Study Guide - PowerPoint PPT Presentation
1 / 50
Title:
Study Guide
Description:
Study Guide How do hormones regulate adenylyl cyclase activity? PLC activity? Describe the mechanism of regulation of PKA by cAMP Contrast diabetes mellitus type I ... – PowerPoint PPT presentation
Number of Views:101
Avg rating:3.0/5.0
Title: Study Guide
1
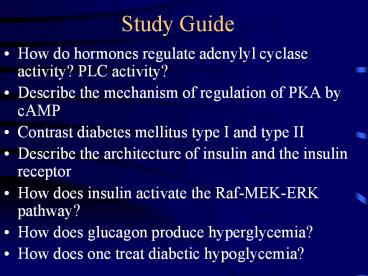
Study Guide
- How do hormones regulate adenylyl cyclase
activity? PLC activity? - Describe the mechanism of regulation of PKA by
cAMP - Contrast diabetes mellitus type I and type II
- Describe the architecture of insulin and the
insulin receptor - How does insulin activate the Raf-MEK-ERK
pathway? - How does glucagon produce hyperglycemia?
- How does one treat diabetic hypoglycemia?
2
How Do Hormones Regulate cAMP levels and PLC
Activity?
- Seven transmembrane segment receptors that
interact with G-proteins - G-protein GTPase activity
- Gs stimulates adenylyl cyclase
- Gi inhibits adenylyl cyclase
- Gq activates phospholipase C (PLC)
- Leads to generation of two messengers
- Diacylglycerol, activates PKC
- Inositol 1,4,5 trisphosphate, releases Ca2 from
intracellular stores in the ER
3
G-Protein Cycle (Fig. 19-10)
4
Regulation of Adenylyl Cyclase (Fig. 19-11)
Gs activates adenylyl cyclase (12) Gi inhibits
adenylyl cyclase
5
Cyclic AMP Metabolism Revisited (Fig. 10-13)
6
How Does Glucagon Lead to an Acute Rise in Blood
Glucose?
- Earl W. Sutherland, Jr. asked how does
epinephrine injection in dog lead to
hyperglycemia? - Epinephrine in dogs uses the beta adrenergic
receptor and the cAMP second messenger system
(Sutherlands system) - Epinephrine in rats, mice, and humans works via
the alpha receptor and not by the cAMP protein
kinase A cascade - In liver, glucagon activates its receptor, Gs,
and adenylyl cyclase to increase cAMP and
activate PKA glucagon in humans works the same
as epinephrine in the dog - This leads to a cascade that activates glycogen
phosphorylase - This leads to the inhibition of glycogen synthase
- Review Daniel Stewarts presentation on 11
February 2004
7
The Protein Kinase Reaction
- ATP protein ? phosphoprotein ADP
- PKA is a serine/threonine kinase
- It is a broad specificity enzyme with many
substrates
8
Fig 10-8 Overview of Glycogen Metabolism
9
Regulation of Glycogen Metabolism (Fig. 10-14)
cAMP activates PKA this illustrates the actions
of PKA
10
Phospholipase C and Inositol (Fig. 19-13)
11
Diabetes Mellitus
- A relative or absolute deficiency of insulin
- Chronic hyperglycemia and disturbances of
carbohydrate, lipid, and protein metabolism - Incidence
- 16 Million Americans aged 20 years and older and
the incidence is increasing - 60-70 patients per thousand dental patients 50
are not diagnosed - Increases with obesity
- Polydipsia, polyphagia, polyuria is the classic
triad understand the mechanisms - Hyperglycemia leads to polyuria as glucose
transport maximum is exceeded - Polyuria leads to polydipsia
- Loss of energy (calories) leads to excessive food
intake, or polyphagia - Type I insulin-dependent, juvenile, immunologic
destruction of the beta cells of the islets of
Langerhans 10 - Type II Adult onset 90
12
Comparison of Type I and II Diabetes Mellitus
Type I Type II
Age of onset lt20 gt30
Ketosis Common Rare
Body weight Non-obese Obese
Prevalence 0.5 5-6
Islet cell antibodies 65-85 lt10
Insulin Rx Necessary Usually not required
Complications Frequent Frequent
13
Metabolic Disorders Associated with Type II
Diabetes
- Hyperglycemia
- Dyslipidemia
- Elevated triglycerides
- Decreased HDL (Good Cholesterol)
14
Diabetes Mellitus Complications
- Retinopathy
- Vision changes
- Most common cause of blindness in the US
- Nephropathy (renal failure)
- Neuropathy
- Sensory, loss of sensation in hands, feet, legs
- Autonomic
- Change in cardiac rate, rhythm, conduction
- Impotence
- Accelerated cardiovascular disease and
atherosclerosis - Peripheral vascular disease (amputations)
- Coronary artery disease
- Stroke
- Hypertension
- Dental complications
- Alterations in wound healing
- Increased incidence of infections
- Xerostomia
- Increased incidence of oral candidiasis
(controversial)
15
Diabetes and Periodontal Health
- Risk factor for prevalence and severity of
gingivitis and periodontitis - Altered host defense secondary to diabetes may
contribute - Increased collagen breakdown owing to increased
collagenase production - Not only does diabetes promote periodontal
disease, but periodontal disease can make the
diabetes more difficult to control (any
inflammatory flare up can increase insulin
requirement) - Possible findings in an undiagnosed diabetic
- Severe, progressive periodontitis
- Enlarged gingiva that bleed easily when
manipulated - Multiple periodontal abscesses
16
Abscesses in Diabetes
17
Periodontitis in Diabetes
18
What do I do with a patient suspected of having
diabetes?
- Ask whether the patient has experienced
polydipsia, polyphagia, polyuria - Probably will be negative, but you have to ask
- This classical triad is associated with type I
diabetes more often than type II diabetes - Symptoms for type II diabetes include lethargy
and fatigue - Recent weight loss (paradoxical in an obese
person) - Family history, i.e., a parent or sibling with
diabetes - Refer to your sister-in-law, the internist
- Diagnosis
- Fasting blood glucose
- Normal lt 110 mg/dL diabetes gt 126 mg/dL
- 2-hour serum glucose after 75 g of glucose PO
- lt140 mg/dL diabetes gt 200 mg/dL
- Hemoglobin A1c
- Normal lt6 diabetes gt7 (usually 10-15)
- Glucosuria this was noted by Dr. Thomas Willis
(of the circle of Willis) - The urine of the diabetic patient.the spirits of
honey
19
Formation of Hb A1c (Fig. 7-5)
20
Insulin
- 51 residues
- Two chains
- 3 Disulfide bonds
- What happens when you remove Asn21?
- Produced in which cells of the pancreas?
- Hyperglycemia ? increased secretion
- First protein to be sequenced Fred Sanger
21
Insulin Receptor Protein-Tyrosine Kinase
- Insulin stimulates glucose uptake in muscle and
fat, glycogen synthesis, lipogenesis, and protein
synthesis, and insulin inhibits lipolysis,
proteolysis, and glycogenolysis - Insulin receptor undergoes autophosphorylation
and phosphorylates IRS1-4 (Insulin receptor
substrates 1-4), PI3 kinase binding protein, and
Shc - Expressed in almost all cells, but at much higher
levels in liver, fat, and muscle - Insulin does not increase glucose transport into
the liver
22
Protein-Tyrosine Kinase (PTK) Cascades
- Initial step represents the activation of a PTK
- The enzyme is not active as a monomer it must
dimerize - There is transphosphorylation A phosphorylates
A, and A phosphorylates A to achieve activation - These phosphotyrosines can function as docking
sites - Attraction of proteins to the docking sites can
be regulatory - The PTK may phosphorylate other proteins that can
serve as docking sites, or they may activate or
inhibit activity
23
Insulin Receptor
- It is a protein-tyrosine kinase
- It autophosphorylates itself and insulin
substrates - The resulting phosphotyrosines serve as docking
proteins that attract Grb2 and Shc - These attract Sos, a GEF, and Ras to start the
signal transduction cascade
24
Insulin Receptor Architecture
- Insulin binds to the N-terminal half of the
a-subunit - Human autoantibodies recognize 450-601
- Y965, Y972 yields sites for PTB (phosphotyrosine
binding) domains that are found in IRS1-4 and Shc - After IRS binds to pY972, it can be
phosphorylated - pY1334 binds SH2 domains of p85 regulatory
subunit of PI3 kinase
25
Ras GTP-Cycle (Fig. 20-3)
- Ras is a GTPase
- It is on one pathway for insulin action
- It is on many other pathways that lead to cell
growth and division - Ras is frequently mutated in cancer (25 of all
human cancers)
26
Grb2, Sos, and Ras
- pY of IRS binds SH2 of Grb2
- SH3 of Grb2 binds to Sos (son of sevenless, a
GEF) - Sos mediates the exchange
27
Ras-Raf-MEK-ERK Overview
- Raf-Mek-ERK is associated with cell growth and
cell division - MEK is a dual specificity kinase
- However, it can lead to apoptosis
- The final result depends upon the conditions, or
context - It is not clearly understood
- SOS GEF
28
Docking Sites and Activation
29
Insulin Receptor and PI3 Kinase
30
The PI-3 Kinase Pathway
- Activated allosterically by binding to
protein-tyrosine phosphate - Catalyzes the phosphorylation of PIP2 to form
PIP3 - PIP3 activates phosphoinositide-dependent protein
kinase (PDK) allosterically - PDK phosphorylates S6K, PKB (AKT), and PKC
- PKB phosphorylates glycogen synthase kinase 3
(GSK3)
31
PI3 Kinase Cascade and Insulin
32
Phosphoprotein Phosphatase-1
- Insulin stimulates glycogenesis in muscle, but
epinephrine stimulates glycogenolysis - Glycogenolyis (breakdown) is associated with
phosphorylation (the cascade) - Glycogenesis (build up) is associated with
dephosphorylation - Insulin promotes the dephosphorylation of
glycogen synthase and phosphorylase - These reactions are catalyzed by the catalytic
subunit of PPase-1 - Insulin leads to the phosphorylation and
activation of PPase-1 - Epinephrine leads to the phosphorylation and
inactivation of PPase-1
33
Phosphoprotein Phosphatase-1 (Fig. 20-5)
34
Diabetes the Glucagon/Insulin Ratio
- Glucagon
- Produced by the alpha cells of the islets of
Langerhans - Early preparations of insulin produced
hyperglycemia followed by hypoglycemia - The hyperglycemic factor represented
contamination - This factor was purified, characterized, and
re-named glucagon - It produces hyperglycemia by at least three
mechanisms - It promotes glycogen breakdown as noted above
- It inhibits glycolysis and increases
gluconeogenesis - cAMP activates PKA, which phosphorylates
fructose-6-phosphate-2-kinase/fructose-2,6-bisphos
phatase - This decreases fructose-2,6-bisphosphate
- This removes a stimulant of glycolysis at the PFK
step - This removes an inhibitor of gluconeogenesis at
the fructose-1,6-bisphosphatase step - PKA promotes transcription of PEP carboxykinase,
an important enzyme in gluconeogenesis - The high ratio of glucagon/insulin action
promotes hyperglycemia
35
Regulation of Fructose 2,6-BP
Fig 7-11
- Glucagon increases cAMP and PKA activity
- PKA increases Frc 2,6 BPase activity and
decreases Frc 2,6 BP - Glycolysis decreased, gluconeogenesis increased
36
Reciprocal Regulation of Glycolysis and
Gluconeogenesis (Fig. 25-2)
37
Insulin Action
- Stimulates glucose transport into muscle, adipose
tissue, and many other cells EXCEPT liver - This results from the recruitment of GLUT4 (of
GLUT1-GLUT7) - Glucose transporters contains 12 transmembrane
segments - Mechanism of recruitment is unclear
- It does not rely on new transporter synthesis
- GLUT4 associated with internal membranes fuses
with the plasma membrane - Insulin promotes glycogen synthesis by inducing
the production of glycogen synthase
38
Glucose Transporter with 12 TM Segments
39
GLUT Recyling
40
Diabetic Hypoglycemia
- One of the five most common dental emergencies
- Usually due to inadequate food intake
- Ask every person receiving insulin whether they
have eaten prior to Rx - If the answer is no, provide food before
providing Rx - Characterized by confusion, agitation, anxiety,
hostility (the previous four can be described as
acting weird), dizziness, tachycardia,
sweating, tremor - Severe loss of consciousness
- Make presumptive Dx of hypoglycemia
- Rx
- If conscious, give 15 g oral carbohydrate 4-6 oz
fruit juice or soda hard candy usually respond
in a few minutes - If unable to take food by mouth, give 50 glucose
IV (LSUHSC SOD) - If unable to take food by mouth, give 1 mg
glucagon sq or im (This is not standard practice
here.)
41
Angiotensin System
- Renin, a proteolytic enzyme, is released from the
juxtaglomerular (JG) cells of the kidney and
converts angiotensinogen to angiotensin I - Angiotensin converting enzyme (ACE) catalyses the
conversion of angiotensin I to angiotensin II - Angiotensin II is a potent vasoconstrictor and
promotes the formation of aldosterone (increases
Na reabsorption)
42
Angiotensin Metabolism
43
ACE Inhibitors
- These compounds decrease peripheral
vasoconstriction and decrease aldosterone
synthesis - This class of drugs are widely used in the Rx of
hypertension
44
Lipophilic First Messengers
45
Lipophilic Hormones
- These hormones can diffuse through plasma and
nuclear membranes - The intracellular receptors , which constitute
the nuclear-receptor superfamily, function as
transcription activators when bound to ligand - Receptor architecture
- C-terminal variable segment
- Middle DNA binding region with a C4 zinc finger
segment - N-terminal hormone (ligand) binding domain
- In some receptors, this domain functions as a
repression domain in the absence of ligand
46
Lipophilic Hormones
- The DNA binding sites, or response elements have
been determined - Inverted repeats bind symmetric receptor
homodimers GRE, ERE - These are found in the cytoplasm in the absence
of ligand bound to Hsp90 (heat shock protein of
MW 90 kDa) - Binding of hormone releases the Hsp and allows
nuclear translocation - After translocation and binding to its HRE, it
activates transcription by interacting with
chromatin-remodeling and histone acetylase
complexes - Direct repeats bind with heterodimers with a
common receptor called RXR VDRE, TRE, RARE - The vitamin D3 response element is bound by the
RXR-VDR heterodimer - Heterodimers are located exclusively in the
nucleus - These repress transcription in the absence of
ligand - They direct histone deacetylation at nearby
nucleosomes - In the liganded state they direct
hyperacetylation
47
Steroid Receptor Superfamily
48
Steroid Hormone Action
49
Hormone Response Elements (HREs)
50
The End
- Biochemistry is fun!!!















![[June 2018]Microsoft 70-779 Study Guide Killtest PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/9087991.th0.jpg?_=20180629044)
![[June 2018]NetApp NS0-159 Study Guide Killtest PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/9087992.th0.jpg?_=20180629045)













