand muscles - - sensory features very mild/inapparent
clinically - - DTRs diminished/absent
- - pes cavus/claw toes common
- - enlarged nerves may be felt
- - typically mild - most patients retain full
mobility/independence (20 have significant
disability) - ( - recessive CMT1 (labelled CMT4) is
typically earlier onset/much more severe) - Note- PMP22 duplication causes 70 of all
- CMT1
12
3) Inherited Neuropathies
- b) CMT2 ( HMSN2)
- median motor NCV gt42 m/sec.
- (less common - 30 of CMT)
- Locus Gene Mechanism
- CMT2a 1p36 ? ?
- CMT2b 3q21 ? ?
- (unusually severe
- sensory features)
- CMT2c ? ? ?
- ( respiratory failure)
- CMT2d 7p14 ? ?
- CMT2e ? ? ?
- Clinical
- - like CMT1 except tendency for
- - later onset
- - more severe weakness/atrophy legs (?
less hands) - - relatively better preservation of DTRs
13
3) Inherited Neuropathies
- c) Dejerine-Sottas Syndrome (HMSN3) (rare)
- (some require median motor NCV lt10 m/sec most
do not - overlaps with severe CMT1 clinically) - Clinical
- - severe, infantile/childhood onset,
hypertrophic dysmyelinating neuropathy (
onion bulbs) with enlarged nerves - - may have raised CSF protein
- Genetic
- - previously considered recessive as most are
sporadic, BUT - - most have dominant (new) mutations of PMP22
or P0 (about equal numbers) dominant EGR2
mutations have occurred - - can have homozygosity for PMP22 duplication
or P0 mutation
14
3) Inherited Neuropathies
- 2) HNPP (tomaculous neuropathy) - AD
- Clinical
- - painless mononeuropathy developing after
minor trauma or compression typically resolves
in days-weeks - - may show signs of more generalised
neuropathy, like CMT1 - - usually find slowing of lower limb NCVs and
median distal latencies, as well as symptomatic
focal conduction block - Genetic
- - great majority PMP22 deletion (tested locally
- FISH) - - a few PMP22 mutations, or non PMP22
15
3) Inherited Neuropathies
- 3) Hereditary neuralgic amyotrophy (familial
brachial plexus palsy) - AD - - typical attacks of (painful) brachial
neuritis, may begin in childhood usually
teens - 20s - - axonal damage no evidence of generalised
neuropathy. Recovers over months - - may have hypotelorism/short stature
- - also Ch17, but 17q23-25, not 17p11.2-12
- Note- distinction of HNA from HNPP which may
affect plexus (10), but - - is painless
- - has mild NCV decrease in legs
- - does not have dysmorphic features
16
3) Inherited Neuropathies
- 4) Sensory Neuropathies (HSANs)
- HSAN I ( AD hereditary sensory neuropathy)
9q22.1-22.3 - - onset teens-20s
- - usually with painless foot ulceration/neurop
athic joints may be with burning feet or
lancinating pain - - unmyelinated/small myelinated fibres affected
first - - minimal autonomic/motor involvement
- - DRGs and distal axonal
- HSAN II ( AR sensory neuropathy) ?locus
- - onset infancy/childhood
- - all forms of sensation affected - severe
ulceration, and loss of DTRs - - minimal autonomic involvement
17
3) Inherited Neuropathies
- HSAN III ( Riley-Day syndrome) 9q31-33
- - overriding feature loss of unmyelinated
C-fibres with severe autonomic dysfunction - - most have pain/temperature loss, and some
lose larger fibre function. Absent histamine
triple response - - AJs depressed/absent
- - fungiform papillae absent from tongue
- - often short stature, may have
kyphoscoliosis - - (?nearly) all are Ashkenazim
18
3) Inherited Neuropathies
- HSAN IV
- ( hereditary anhidrotic sensory neuropathy,
congenital insensitivity to pain with
anhidiosis) - - AR, due to trkA receptor (for NGF) mutations
(in some families, at least) - - all unmyelinated nerve fibres lost,
myelinated fibres preserved
19
3) Inherited Neuropathies
- 5) FAPs (Familial amyloidotic polyneuropathies)
- Most are due to one of many point mutations in
the transthyretin (TTR) gene. - Clinical
- - neuropathy, usually lower limbs first, in
nearly all, sensory before motor, small before
large fibre - - autonomic features common
- - other features may be seen - CTS,
cardiomyopathy, vitreous deposits
20
Hereditary Spastic Paraplegia
- Clinically divided into pure and
- complicated
- Pure HSP
- History
- - onset usually teens - 30s, but can be
infancy to 80s - - typically slowly/relentlessly progressive
- - bladder involvement may occur late
- Examination features
- - cranial nerves (JJ, rapid tongue movements)
normal - - upper limb reflexes typically brisk with
spread, Wartenbergs thumb sign, but tone and
power normal - - lower limb tone increased, clonus
21
Hereditary Spastic Paraplegia
- - lower limb power often decreased, especially
hip flexors/ankle dorsiflexors - - lower limb hyperreflexia spread. Plantars
usually extensor abdominal reflexes often
preserved - - sensation usually normal may have mild
vibration perception loss - - may have pes cavus
- Complicated HSP
- - pure HSP other features such as
- - ataxia
- - peripheral sensory loss/ mutilation
- - amyotrophy
- - retinitis pigmentosa
22
Hereditary Spastic Paraplegia
- Genetics of pure HSP
- Most cases dominant (or just better
ascertainment) - - AD - at least 7 defined loci
- - only SPG4 (spastin) cloned to date
(2p) (commonest AD HSP, gt40, - not tested
for routinely) - - nuclear ATPase
- - 39 point mutations found throughout
17 exons, so hard to test - - AR - at least 2 loci defined
- - only SPG7 (paraplegin) cloned to
date (16q) - - ATPase in mitochondria (have RRFs)
- - not tested for routinely
23
Hereditary Spastic Paraplegia
- Spastin mutation phenotype
- - 25 non-penetrant or only detected on exam
- - mean onset age 29, but range wide (infancy -
79!) - - progression highly variable, but
significantly faster in those with late onset
(gt35 years) - - associated signs (weakness, wasting,
decreased vibration perception, sphincter
disturbances) related to disease - - not always pure - cognitive impairment and
epilepsy seen rarely
24
Hereditary Spastic Paraplegia
- Genetics of Complicated HSP
- X-linked
- i) LI-CAM mutations (SPG1)
- CRASH syndrome
- (corpus callosum agenesis, retardation,
adducted thumbs, spastic paraplegia,
hydrocephalus) - includes MASA syndrome - ii) PLP mutations (SPG2)
- Pelizaeus-Merzbacher disease
- - widely variable severity, from infantile
hypotomia/nystagmus/pyramidal/
cerebellar/dystonia, to complicated HSP, to
pure HSP - - female carriers may manifest
- AD or AR
- (Only gene found to date is for ARSACS
Charlevoix-Saguenay spastic ataxia - only
identified in French-Canadians to date)
25
Hereditary Spastic Paraplegia
- Differential diagnosis of HSP
- - major problem is with isolated case
- - other genetic causes
- - AMN (isolated male)
- - SCAs
- - DRD (therapeutic trial)
- - structural causes (do not forget
tethered cord, AVM) - - degenerative causes
- - MS
- - PLS variant of MND
- - infectious causes
- - TSP, HIV (subacute courses)
- - metabolic causes
- - B12, lathyrism
26
Friedreichs Ataxia
- AR - equal commonest genetic ataxia of
childhood (1/40,000) - - carrier rate 1/100
- Classical Clinical Picture
- - onset 8-15 years can be as late as 25
- - within 5 years of onset should have
- - progressive limb and gait ataxia
- - absent lower limb DTRs
- - extensor plantars
- - median motor NCV gt40 ms-1, with reduced
or absent SNAPs - - within 10 years of onset should have
- - dysarthria
27
Friedreichs Ataxia
- - most patients also have
- - scoliosis
- - abnormal ECG/ECHO (but cardiac
symptoms rare until preterminal) - - abnormal ocular pursuit (nystagmus
lt50) - - pyramidal weakness in legs
- - a minority of patients also have
- - glucose intolerance (20 10
diabetic) - - optic atrophy (30)
- - sensorineural hearing loss (20)
- (Note- MRI typically does not show cerebellar
atrophy) - BUT this is too restrictive! Since gene test,
- many non-classical presentations recognised
- i) LOFA - late-onset FA - gt25 years and can
be in 50s-60s. Often preserved reflexes, no
cardiomyopathy, slow progression
28
Friedreichs Ataxia
- ii) FARR - FA with retained reflexes.
Reflexes can be brisk. Most patients with
Hardings AR ataxia with preserved reflexes have
this. - iii) Acadian ataxia - a milder variant in
Acadians (ex French-Canadians) - iv) Assorted others (rare) - e.g. spastic
paraplegia, pure sensory ataxia,
chorea/myoclonus - Genetic Mechanism
- - GAA triplet repeat expansion in intron 1 of
frataxin gene (9q). 95 - - rarely point mutations (various)
- - severity inversely proportional to amount of
residual gene product (-/- mice are not viable) - - longer GAA repeats decrease product
more, so severity depends on length of
shorter repeat - - double point mutations probably lethal -
do not occur
29
Friedreichs Ataxia
- - frataxin - mitochondrial protein - absence
causes iron accumulation and excess oxidative
stress - - idebenone reported to reverse cardiomyopathy in
part - Prognosis
- - variable - gt95 of classic patients
wheelchair-bound by age 45 - - typically wheelchair-bound about 15
years after onset - - mean age of death mid-30s, but normal
survival possible if no cardiomyopathy or
diabetes - Imitators (genetic)
- i) AVED (isolated Vitamin E deficiency)
- - mutations in ?-tocopherol transferase
(8qB) - - FA-like, with fine retinal
pigmentation
30
Friedreichs Ataxia
- ii) Abetalipoproteinaemia and hypobetalipoprot
einaemia (not the same) - AVED-like picture - iii) NARP (neuropathy, ataxia, retinitis
pigmentosa) mitochondrial inheritance - ATP
synthetase subunit 6 point mutations - (Note- Roussy-Levy syndrome is really CMT1)
31
Ataxia - Telangiectasia
- AR - equal frequency to FA (1/40,000, so
carrier rate 1/100) - - commonest cause of inherited ataxia
before age 5 - - typically wheelchair-bound by age 10-11
- Clinical picture
- i) neurological
- - onset between infancy and 20 gait ataxia
- - may have titubation, myoclonus, chorea
- - dystonia in post-adolescent patients
- - dysarthria - slow, slurred
- - impassive facies may drool
- - ocular motor apraxia, with compensatory
head thrust - - may develop sensory loss/distal
weakness/areflexia, but plantars are flexor
32
Ataxia - Telangiectasia
- ii) non-neurological
- - telangiectases - bulbar conjunctivae
between ages 3-5, then - - pinnae, palate, elbow and knee
flexures - - recurrent sinusitis/pneumonia
- - lymphomia/leukaemia
- ( - solid organ malignancies when older)
- - marked radiosensitivity
- Laboratory tests
- - elevated ?FP and CEA (may be normal in
childhood) - - 2/3 show impaired humoral and/or cellular
immunity - - absent or low IgG2, IgA, IgE (IgG and
M normal) - - decreased DTH and T cells
- - cytogenetic studies show t(714)
translocations and radiosensitivity - - MRI - early cerebellar atrophy
33
Ataxia - Telangiectasia
- Clinical variants
- - AT sine telangiectasia
- ( - AT sine immune compromise)
- - both together constitute some, and maybe all,
of Aicardis Ataxia Ocular Motor Apraxia - Genetic mechanism
- - ATM (mutation in AT) gene 11q
- - large (gt180 kb, 3056 aas), many point
mutations, so not tested for routinely
(Research - QIMR) - - most mutations nonsense (deletions, splice
mutations, stop mutations) - - missense mutations produce milder phenotype
in homozygotes/compound heterozygotes - Note - Heterozygote carriers have increased
sensitivity to DXRT - - Female heterozygote carriers may have
increased risk of breast cancer
34
Spinocerebellar Ataxias (SCAs)
- - All AD mostly adult - onset
- - Named in order of discovery, not frequency
- - SCAs 1, 2, 3, and 6 tested locally SCA 7 in
Sydney - SCA 1 - 6q (CAG)n expansion (?39) in
ataxin 1 gene - - common(est) in Anglocelts
- - pyramidal features common - slow MEPs
- - nystagmus uncommon (lt10) but saccades
often hypermetric - - may have optic atrophy (mild)
- - MRI shows moderate pontocerebellar
atrophy
35
Spinocerebellar Ataxias (SCAs)
- SCA 2 - 12q (CAG)n expansion (?34) in
ataxin 2 gene - - commonest in Italians
- - typically - slow/viscous eye
movements - - depressed reflexes
- - may have early dementia
- - MRI typically shows severe
pontocerebellar atrophy - SCA 3/MJD - 14q (CAG)n expansion (?66) in
ataxin 3 gene - - commonest in Portuguese, Germans,
Chinese - - very variable syndrome
- spasticity, amyotrophy,
- neuropathy (may be small fibre)
36
Spinocerebellar Ataxias (SCAs)
- - may have autonomic dysfunction
(confusion with sporadic OPCA) - - may present as extrapyramidal
syndrome parkinsonism/ dystonia common - - may be ophthalmoplegia, but typically
horizontal gaze-evoked nystagmus diplopia - - MRI shows enlargement of 4th ventricle
only - SCA 4 - 16q gene unknown
- - ?frequency - may be rare
- - sensory axonal neuropathy prominent
(may be 1st) pyramidal signs - May also be a cause of pure ataxia
(ADCA III) - SCA 5 - 11 cent gene unknown
- - ?frequency
- - relatively slow course pure or
pyramidal signs
37
Spinocerebellar Ataxias (SCAs)
- SCA 6 - 19 p CACNL1 A4 gene (?1A subunit
of P-type voltage gated Ca2 channels)
CAG repeat (21-29) - - common (except in France) (equal with
SCA 1 here) - - The exception in SCAs because
- - repeat number small (and stable)
- - mutation disrupts function of Ca2
channel (not gain of novel
function) - - topography of neuropathology
matches distribution of gene product
38
Spinocerebellar Ataxias (SCAs)
- - Clinically
- - may cause later onset, slowly
progressive pure ataxia (ADCA III) -
?shorter repeats - - may cause earlier, more rapid ataxia
with pyramidal signs (ADCA I) -
?longer repeats - - Allelic with (and phenotypic overlap
with) - - EA2 - nonsense (truncating)
CACNL1A mutations - - FHM1 - missense CACNL1A mutations
39
Spinocerebellar Ataxias (SCAs)
- SCA 7 - 3p (CAG)n expansion (?38) in
ataxin 7 gene - - rare everywhere (1-2 of SCAs)
- - characterised by tritanopia leading
to visual failure (ADCA II) - - early onset lt30
- - later if later onset