Session Structure - PowerPoint PPT Presentation
Title: Session Structure
1
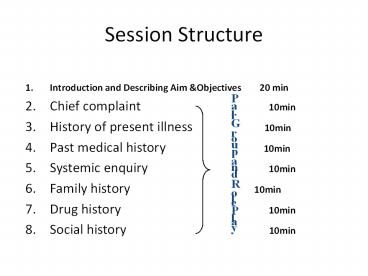
Session Structure
- Introduction and Describing Aim Objectives
20 min - Chief complaint 10min
- History of present illness
10min - Past medical history
10min - Systemic enquiry 10min
- Family history
10min - Drug history 10min
- Social history 10min
Pair Group and Role Play
2
Importance of History Taking
- Obtaining an accurate history is the critical
first step in determining the etiology of a
patient's problem. - A large percentage of the time ) 70), you will
actually be able make a diagnosis based on the
history alone.
3
How to take a history?
- The sense of what constitutes important data will
grow exponentially in future as you learn about
the pathophysiology of disease - You are already in possession of the tools that
will enable you to obtain a good history. - An ability to listen ask common-sense questions
that help define the nature of a particular
problem. - A vast sophisticated fund of knowledge not
needed to successfully interview a patient.
4
General Approach
5
Taking the history Recording
- Always record personal details NASEOMADR.
- Name,
- Age,
- Address,
- Sex,
- Ethnicity
- Occupation,
- Religion,
- Marital status.
- Date of examination
6
Complete History Taking
- Chief complaint
- History of present illness
- Past medical /surgical history
- Systemic review
- Family history
- Drug /blood transfusion history
- Social history
- Gyn/ob history.
7
CHIEF COMPLAINT
8
Chief Complaint
- The main reason push the pt. to seek for visiting
a physician or for help - Usually a single symptoms, occasionally more than
one complaints eg chest pain, palpitation,
shortness of breath, ankle swelling etc - The patient describe the problem in their own
words. - It should be recorded in pts own words.
- What brings your here? How can I help you? What
seems to be the problem?
9
Chief Complaint
- Cheif Complaint (CC)
- Short/specific in one clear sentence
communicating present/major problem/issue. As - Timing fever for last two weeks or since Monday
- Recurrent recurring episode of abdominal
pain/cough - Any major disease important e.g. DM, asthma, HT,
pregnancy, IHD - Note CC should be put in patient language.
10
Duration tips
- Exact duration.
- For how long you are ill.
- When you were completely normal.
- Is this complain for the first time or you have
other episodes.
11
History of Present Illness
- Details progression, regression of the CC
12
History of Present Illness - Tips
- Elaborate on the chief complaint in detail
- Ask relevant associated symptoms
- Have differential diagnosis in mind
- Lead the conversation thoughts
- Decide weight the importance of minor complaints
13
History of Presenting Complaint (HPC)
14
History of Presenting Complaint (HPC)
15
History of Present Illness - Tips
- Avoid medical terminology make use of a
descriptive language that is familiar to them - Ask OPQRSTA for each symptom
16
Pain (OPQRST)
17
Past Medical Illness
18
Past Medical /Surgical History
- Start by asking the patient if they have any
medical problems - IHD/Heart Attack/DM/Asthma/HT/RHD,
TB/Jaundice/Fits E.g. if diabetic- mention time
of diagnosis/current medication/clinic check up - Past surgical/operation history
- E.g. time/place/ what type of operation.
- Note any blood transfusion / blood grouping.
- H/O dental extractions/circumcision any
exessive bleeding during these procedures. - History of trauma/accidents
- E.g. time/place/ and what type of accident
- Any minor operations or procedures including
endoscopies, dental interventions, bipsies.
19
Drug History
20
Drug History
- Drug History (DH)
- Always use generic name or put trade name in
brackets with dosage, timing how long. - Example Ranitidine 150 mg BD PO
- Note do not forget to mention
OCT/Vitamins/Traditional /Herbal medicine
alternative medicine as cupping or cattery or
acupuncture. - Blod transfusion.
21
Drug History
- bd (Bis die) - Twice daily (usually morning and
night) - tds (ter die sumendus)/tid (ter in die) Three
times a day mainly 8 hourly - qds (quarter die sumendus)/qid (quarter in die)
four times daily mainly 6 hourly - Mane/(om omni mane) morning
- Nocte/(on omni nocte) night
- ac (ante cibum) before food
- pc (post cibum) after food
- po (per orum/os) by mouth
- stat statim immediately as initial dose
- Rx (recipe) treat with
22
Family History
- Any familial disease/running in families e.g.
breast cancer, IHD, DM, schizophrenia,
Developmental delay, asthma, albinism. - Infections running in families as TB, Leprosy.
- Cholera, typhoid in case of epidemics.
23
Social History
24
Social History
- Smoking history - amount, duration type.
- A strong risk factor for IHD
- Alcohol history - amount, duration type.
- Occupation, social education background, ADL,
family social support financial situation. - Social class.
- Home conditions as
- Water supply.
- Sanitation status in his home surrounding.
- Animals / birds in his/her house.
25
Social History smoking
- The most important cause of preventable diseases.
- Smoking history - amount, duration type.
- Amount packyear calculations.
- Duration continuous or interrupted.
- Any trials of quitting how many.
- Deep inhalation or superficial.
- Active or passive smoker.
- Type packs, self-made, Cigars, Shesha , chewing
etc.
26
Social History smoking
- Ask the smoker whether he is willing to quit or
not. - Do not forget to encourage the smoker to quit
whenever contacting a smoker as it is proved to
increase quitting rate. - If he is willing to quit, but can not, help him
by NRT, buberpion.
27
Social History alcohol.
- Whether drinking alcohol or not.
- If drinking know whether it is healthy or not.
- Healthy alcohol use
- Men 14 units/week, not gt 4 units/session.
- Women 7 units/week, not gt 2 units/session.
- Dont forget that healthy alcohol use is
associated with less IHD Ischemic CVA. - Unhealthy alcohol use is associated with
cardiomyopathy, CVA, Myopathies, liver cirrhosis
CPNS dysfunction.
28
Social History alcohol.
- Note Do not advice patients or individuals , to
drink for health, because of - Religious cultural reasons.
- Possibility of addiction with its known health
problems.
29
Other Relevant History
- Gyane/Obstetric history if female
- Gravida, para, abortions, SZ sections, antenatal
care screens as for Hep B C.
30
Other Relevant History
- Immunization if small child
- Note Look for the child health card.
- Travel / sexual history if suspected STDs or
infectious disease - Note
- If small child, obtain the history from the care
giver. Make sure talk to right care giver. - If some one does not talk to your language, get
an interpreter(neutral not family friend or
member also familiar with both language). Ask
simple straight question but do not go for yes
or no answer.
31
System Review (SR)
32
System Review
- General
- Weakness
- Fatigue
- Anorexia
- Change of weight
- Fever/chills
- Lumps
- Night sweats
33
System Review
- Cardiovascular
- Chest pain
- Paroxysmal Nocturnal Dyspnoea
- Orthopnoea
- Short Of Breath(SOB)
- Cough/sputum (pinkish/frank blood)
- Swelling of ankle(SOA)
- Palpitations
- Cyanosis
34
System Review
- Gastrointestinal/Alimentary
- Appetite (anorexia/weight change)
- Diet
- Nausea/vomiting
- Regurgitation/heart burn/flatulence
- Difficulty in swallowing
- Abdominal pain/distension
- Change of bowel habit
- Haematemesis, melaena, haematochagia
- Jaundice
35
System Review
- Respiratory System
- Cough(productive/dry)
- Sputum (colour, amount, smell)
- Haemoptysis
- Chest pain
- SOB/Dyspnoea
- Tachypnoea
- Hoarseness
- Wheezing
36
System Review
- Urinary System
- Frequency
- Dysuria
- Urgency/strangury
- Hesitancy
- Terminal dribbling
- Nocturia
- Back/loin pain
- Incontinence
- Character of urinecolor/ amount (polyuria)
timing - Fever
37
System Review
- Nervous System
- Visual/Smell/Taste/Hearing/Speech problem
- Head ache
- Fits/Faints/Black outs/loss of consciousness(LOC)
- Muscle weakness/numbness/paralysis
- Abnormal sensation
- Tremor
- Change of behaviour or psyche.
- Pariesis.
38
System Review
- Genital system
- Pain/ discomfort/ itching
- Discharge
- Unusual bleeding
- Sexual history
- Menstrual history menarche/ LMP/ duration
amount of cycle/ Contraception - Obstetric history Para/ gravida/abortion
39
System Review
- Musculoskeletal System
- Pain muscle, bone, joint
- Swelling
- Weakness/movement
- Deformities
- Gait
40
SOAP