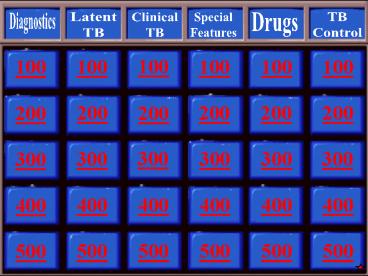
Diagnostics - PowerPoint PPT Presentation
Title:
Diagnostics
Description:
email mhamlyn_at_jessamine.k12.ky.us ... 100 100 100 100 100 200 200 200 200 200 200 300 300 300 300 300 300 400 400 400 400 400 400 500 – PowerPoint PPT presentation
Number of Views:227
Avg rating:3.0/5.0
Title: Diagnostics
1
Diagnostics
Latent TB
Clinical TB
Special Features
Drugs
TB Control
100
100
100
100
100
100
200
200
200
200
200
200
300
300
300
300
300
300
400
400
400
400
400
400
500
500
500
500
500
500
2
Jeopardy Value
Extraction of DNA hybridization of labeled PCR
products with oligonucleotide probes according
to the CDC, this must be performed on at least
one respiratory specimen from each patient with
clinical suspicion of TB, where diagnosis has not
yet been established
3
What are nucleic acid amplification tests?
4
Jeopardy Value
3 to 7 of sputum specimens have this, Less
than 50 of labs do this
5
What are tests for NAA inhibitors?
6
NAA
- CDC recommends that standardized NAA testing be
performed on at least one respiratory specimen
from each patient with clinical suspicion of TB,
where Dx has not yet been established, and for
whom the result will alter management and TB
control measures/contact investigations
MMWR Jan 2009/58(01)7-10
7
NAA
Ampl MTB direct test MTD (Gen-probe)
Enhanced Amplicor (Roche) test
Greater PPV /NPV and SS in smear positive cases )
80-95 Lower sensitivity and PPV in smear
negative cases 50 appx Earlier Detection Less
inappropriate use of FQ as empiric monotherapy
for pneumonia Reliance by MDs 20-50 of
cases NAA testing should be considered as
Critical test value notification Report time less
than 48 hours. If clinical suspicion is low, do
not do NAA as PPV low If clinical suspicion
moderate or high single NAA negative should not
be relied upon
MMWR Jan 2009
8
Interpretation of NAA
CLINICAL SUSPICION AFB smear NAA result
HIGH positive positive MTB (PPV 95) Rx Isolate and Contact investigation
HIGH Negative positive Repeat NAA if positive or clinical suspicion high Rx as TB as above
Positive negative Repeat test for Inhibitors, if none This is probably MOTT If Inhibitors present NAA no use Decision to Rx ??
Adapted from AJRD 1997 155 1804
9
Jeopardy Value
This is based on mycobacterial genomics and
antigen specific T cell response, Antigenic
targets include ESAT-6 and CFP-10
10
What is the IGRA test based on?
11
IGRA update
The blood test for TB Global caution!!
-
Advantages -
Disadvantages - TIGRA preferred but TST acceptable
Homeless /Transitional Care/ Substance abusers - TST is preferred
Children less than 5 years of
age - Equally acceptable
Contact screening ( although
higher PPV -
and NPV seen ( 3
vs. 13 and 99 vs.. - ILH current priority list
100 when compared with TST
5mm ) - Employees
Am j Resp Crit Care 2011
jan - Immune compromised patients
- Patients with Hx of BCG
- Specific cases where differential Dx of
pneumonia includes TB or MAC - Referral from Transitional Homes/ Shelters to
UCC - Ref MMWR
/CDC Rep 2010 59 (RR-5 1-28
Relationship of timing of TST to TIGRA Variable
conflicting data Present consensus no effect
on either test results or booster phenomenon or
false positivity
12
Jeopardy Value
NTM/MOTT BCG Technique
13
What are the drawbacks of TST/Mantoux test/PPD?
14
No cross-reactivity to BCG and most NTMs
Tuberculosis Complex Antigens Antigens Environmental Strains Antigens Antigens
Tuberculosis Complex ESAT-6 CFP 10 Environmental Strains ESAT-6 CFP 10
M. tuberculosis M. abcessus - -
M. africanum M. avium - -
M. bovis M. branderi - -
BCG substrain M. celatum - -
gothenburg - - M. chelonae - -
moreau - - M. fortuitum - -
tice - - M. gordonae
tokyo - - M. intracellulare - -
danish - - M. kansasii
glaxo - - M. malmoense - -
montreal - - M. marinum
pasteur - - M. oenavense - -
M. scrofulaceum - -
M. smegmatis - -
M. szulgai
M. terrae - -
M. vaccae - -
M. xenopii - -
Watch for M. MSGK
15
Updated CDC Guidelines
- CDC guidelines1 allow the use of IGRA or TST for
screening healthcare workers - An IGRA or a TST may be used without preference
for periodic screening of persons who might have
occupational exposure to M. tuberculosis (eg,
surveillance programs for healthcare workers). - IGRA preferred testing for groups with low rates
of return - IGRA preferred testing for individuals who have
received BCG - Prior to implementing IGRAs, each institution
and tuberculosis-control program should evaluate
the availability, overall cost, and benefits of
IGRAs for their own setting. - LSU/ILH guidelines When DDx includes
Pneumonia/MAC/MOTT - with employees screening
1. Updated Guidelines for Using Interferon Gamma
Release Assays to Detect Mycobacterium
tuberculosis Infection - 2010. CDC MMWR 59 RR-5.
16
Commercially Available IGRAs
- QuantiFERON-TB Gold In-Tube1
- ELISA technology
- Measures IFN-? release
- One and done
- PI sensitivity 88.2
- PI specificity 99.1
- 3 specialized tubes
- Provides qualitative results
- Sample stability 16 hours
- Can be run in hospital lab
- Available nationally through reference
laboratories (eg, Quest)
- The T-SPOT.TB Test2
- ELISpot technology
- Enumerates effector T cells
- One and done
- PI sensitivity 95.6
- PI specificity 97.1
- 1 standard tube
- Provides quantitative and qualitative results
- FDA-approved borderline category
- Sample stability 32 hours
- Can be run in hospital lab
- Available nationally through Oxford Diagnostic
Laboratories
1. QuantiFERON-TB Gold Package Insert. Cellestis,
Inc. Valencia, CA. Doc. No. US05990301K, July
2011. 2. T-SPOT.TB Package Insert. Marlborough,
MA Oxford Immunotec 2010. T-SPOT is a
registered trademark of Oxford Immunotec, Ltd.
QuantiFERON is a registered trademark of
Cellestis, Inc.
17
Questions We Ask ?
- TST and IGRAs predictors of disease General
- Does quantifying help in either case ?
- Specific Quantification in TB spot test
Culture filtrate protein 10 spot count, but not
early secretary antigenic target 6 spot count,
was significantly associated with subsequent TB
development. ( Hongkong study in silicotic pts ) - Issue of discordance Borderline data
- Effect of Smoking Negative effect of smoking on
the performance of the QuantiFERON TB gold in - tube test BMC Infectious Diseases 2012, 12379
doi10.1186/1471-2334-12-379 - IMPORTANCE OF DEFINITION OF CONVERTORS OR
REVERSION SPECIALLY IN HCWs - Challenges of IGRAs conversion in serial
testing of HCW Fong et al Chest 2012 142
(1) 55-62
18
Active Vs latent
- IGRA responses are higher in active disease than
in LTBI - However, there is a very large overlap in the
results so it will not be possible to use IGRAs
to differentiate between active disease and
latent infection
Chee et al Eur J Clin Microbiol Infect Dis (2008)
Janssens et al ERJ (2007)
T-SPOT.TB spot numbers in subjects with active
disease compared to LTBI (TSTve and TST-ve)
T-SPOT.TB spot numbers in subjects with active
disease compared to LTBI
19
Explaining discordant results TNF screening
- 70 subjects attending a rheumatology clinic in
Athens - All candidates for anti-TNF therapy
- 43/70 on immunosuppressive drugs
- 15/70 had co-morbid conditions (e.g. chronic
liver disease, diabetes, COPD) - Results of TST and the T-SPOT.TB test compared,
multivariate analysis used to analyse discordant
results
TST TST TST TST
T-SPOT.TB - Total
T-SPOT.TB 12 4 16
T-SPOT.TB - 15 39 54
T-SPOT.TB Total 27 43 70
Vassilopoulus et al., J Rheumatology (2008)
(BCG) vaccination was associated with
TST/Elispot discordant results (p 0.01),
whereas steroid use was linked to TST/Elispot
discordant results (p 0.04).
20
Jeopardy Value
Must check for active TB Do not forget to look
for extra- pulm TB
21
What do you do before starting treatment for
latent TB?
22
A positive TST / IGRA
suggested plan
JALI
A DATA B EVALUATE C
SCAN D RECAP
E TREAT
QUANTIFY ASSESS BORDERLINE INDETERMINATE DISCORDANT RESULTS RULE OUT ACTIVE DISEASE RULE OUT EXTRA-PULM DISEASE SIZE OF TST is it helpful? IN CHILDREN Degree of IGRA ?? Dx LTBI Should we offer Rx? Based on many factors
DOCUMENT SYMPTOMS H/P ROS LN EXAM GO BACK to STEPS BC IF IN DOUBT RISK OF ADR
CHECK HIV CXR CT Scan if needed CORRELATE with Chest imaging PRE-LAB CHECK
STRATIFY RISK, CHECK SOURCE CASE WHY??? SPUTUM INDUCE if needed PRE-TEST PROBABILITY? IF SURE GO TO STEP E TREAT FOR LTBI. ASSESS RISK BENEFIT RATIO
CONCLUDE AFTER FULL EVALUATION IF POSITIVE STEPS B-E PRE-TEST PROBABILITY? TREAT FOR ACTIVE TB ? TREAT FOR TB ? MONITOR SIDE EFFECTS AND Rx
steps
ATS 2006 DILI consensus statement
23
Jeopardy Value
Must be DOT and it is not treatment for active TB
24
What is chemoprophylaxis for latent TB by
intermittent therapy? Ripaentine / INH weekly
25
Jeopardy Value
13 to 22 of cohort can acquire disease form
this group
26
What is Smear negative TB?
27
The hidden reservoir of TB
- Smear negative cases 13-22 of cohort can
acquire disease from smear negative contacts - Undocumented immigrants with prolonged symptoms
with poor access to health care - ( CID 2008 Tostmann et al)
- (Achkar et al Clin Infec Dis 2008
Nov) - Delay in Dx, Index of suspicion
( Surgical specialties) - Am J Med science 340 Nov 2010)
- Note
- Infectious period 3 months prior to onset
of symptoms - Only 20 of contacts with LTBI complete
Rx. Need to expand contact screening for Smear
negative TB - (
28
Suspect cases
- ILH data
- Suspect TB cases require Resp Isolation
- Average cost of care 20 K per pt
- ALOS may be as high as 22.7 days
29
When to hospitalize and when to discharge Basis
NYC Health Dept criteria
Latent TB TB Low Suspicion For TB
IN-Patient
ED
When to discharge Avoid weekends Check pt
infection and clinical factors Co morbid
conditions Home and follow up situations. Depends
upon where discharged to
When to admit? Cavitary disease / Hx
Substance abuse Unstable medical /psych /social
conditions or unclear follow up situations
30
Jeopardy Value
Compliance No DOT Increase bacterial
burden Development of secondary
resistance Malabsorption of Drugs Host variation
in response to drugs lab error
31
What are The causes of delayed sputum conversion
and/or treatment failure?
32
Therapy
- Ideal Rx DOT RIPE
- Duration 6 months .. 9 months in
- special case scenarios
- When sputum culture is still positive at the
end of 2 months - CXR showed cavitary disease/ Initial high
bacterial load - When initial induction phase did not include
PZA - When induction phase was not standard i.e.
once weekly doses
33
Jeopardy Value
Sputum culture is positive after 2 months
Cavitary, heavy smear positive disease PZA of
RIPE not used.
34
When Do you extend treatment beyond 6 months?
35
Jeopardy Value
No SM No PZA in USA 9 months at least Vitamin B6
a must
36
What is TB treatment in pregnant womem?
37
Jeopardy Value
Side effects may be due to longer intervals of
dosing rather then the actual dose We may be
using a lower dose than is needed
38
What is Rifampin and ? issues with standard
dosage?
39
Jeopardy Value
23 of MDR-TB are this
40
What is XDR-TB?
41
RISK Factors for DR MDRTB and XDRTB
- Inadequate Rx protocols and non compliance
- Question of low level resistance and importance
there of - Previous TB Rx OR 11 HIV OR 3 , Homelessness OR
3, ETOH abuse OR 2 - ( Annals June 2009 )
- Rifampin Resistance is an excellent marker for
MDRTB
42
Where are we moving forward ?
- Old drugs Newer drugs and newer class of drugs
( focus has moved to out of USA to Japan , India
) - Other approaches targeting MTB proteins
- Drug delivery Inhaled administration
- Revisit Rifampins ( Dose, toxicity concerns (
immunologic and idiosyncratic ) , association
with PZA , Drug levels, D-D interaction ) - Caution about Flouroquinoles
- Mitnick et al NJMRC Denver Expert Opinion
Pharmacoth 2009 - ( Nature 2009 Lin et al )
43
Jeopardy Value
KatG gene aphC gene
44
What is the the genetic basis of INH resistance?
45
Detecting drug
resistance ?? Rifampicin resistance Mutations
in ß subunit of RNA polymerase ?? gt90 of
mutations in 81 base pair region ?? Isoniazid
resistance more complex ?? katG gene
(peroxidase) mutations ?? inhA gene mutations
cell wall synthesis ?? others - aphC gene
mutations ??PCR-based detection ?? GenoType
MTBDRplus (Hain Lifescience) ??
USED RECENTLY AT WETMORE
46
Jeopardy Value
It is not coming soon It is here 90
sensitive/specific
47
What is The XPERT Test?
48
Detecting drug
resistance ?? Rifampicin resistance Mutations
in ß subunit of RNA polymerase ?? gt90 of
mutations in 81 base pair region ??
Isoniazid resistance more complex ?? katG gene
(peroxidase) mutations ?? inhA gene mutations
cell wall synthesis ?? others - aphC gene
mutations PZA mutations in gene
pncA ?? ?? PCR-based detection line probe
assay ?? GenoType MTBDRplus (Hain Lifescience)
XPERT Testing FIND Inititative It is not
coming soon, it is here ( 90 S/S)
NEJM , Eur Pub June 2011 ??
49
- Delayed conversion
- Increased bacterial load
- ??Erratic Drug response and levels
- Increased rates
- Double jeopardy
Jeopardy Value
50
Relapse of PTB after sputum conversion after SCC
- Followed for 3 years
- 3.29
- Those who became smear negative after 3 months of
Rx had a relapse rate of 8.8 - Relapse rate about 10 in Diabetics
- CDC data from NC Public health dept
51
High risk for treatment failure or relapse
HIV / DM When second line Rx used
- Cavitation on initial CXR
- Positive Sputum Culture after 8 weeks of Rx.
- When PZA is not used in the Intensive phase
- US PHSS 22 TB Consortium trial 1993-2002 cohort
and ATS guidelines
52
Relapses
- In nearly all patients with TB caused by drug
susceptible organisms and who are treated with
Rif containing regimens using DOT Rx, relapses
occur with susceptible organisms
53
Jeopardy Value
Dec levels Reported in TB patients Decreased
levels /Receptor polymorphism associated with
increase susceptibility to MTB Can suppress
intracellular growth of MTB in vitro Induces
expression of autophagy, phagosomal maturation,
antimicrobial peptides such as cathelicidin Enhanc
es the activity of PZA
54
What is Vitamin D?
55
VITAMIN D
- TB and nutritional deficiency A historical fact
- Vit D deficiency reported in TB pts
- Vit D receptor polymorphism associated with
increased susceptibility to MTB - Vit D can suppress intracellular growth of MTB in
vitro - Vit D also induced expression of autophagy,
phagosomal maturation, antimicrobial peptides
(cathelicidin, - Enhanced activity of PZA
- Amer Jour Med Sciences 341 June 2011 Science
Tran s Med Oct 11
56
Jeopardy Value
Seen in at least one TB drug in about 46 of
cases Data shows significant scatter
57
What are Low drug levels?
58
Drug levels
- Thee et al In J Tuberc 2007 (9) 937
- Um et al In J Tuberc 2007
- Kimerling et al Chest 1998
Done at wetmore
- Due to PK and PD variability it is better to use
Body surface area ,especially in children to
decide dosage and achieve better therapeutic
levels - Low 2 hr serum conc of at least one Anti TB
drug was seen in about 46 - INH associated with acetyl INH/INH ratio and ETH
associated with Cr Cl - However significant scatter noted, many variables
such as ETOH use , fixed combination etc and
hence clinical relevance unclear. Importance of
looking at the therapeutic level range
59
Drug levels
- Thee et al In J Tuberc 2007 (9) 937
- Um et al In J Tuberc 2007
Done at wetmore
- Body weight or Body surface especially in
children - Low 2 hr serum conc was 46 INH and Rifampin
mainly associated with dose/kg weight - INH associated with acetyl INH/INH ratio and ETH
associated with Cr Cl - However significant scatter noted and clinical
relevance unclear
60
(No Transcript)
61
(No Transcript)
62
Observation
- We observed at Wetmore Clinic in our random ,
haphazard analysis that TB patients with DM were
requiring higher dosage of TB Meds based on their
drug level data . This was specially seen with
PZA and Rifampin
63
Hypothesis
- Patients who have diabetes and TB have lower
blood drug levels of PZA , compared to patients
with TB without DM
64
- WE are looking at Rifampin levels and data , but
do not have that yet
65
- PZA levels
Descriptive Statistics Descriptive Statistics Descriptive Statistics Descriptive Statistics Descriptive Statistics Descriptive Statistics
N Minimum Maximum Mean Std. Deviation
INH 245 0 25 6.53 4.943
RIF 242 0 34 10.09 7.052
PZA 117 0 100 40.13 19.806
Valid N (listwise) 67
1. There were repeats and missing data cases
among those 117 cases. Once the data was cleaned,
this was the outcome
Group Statistics Group Statistics Group Statistics Group Statistics Group Statistics Group Statistics
DIABSTATUS N Mean Std. Deviation Std. Error Mean
PZA 1.0 5 34.800 13.4425 6.0117
PZA .0 38 49.921 24.0106 3.8950
2. Of the 117 instances, 43 were true PZA
individual cases.
Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test Independent Samples Test
Levene's Test for Equality of Variances Levene's Test for Equality of Variances t-test for Equality of Means t-test for Equality of Means t-test for Equality of Means t-test for Equality of Means t-test for Equality of Means t-test for Equality of Means t-test for Equality of Means t-test for Equality of Means
F Sig. t df Sig. (2-tailed) Mean Difference Std. Error Difference 95 Confidence Interval of the Difference 95 Confidence Interval of the Difference
F Sig. t df Sig. (2-tailed) Mean Difference Std. Error Difference Lower Upper
PZA Equal variances assumed 2.924 .095 -1.370 41 .178 -15.1211 11.0333 -37.4032 7.1611
PZA Equal variances not assumed -2.111 7.912 .068 -15.1211 7.1632 -31.6712 1.4291
3. Once the data is cleaned and analyzed, the
significance level rises to above 0.05, meaning
there is no significant association. There is no
difference between the PZA levels of those that
are diabetic versus the non-diabetic group.
Verbal communication A Ghaffar MD MPHTM 2013
66
TUBERCULOSIS DISEASEDRUG LEVEL TESTING
- CRITERIA FOR TESTING
- Recurrent MTB disease of any site
- MTB cases not converting to negative sputum smear
_at_ 4 weeks - MTB cases not converting to negative sputum
culture _at_ 8 weeks - MTB case with known drug resistant organisms
- MTB case with HIV co-infection
- MTB cases with abnormal Drug Blood Level results
- Other MTB cases with administrative approval
- Drug levels that should be tested include INH,
Rifampin or Rifabutin, PZA and Moxifloxacin.
Other drugs can be tested upon
administrative approval.
67
Drug levels ? Some questions
- Present practice why the doses? RIF specially
- ( Ingen et al CID 2011 3 reasons
- Drug conc above MIC, Fear of side effects,
economic - 600mg is at a lower end of the dose response
curve side effects not dose related
idiosyncratic and immunological more, cost?) - Weight/gender/genetic variations/BSA may
determine different dose - Any reason to change practice since in most cases
of Rx failure , causes are multifactorial - Side effects may be due to longer intervals of
dosage rather than dose - Importance of tailoring Rx
- Do we re-set the clock?
68
Jeopardy Value
??
??
- Environmental/ Ingestion
- No H-H transmission
- Pauci bacillary
- Mixed infection
- Indolent
- New Infection
- Exposure
- Human to human transmission
- Latent disease
- Pauci bacillary ?
- Reactivation
- Relapse
vs.
3 to 10 incidence in clinical and laboratory
settings and data
69
- What are NTMs
70
MYCOBACTERIUM TUBERCULOSIS AND MOTT
- Over the course of 4 years, data were collected
on Mycobacterium tuberculosis and MOTT, basically
to compare the number of patients infected with
each of these organisms. Patients with MTB are
provided treatment at no cost through the Public
Health System. However, those unlucky patients
diagnosed with MOTT are on there own when it
comes to seeking treatment for their condition.
71
(No Transcript)
72
DUAL INFECTIONS
- As noted in the previous chart, there were 10
dual infections. Eight (8) of these were MTB and
Mycobacterium Avium Complex (MAC), one (1) was
MTB and Mycobacterium fortuitum and one (1) was
MTB and Mycobacterium kansasii.
73
Relapse of PTB after sputum conversion after SCC
- Followed for 3 years
- 3.29
- Those who became smear negative after 3 months of
Rx had a relapse rate of 8.8 - CDC data from NC Public health dept
74
High risk for treatment failure or relapse
HIV / DM BMC Med 2011 When second line Rx used
- Cavitation on initial CXR
- Positive Sputum Culture after 8 weeks of Rx.
- When PZA is not used in the Intensive phase
- US PHSS 22 TB Consortium trial 1993-2002 cohort
and ATS guidelines
75
Pulmonary Disease M. abscessus Worldwide may
be found concomitant with MAC M. asiaticum
Rarely isolated M. avium complex Worldwide most
common NTM pathogen in U.S. M. celatum
Cross-reactivity with TB-DNA probe M. kansasii
U.S., Europe, South Africa, coal-mining regions
M. chelonae Pulm Disease ?? . M. fortuitum
Associated with aspiration Contaminant M Szulgai
and M Chelonae and Eye disease
76
When the last ATS statement about NTM was
prepared in 1997, there were approximately 50 NTM
species that had been identified. Currently, more
than 125 NTM species have been cataloged The
increase relates to improved microbiologic
techniques and identification New cases of NTM
lung disease may significantly exceed case rates
for TB in some communities and regions ,
advances in molecular techniques with the
development and acceptance of 16S rRNA gene
sequencing as a standard for defining new species.
Clinical significance??
77
Jeopardy Value
-
Photochromogen -
Scotochromogen - Non- chromogen
78
- What is the Runyon Classification of
Mycobacterial Disease ?
79
Classification of mycobacterial species commonly
causing human disease
M. tuberculosis complex
M. tuberculosis
M. bovis
M. africanum
M. microti
M. leprae
Slowly growing mycobacteria
Photochromogens, Runyon group I
M. kansasii
M. marinum
Scotochromogens, Runyon group II
M. gordonae
M. scrofulaceum
Nonchromogens, Runyon group III
M. avium complex
M. avium
M. intracellulare
M. scrofulaceum
M. terrae complex
M. ulcerans
M. xenopi
M. simiae
M. malmoense
M. szulgai
M. asiaticum
Rapidly growing mycobacteria
Runyon group IV
M. fortuitum
M. chelonae
M. abscessus
The Staph of mycobacteria
80
Pulmonary Disease M. abscessus Worldwide may
be found concomitant with MAC M. asiaticum
Rarely isolated M. avium complex Worldwide most
common NTM pathogen in U.S. M. celatum
Cross-reactivity with TB-DNA probe M. kansasii
U.S., Europe, South Africa, coal-mining regions
M. chelonae Pulm Disease ?? . M. fortuitum
Associated with aspiration Contaminant M Szulgai
and M Chelonae and Eye disease
81
Lung disease due to NTM occurs commonly in
structural lung disease, such as chronic
obstructive pulmonary disease (COPD), bronchiectas
is, CF, pneumoconiosis, prior TB, pulmonary
alveolar proteinosis, and esophageal motility
disorders Abnormal CF genotypes, CFTR Gene
mutation and _1-antitrypsin (AAT) phenotypes may
predispose some patients to NTM infection NTM
lung disease also occurs in women without clearly
recognized predisposing factors There is also an
association between bronchiectasis,
nodular pulmonary NTM infections and a particular
body habitus, predominantly in postmenopausal
women (e.g., pectus excavatum, scoliosis, mitral
valve prolapse) A mean MAC machine in the thin
and lean Bronchiectasis and NTM
infection, usually MAC, often coexist, making
causality difficult to determine. These patients
may carry multiple MAC strains over time,
suggesting either polyclonal infection or
recurrent infection with distinct strains). It is
unclear whether this problem is due to local
abnormalities (e.g., bronchiectasis) or to immune
defects
Am J Respir CC M 178
1066-1074 , 2008 NHLBI
82
Semi-quantitative analysis of smears can be
useful for diagnostic and post Rx follow up
purposes. The burden of organisms in
clinical material is usually reflected by the
number of organisms seen on microscopic
examination of stained smears.
Environmental contamination, which usually
involves small numbers of organisms, rarely
results in a positive smear examination. Previous
studies have indicated that specimens with a
high number of mycobacteria isolated by culture
are associated with positive smears and,
conversely, specimens with a low number of
mycobacteria isolated by culture are less likely
to have positive smears
83
ATS Recommendations 1. As much material as
possible for NTM culture should be provided with
clear instructions to the laboratory to
culture for mycobacteria (C, III). 2. All
cultures for NTM should include both a rapid
detection broth (liquid) media technique and
solid media cultures (C, III). 3. Quantification
of the number of colonies on plated culture media
should be performed to aid clinical diagnosis
(C,III). 4. Supplemented culture media and
special culture conditions (lower incubation
temperatures) should be used for material
cultured from skin lesions, joints, and bone
(A,II 5. The time (in days) to detection of
mycobacterial growth should be stated on the
laboratory report (C, III).
84
Tumor Necrosis Factor Inhibition NTM IFN-_ and
IL-12 control mycobacteria in large part through
the up-regulation of tumor necrosis factor
(TNF)-_ made predominantly by monocytes/macrophage
s. The risk posed by TNF-_ blocking agents for
predisposing to NTM infections or promoting
progression of active NTM infection is unknown.
Expert opinion is that patients with active NTM
disease should receive TNF-_ blocking agents only
if they are also receiving adequate therapy for
the NTM disease.
85
Pathophysiology of Bronchiectasis related to
mycobacterial disease
- The
inflammation /infection cascade - Interleukin,8, neutrophils, unopposed
elastase and proteases - The effect of trans mural inflammation,
edema, crater formation, ulceration, - Neo vacularization leading to permanent
parenchymal damage - Different properties of sputum in dilated
airways - Variance in mycobacterial genetic pool
- Variance in strains
86
Jeopardy Value
- ? Colonizer
- Indolent disease
- Nodular Disease
- Bronchiectasis
- Fibro cavitary Disease
- MDR disease
- Hypersensitivity
87
- What are the many faces of NTM
- specially MAC ?
88
A 52-year old Caucasian woman sought medical
attention due to chronic cough. Physical exam was
unremarkable. Sputum culture revealed light
growth with few colonies of Mycobacterium avium
complex (MAC). Repeat sputum cultures later again
revealed a few colonies of MAC. The patient was
treated symptomatically and followed clinically
by serial sputum test (s) and radiographic
evaluation. No specific therapy for MAC was
initiated and the patient did well, remaining
asymptomatic.
89
Wheezing Dx Asthma CXR Nodular opacities ? TB
Started RIPE Tr Bx Bx Granulamatous
Inflammation Br Wash MAC
MAC Hot tub Lung or Sarcoidosis with
MAC?
90
Culture positive TB on Rx Subsequent 7 sputa
all culture negative for TB , positive for MAC
Figure 6
91
A 76- year old Caucasian woman, smoker, with
past history of TB, treated completely in the
1960s, was seen with cough and minimal shortness
of breath. Pulmonary function tests revealed
moderate obstructive airways dysfunction. Sputum
tests revealed moderate growth of Mycobacterium
avium complex on repeated examinations. The
patient was placed on daily treatment with
clarithromycin and ethambutol with
bronchodilators. She remained stable on this
regimen without any acute exacerbations. Serial
sputum cultures intermittently revealed light
growth of Mycobacterium avium complex.
92
A 65-year old woman with a history of
nonspecific interstitial pneumonitis (NSIP) and
pulmonary fibrosis and with documented
Mycobacterium avium complex (MAC) on repeated
sputum cultures since 2003 was admitted in March
2006 with increasing dyspnea and respiratory
failure. Prior to admission she had had multiple
sputum cultures which were positive for MAC and
sensitive only to high dose clarithromycin,
ethambutol and rifabutin with which she was
treated for 18 months. Due to concomitant and
repeated growth of methicillin-resistant
Staphylococcus aureus (MRSA), she was also given
linezolid intermittently. She was admitted to
the hospital and treated empirically with
broad-spectrum antibiotics while her MAC
treatment was continued due to persistently
positive sputum cultures. She failed to respond
to therapy and died after a month of
hospitalization due to progressive respiratory
failure.
93
MAN!! The Mycobacterial Highway
TB? RIPE
MK
MAC
MC
A
94
A 42-year old man with history of treated TB in
1980 developed fibrocavitary MAC infection in
1993. His treatment with ethambutol, rifabutin
and clarithromycin was erratic due to
non-adherence. He was admitted to the hospital in
March 2004 with increasing cough, night sweats
and a ten pound weight loss. No culture and
sensitivity data were available. With the history
of erratic treatment, presumed macrolide
resistance and unilateral fibrocavitary right
sided disease, he was evaluated for surgical
excision and pneumonectomy. His pulmonary
function tests revealed a FEV1 of 1.4 L and a
split perfusion pulmonary scan showed one percent
perfusion of the right lung and 99 of blood flow
to the left lung. The patient had a complicated
operative and perioperative course and died of
respiratory failure after a month long stay in
the ICU.
95
A 50-year old man with severe COPD and
bronchiectasis was on long term treatment for
Mycobacterium avium complex pulmonary disease
(MAC-PD) initially and later for
macrolide-resistant MAC (MRMAC). He was admitted
in moderately severe respiratory distress with
fever and increasing cough. In addition to the
multiple drugs used for the treatment of this
patient though the course of his illness,
therapeutic trials of thalidomide, interferon
gamma and high dose mefloquine were given. Due to
progressive bilateral disease and poor pulmonary
function, surgery was not considered. (The
patient later died of respiratory failure and
overwhelming infection).
96
-
ENVIRONMENTAL LUNG DISEASE OUTPATIENT CLINIC -
NON-TUBERCULOUS MYCOBATERIAL DISEASE NTM PROTOCOL - Identify which NTM the patient has
- Check for predisposing factors
- Check environmental factors/ contacts and history
- Check for systemic immune deficiencies
- Check for local structural deficiencies
- Stage the patient based on clinical, radiographic
and bacteriological data. - Staging Mgm plan
- Stage 1 Mild intermittent disease surveillance
and environmental controls - Stage 2 Mild to moderate disease above
measures in addition to emphasizing bronchial
toilet - Stage 3 Moderate disease surveillance,
environmental controls, bronchial toilet plus
oral treatment thrice weekly - Stage 4 Moderate to severe disease
surveillance environmental controls, bronchial
toilet, oral DAILY treatment plus inhaled
antibiotics - Stage 5 Severe disease surveillance,
environmental controls, bronchial toilet, daily
oral customized treatment, inhaled antibiotics
with surgical options always to be kept in mind - Questions we need to ask when considering the
treatment regimen of these patients - What will the benefit of the treatment be to the
patient?
97
- THIS IS THE CORNERSTONE OF DRUG REGIMEN in MAC
Jeopardy Value
98
- WHAT IS A MACROLIDE /AZOLIDE?
99
Isolates of MAC have only a single copy of the
ribosome, and hence, macrolide monotherapy
carries a significant risk of the development of
mutational resistance. All high-level clarithrom
ycin-resistant isolates have mutations in the
adenine at position 2058 or 2059 of the 23S rRNA
gene, which is the presumed macrolide binding
site on the ribosomal unit
100
Suggested algorithm for Culture Sensitivity
Macrolide/Azolide Sensitive
No
Yes Rx with macrolide/Azolide Combination
double or triple Drug Rx
Do Expanded Sensitivity Consider combination Rx
sensitivity Such as Rif /Rb with Eth
101
MANAGEMENT OPTIONS
Step 1 Diagnosis Clinical
Classification
Ref 5. American Thoracic Society
Documents Mycobacterial Diseases Subcommittee.
The Official Statement of the American Thoracic
Society (ATS) and the Infectious Diseases Society
of America (IDSA) Am J Respir Crit Care Med Vol
175. pp 367416, 2007 Ref 9 Chitty S, Ali J.
Mycobacterium Avium Complex Pulmonary Disease in
immune competent patients. Southern Medical
Journal June 2005, 98 (6) pp 646-652
Step 2 CATEGORIZE GROUP
Aggressive treatment group
FOCAL DISEASE DIFFUSE NODULAR
FIBROCAVITARY
COMPLEX
BRONCHIECTASIS
DISEASE
MACROLIDE RESISTANT 3 drugs - SURGERY
3 DRUGS THRICE 3 DRUGS DAILY plus IV
CUSTOMIZED
WEEKLY
AMINOGLYCOSIDE
PROTOCOL
102
Recommendations 1. Surgical resection of limited
(focal) disease in a patient with adequate
cardiopulmonary reserve to withstand partial or
complete lung resection can be successful in
combination with multidrug treatment regimens for
treating MAC lung disease (B, II). 2. Surgical
resection of a solitary pulmonary nodule due
to MAC is considered curative (C, III). 3.
Mycobacterial lung disease surgery should be
performed in centers with expertise in both
medical and surgical management of mycobacterial
diseases (C, III).
103
Factors contributing to the poor response to
therapy included cavitary disease, previous
treatment for MAC lung disease, and a history
of chronic obstructive lung disease or
bronchiectasis and macrolide resistance Helps
establish prognosis, goals and expectations of
therapy
104
Treatment of M. abscessus pulmonary disease.
There are no drug regimens of proven or
predictable efficacy for treatment of M.
abscessus lung disease. Multidrug regimens that
include clarithromycin 1,000 mg/day may cause
symptomatic improvement and disease regression.
Surgical resection of localized disease
combined with multidrug clarithromycin-based
therapy offers the best chance for cure of this
disease.
105
Summary For NTM
- Environmental Surveillance
- Underlying immune or structural lung defect
- Focus on type of clinical-radiologic disease
Bronchiectasis, F/C , Nodular etc - Specific identification of NTM and source search
- Consistent quantification smear/colony count
- Stratification of risk/benefit of Rx
- Goals of Rx and outcomes be established
- Customized approach ( step ladder method ramping
it up )based on tolerance and compliance with
Rx and without compromising overall regimen - Watch drug- drug interaction
- ? role of drug levels?
106
Challenges
- Identification characteristics
- Macrophage barrier to Rx
- Hydrophobicity of MOTT with drugs being
hydrophilic in nature eg more hydrophobic drugs
i.e rifabutin as opposed to rifampin - Cell wall associated permeability barrier
specially seen in M. Chelonei hence ethambutol
specially in combination a better choice - Lack of correlation in vitro and therapeutic
efficacy - Multi strain sero variance specially in AIDS and
patients with nodular / bronchiectasis disease
pattern - Theory of adaptive resistance due to continual
exposure eg pigmentation /proteins when
clofazimine is used
107
Confused ?
So am I , most of the time and if I am not , I
consider myself lucky
108
Thank you , JA