IV Holding Techniques-Neonates and Infants - PowerPoint PPT Presentation
1 / 24
Title:
IV Holding Techniques-Neonates and Infants
Description:
IV Holding Techniques-Neonates and Infants Remember to gather all necessary equipment as well as a second person to hold Equipment includes: 24 gauge insyte IV ... – PowerPoint PPT presentation
Number of Views:187
Avg rating:3.0/5.0
Title: IV Holding Techniques-Neonates and Infants
1
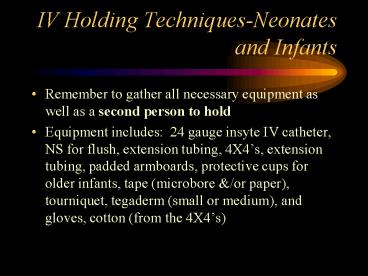
IV Holding Techniques-Neonates and Infants
- Remember to gather all necessary equipment as
well as a second person to hold - Equipment includes 24 gauge insyte IV catheter,
NS for flush, extension tubing, 4X4s, extension
tubing, padded armboards, protective cups for
older infants, tape (microbore /or paper),
tourniquet, tegaderm (small or medium), and
gloves, cotton (from the 4X4s)
2
Appropriate IV Sites
- Extremities (Hicks Gilles, 1999)
- Hands/arms-when choosing hand IV, take into
account which hand is used for finger/thumb
sucking - Feet/legs- make sure that there is adequate
access for heelsticks if applicable - Scalp-for infants 18 months and younger only
contraindicated with infants with hydrocephalus - Important to tell to parents that scalp IVs are
just under the skin and do not go into the brain
or skull, that hair may be shaved also the
advantage of scalp IVs is that they allow their
infant to have full mobility of their hands and
feet (Zaichkin, 2002)
3
Appropriate IV Sites
- Scalp IVs
- all attempts should be made to minimize the
amount of hair to be shaved for IVs-look before
shaving - Save shaved hair for parents-show RCNIC card
- Best places-scalp line along the forehead,
especially in the middle, on the temporal sides,
and behind the ears try to avoid areas near the
eyes - can part hair with alcohol wipes/swabs, water, or
surgilube
4
Armboards
- Can be placed before or after IV insertion,
usually easier after insertion - There are small and regular size padded armboards
used for neonates and preemies - Use as little tape as possible, in some instances
you should use double back tape to secure
extremity - Tape should not cover tips of fingers or toes and
nailbeds should remain exposed - IMPORTANT Have an experienced assistant help you
hold site/extremity/infant securely and keep
infant as calm as possible
5
Other Helpful Tips
- (Hicks Gilles, 1999)
- Warm area by using heel warmer or warm wet cloth
for 10-15 minutes OR turn on radiant warmer if
readily available - Calm infant by swaddling, snuggling, offering
pacifier, playing music, placing toys in view
Also ask parents what their infant likes - Apply tourniquet-can use rubber band-but be aware
of latex precautions when applicable - Hold extremity in dependent position-extremity
should be lower than heart to allow venous
distention - Rub site vigorously with alcohol, but be cautious
with preemies and infants with impaired/compromise
d skin integrity
6
Developmentally Supportive Care
- It is important to watch infants for maladaptive
behaviors. You should allow a rest period
whenever possible between caregiving activities,
including IV starts. Use the infants clinical
status to determine what and how much you do.
This helps to prevent overstimulation. (NANN,
2000)
7
Developmentally Supportive Care
- Touch and Pain (Zaichkin, 2002)
- The sense of touch is the first to develop
- The nerves carrying feeling to and from the
extremities develop during the 5th week of
gestation. - Sensory endings in the skin develop during early
gestation. - As early as 25 weeks, infants have an acute sense
of touch. - Therefore, interventions that provide a positive
sense of touch is extremely important, even in
the most premature of infants.
8
Developmentally Supportive Care
- Touch and Pain-
- Consider the use of Sweet-Ease before beginning
painful procedures such as IV starts and
heelsticks - See RCNIC protocol for use of Sweet-Ease
- Must be ordered by physician or NNP
9
Developmentally Supportive Care
- Swaddling and/or snuggling for containment
- swaddling in blankets or snuggling in a
snuggle-up provides containment - containment helps to (NANN, 2000)
- maintain flexed position for infant, bringing
arms and legs midline, which is similar to the
fetal positions this is an example of
self-consoling behavior - facilitate tucking, which has been shown to
positively help a preterm infants response to
pain - decrease stress during routine procedures
- stabilize infants motor and physiologic
subsystems during stressful manipulations
10
Developmentally Supportive Care
- Containment (continued) helps to
- promote self-regulatory/self-consoling behaviors
such as finger and fist sucking, hand to mouth
maneuvers, leg-bracing (pressing up against a
stable object) and hand clasping (NANN, 2000) - provide boundaries which gives infants a sense of
security because of the womb feeling (Zaichkin,
2002) - Infants prefer boundaries or a nest made of
soft surfaces that yield to their movements
(Zaichkin, 2002)
11
Developmentally Supportive Care
- Other Interventions/Considerations
- Grasping can provide comfort for the
infant-provide objects such as blanket, diaper,
piece of tubing (NANN, 2000) - Light-Dim lighting by shading face during IV
starts-helps to reduce environmental stress and
provide them with womb-déjà vu (dark and muted
environment). (Zaichkin, 2002) - Visual-Provide toys for distraction. Infants
prefer objects high in contrast like black
white bulls eye shape infants also like faces,
like your face or photos (Zaichkin, 2002)
12
Developmentally Supportive Care
- Sound-(Zaichkin, 2002)
- Ears are functionally developed at 27 weeks, but
auditory canal continues to mature after birth
making infants susceptible to noise damage
continuous loud noises can harm infants hearing
and produce physical stress - you can protect hearing during IV starts by
- playing only soft, soothing music
- conversing softly when near infant minimizing
conversations
13
Peripherally Inserted Central Catheters (PICCs)
- Long, soft, flexible catheters inserted through a
peripheral vein (extremities or scalp) designed
to reach one of the larger veins near the heart - They are placed sterilely by specially-trained
RCNIC RNs or CVC RNs - May be done at the bedside or under fluroscopy
- Follow central line protocol
- See Nursing Policy and Procedure III-3.03
Central Venous Catheters for care and maintenance
of PICCs
14
PICCs
- Generally use 1.9 French Neo-PICCs in the RCNIC
15
Central Venous Catheters (CVC)
- A special intravenous catheter placed for
long-term use - Allows a child with chronic conditions who have
need of long term intravenous access to receive
needed fluids, medications, blood products, or
blood draws
16
Central Venous Catheters (CVC)
- Placement of Central Venous Catheters (CVC)
17
Central Venous Catheters (CVC)
- Types of CVCs
- Tunneled- Usually tunneled under the skin on the
chest into a vein near the neck tip of the
catheter is in a large blood vessel near the
heart (superior vena cava)
18
Central Venous Catheters (CVC)
- Types of CVCs
- Non-Tunneled- (Cutdown)-Placed percutaneously
in a major vein such as the subclavian or femoral
veins usually double-lumen Cook catheter used
in the RCNIC
19
Central Venous Catheters (CVC)
- Refer to the following policies and procedures
for care and maintenance and care of CVCs- - Nursing Policy and Procedure III-3.03 for care
and maintenance of CVCs - RCNIC Policy III-2.06-Care of venous and arterial
cutdown in neonates - RCNIC Policy-2.15-Drawing blood from a CVC in the
RCNIC
20
Umbilical Arterial (UAC) and Venous (UVC)
Catheters
- Venous and arterial access that is placed in the
umbilical artery and umbilical vein by the
physician or practitioner - Ideally, catheters must be placed within 24 hours
of delivery - In general, use a 3.5 FR or 5 FR catheter for the
umbilical artery and a 5 FR or 8 FR catheter for
the umbilical vein - May place a double lumen catheter in the
umbilical vein - See RCNIC Policy III 2.05 and III 2.11 for care
and maintenance of UACs and UVCs
21
Umbilical Arterial (UAC) and Venous (UVC)
Catheters
- Proper placement-
- UAC-recommended low placement-tip at L3-L4
- UVC-tip of the catheter should be visible just
above the diaphragm on x-ray - Ideal placement is at the junction of the
inferior vena cava and the right atrium - Uses-
- UAC-continuous blood pressure monitoring, blood
sampling, volume exchanges must be transduced - UVC-provide IV fluids, administer meds, volume
exchanges
22
Umbilical Arterial (UAC) and Venous (UVC)
Catheters
- Available in 3.5, 5, and 8 french catheters
23
Peripheral Arterial Lines
- May be placed in the same manner as a PIV or
placed surgically - Provides blood sampling and continuous blood
pressure monitoring - May also be used in volume exchanges
- Must be transduced
- See RCNIC Policy III-2.06-Care of venous and
arterial cutdown in neonates
24
Resources
- Hicks, K., RN Gilles, A., RN (Revised, 1999).
CHMC orientation module Phlebotomy Skills and
IV insertion. Cincinnati, OH Childrens
Hospital Medical Center. - National Association for Neonatal Nurses (NANN).
(2000). Infant and family-centered developmental
care Guidelines for practice (Document 1201).
Des Plaines, IL Author. - Zaichkin, J., RNC, MN (2002). Newborn intensive
care What every parent needs to know . Santa
Rosa, CA NICU Link.