Stable Angina, Guidelines - PowerPoint PPT Presentation
Title:
Stable Angina, Guidelines
Description:
Title: West Herts Cardiology Author: Dr John Bayliss Description: Blue background, Yellow title, white text, red bullet, Logo Last modified by: Salvatore – PowerPoint PPT presentation
Number of Views:286
Avg rating:3.0/5.0
Title: Stable Angina, Guidelines
1
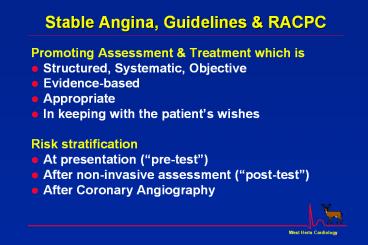
Stable Angina, Guidelines RACPC
- Promoting Assessment Treatment which is
- Structured, Systematic, Objective
- Evidence-based
- Appropriate
- In keeping with the patients wishes
- Risk stratification
- At presentation (pre-test)
- After non-invasive assessment (post-test)
- After Coronary Angiography
2
Angina NSF Standards
- Standard 8
- People with symptoms of angina or suspected
angina should receive appropriate investigation
and treatment to relieve their pain and reduce
their risk of coronary events. - Standard 9
- People with angina that is increasing in
frequency or severity should be referred to a
cardiologist urgently or, for those at greatest
risk, as an emergency. - Standard 10
- NHS Trusts should put in place hospital-wide
systems of care so that patients with suspected
or confirmed coronary heart disease receive
timely and appropriate investigation and
treatment to relieve their symptoms and reduce
their risk of subsequent coronary events.
3
Arterial blood flow
- Blood
- Red cells
- White cells
- Platelets
- Plasma (with O2 Nutrients)
- Clotting factors
- Cholesterol
- Toxins..
- Arterial wall
- Endothelium
- Intima
- Muscular wall
Alt-F4 to close movie Space/ ? ? controls
playback
4
Atherosclerosis Timeline
Foam Cells
Fatty Streak
Intermediate Lesion
Atheroma
Fibrous Plaque
Complicated Lesion / Rupture
From First Decade
From Third Decade
From Fourth Decade
Adapted from Pepine CJ. Am J Cardiol.
199882(suppl 104).
5
Clinical Manifestations of Atherothrombosis
Transient ischemic attack (TIA)
Ischaemic stroke (CVA)
Acute Coronary Syndrome (ACS) Myocardial
infarction (MI)
Angina
AAA Renovascular Disease
Peripheral Vascular Disease (PVD)
6
Angina Prognosis
100
90
Webster 1960-5 Severe CHD Kannel
1949-66 Framingham Men, gt50yrs,
Angina Podrid 1981 ExECG , Mild Angina
Podrid
80
Survival
70
Kannel
Webster
60
2
4
6
8
10
Years of Follow-up
Goldman L et al Am J Cardiol 198351449-52
7
Progression of Vascular Disease
Asymptomatic, or Stable Vascular Disease eg
Stable Angina
Stable AtheromatousPlaque
Unstable Plaque
Complications
- Sudden Death
- ACS
- Myocardial Infarction
- Heart Failure
- Stroke
- etc, etc
Risk Factors
Genetics
8
Majority of MIs are associated with non-flow
limiting, Unstable lesions
Falk et al. Circulation. 199592657-71.
9
Stable Angina in CHD
Narrowing of Coronary artery limits blood supply
to heart muscle
10
Stable Angina Symptoms
"There is a disorder of the breast with strong
and peculiar symptoms considerable for the kind
of danger belonging to it. The seat of it and the
sense of strangling and anxiety with which it is
attended may make it not improperly called angina
pectoris. They who are afflicted with it are
seized while they are walking with a painful and
most disagreeable sensation in the breast ... But
the moment they stand still all this uneasiness
vanishes. If the pain continues, patients
suddenly fall down and perish almost
immediately.
William Heberden London Medical Transactions
1772
11
Effects of Myocardial Ischaemia
Myocardial Ischaemia
TransientLV Dysfunction
ProgressiveLV dysfunction
Angina
Arrhythmia
Breathlessness
Most Myocardial ischaemia is painless (Silent)
.
Sudden Death
12
Causes of Myocardial Ischaemia
Reduced Oxygen Supply
Increased Oxygen Demand
- Coronary AtheroThrombosis
- gradual, progressive ?
- sudden, occlusive ?
- Other causes of ? Coronary flow
- active spasm ?
- lack of vasodilatation ?
- Cold
- Anaemia
- Carbon Monoxide ?
- High Altitude
- Increased Heart Rate
- Exercise, stress
- Smoking ?
- Increased LV stress
- LVH, Hypertension ?
- Aortic Stenosis, HCM
- Cold
- Food
- Hyperthyroidism
? Effects of cigarette smoking
13
Evaluation and Diagnosis
- In patients presenting with chest pain
- detailed symptom history
- focused physical examination
- directed risk-factor assessment
- Estimate the probability of significant CHD
- if intermediate or high refer to RACPC
- Objective assessment (eg ExECG) is for
- Diagnosis of myocardial ischaemia
- Assessment of severity pathophysiology
- Assessment of prognosis
14
Rapid Access Chest Pain Clinics
- One-stop assessment of stable patients
- ? Recent (lt6 months) onset of exertional chest
pain, intermediate-high risk of angina - ? Known CHD which was stable (eg after PTCA or
CABG) now symptomatic again - lt 2 week wait to clinic
15
Classification of Chest Pain
- Estimating the Probability of CHD from History of
Chest Pain - Precipitated by exercise
- Brief duration (lt15 minutes)
- Relieved promptly by rest or GTN
- Central chest location
- Radiates to Jaw, Throat, or L Arm
- Absence of other causes for pain
- CHD
- If only ONE criterion Non Anginal pain lt
30 - If only criteria 4-6 ,or any TWO Chest Pain
? Cause 30-70 - If only criteria 1-3 ,or any FOUR Typical
Angina gt 70
Diamond GA, Forester JS. NEJM 19793001350-8
Patterson RE, et al JACC 1989131653-65
16
Pre-test probability of CHD Duke Score
- By combining
- Classification of Chest Pain
- CHD risk factors (including ECG)
- a more accurate prediction of the (pre-test)
probability of significant CHD can be generated - Structured, systematic, objective assessment
- Easy to use on web, PC or PDA
Pryor DB et al Ann Int Med 199311881-90
17
Pre-test probability of CHD Duke Score
Probability of CHD ? 50
Multiple risk factors Probability of CHD
increased to 88
Pryor DB et al Ann Int Med 199311881-90
18
Pre-test probability of CHD Duke Score
Probability of CHD ? 50
Few risk factors Probability of CHD decreased
to 15
Pryor DB et al Ann Int Med 199311881-90
19
Pre-test probability of CHD Duke Score
- Demonstration of
- web-based RACPC referral form
- automatic risk assessment
- www.westhertshospitals.nhs.uk/whc
- Risk calculators ? RACPC Referral
20
Rapid Access Chest Pain Clinics
- Not every patient with chest pain is suitable
- ? Acute MI / Unstable Angina CCU
- ? Stable Angina with mod-high prob of CHD
- ? Chest Pain ? Cause with mod prob of CHD
- ? Atypical Pain with low prob of CHD ?? OP
- ? ACS / MI, Heart Failure, Valve Disease,
Palpitations - ? Anaemia, AF, Digoxin, LVH, LBBB, cant walk
21
Evidence-based Management of Angina
- Careful assessment
- ? Underlying cause
- ? Risk factors Smoking, Lipids, BP, DM
- ? Prognosis Exercise ECG
- Treatment
- Stop smoking, lose weight, healthy diet
- Aspirin, Statin and ACEI as appropriate for 2y
prevention - ? Blocker if possible (else Verapamil or
Diltiazem) - Nicorandil or Nitrate, using GTN prophylactically
- Consider Angiography ? Revascularisation
22
Effects of Treatment of Stable Angina
23
Stable Angina Guidelines
Gibbons et al JACC 199972092197
24
Stable Angina Guidelines Assessment 1
25
Stable Angina Guidelines Assessment 2
26
Stable Angina Guidelines - Treatment
27
(No Transcript)
28
Prognostic Markers in Exercise Testing
- The Duke Treadmill Score
- exercise time in minutes on Bruce Protocol
- minus 5 x the ST-segment deviation
during or after exercise (mm) - 4 x the angina index 0 if there is no
angina 1 if angina occurs, and
2 if angina is the reason for stopping the
test - works well for both inpatients and outpatients,
and equally well for men and women
Mark DB et al NEJM 1991325849-53Shaw LJ et al
Circulation 1998981622-30
29
Duke Treadmill Score
- Survival According to Risk Groups
- 4 -Year Annual
- Risk Group (Score) Total Survival Mortality
- Low (? 5) 62 99 0.25
- Moderate (-10 to 4) 34 95 1.25
- High (lt -10) 4 79 5.00
Mark DB et al NEJM 1991325849-53Shaw LJ et al
Circulation 1998981622-30
30
Use of Duke Treadmill Score
- Predicted average RecommendedRisk
score annual mortality treatment - low lt1 per year Medical therapy
- intermediate 1 to 3 Cardiac
Catheterization ? Stress imaging - high-risk gt3 per year Cardiac
Catheterization
lt5 pt with low-risk treadmill score will be
identified as high risk after imaging those
with known LV dysfunction should have cardiac
catheterization
Mark DB et al NEJM 1991325849-53Shaw LJ et al
Circulation 1998981622-30
31
Coronary Revascularisation 1
Limiting Angina despite Medical treatment
Recent MIor Unstable Angina
Non-Invasive assessment (eg ExECG) indicates Risk
High Risk
Angiography
Low Risk
Medical treatment
32
Coronary Revascularisation 2
Limiting Angina despite Medical treatment
Recent MIor Unstable Angina
Non-Invasive assessment (eg ExECG) indicates Risk
High Risk
Angiography
Normal or Mild CHD
1-2 vessel CHD
3 vessel CHD or LMS
Low Risk
Medical treatment
PTCA Stent
CABG
MICAS
Balance Risk v Benefit
33
Risk Stratification With Coronary Angiography
- Extent and severity of coronary disease and LV
dysfunction are the most powerful clinical
predictors of long-term outcome - proximal coronary stenoses
- severe left main coronary artery stenosis
- In the CASS registry of medically treated
patients, the 12-year survival rate by - Coronary arteries Ejection fraction
- normal coronary arteries 91 50 to
100 73one-vessel disease 74 35 to
49 54two-vessel disease 59
lt35 21three-vessel disease 40
CASS Circulation 1994902645-57
34
Prognosis of CHD by severity at Angio
100
80
? Distal coronary disease ???1 vessel CHD ???2
vessel CHD ???3 vessel CHD ???Left Mainstem
Stenosis
60
Probability of Survival ()
40
20
0
1
2
3
4
5
Years
Balcon R, Davies S The management of stable
angina RCP1994p61
35
Canadian Cardiovascular Society Classification of
Stable Angina severity
- Class I Ordinary physical activity does not
cause anginaNo angina on ordinary walking or
climbing stairs.Angina with strenuous or rapid
or prolonged exertion at work or recreation. - Class II Slight limitation of ordinary
activityAngina on walking or climbing stairs
rapidly, walking uphill, walking or stair
climbing after meals, in cold, or in wind, or
when under emotional stress, or only during the
few hours after awakening walking more than
100-200m on the level or climbing more than one
flight of stairs at a normal pace and in normal
conditions. - Class III Marked limitation of ordinary physical
activityAngina on walking 100-200m on the level
or climbing one flight of stairs in normal
conditions and at normal pace. - Class IV Inability to carry on any physical
activity without discomfort - Anginal syndrome may be present at rest.
Campeau L. Circulation 197654522523