MENTAL HEALTH INTEGRATION PROJECT - PowerPoint PPT Presentation
Title:
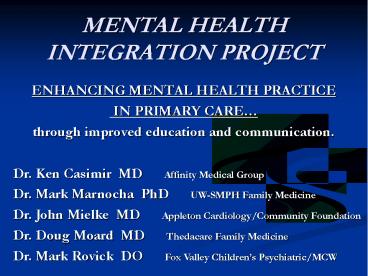
MENTAL HEALTH INTEGRATION PROJECT
Description:
MENTAL HEALTH INTEGRATION PROJECT ENHANCING MENTAL HEALTH PRACTICE IN PRIMARY CARE through improved education and communication. Dr. Ken Casimir MD Affinity ... – PowerPoint PPT presentation
Number of Views:135
Avg rating:3.0/5.0
Title: MENTAL HEALTH INTEGRATION PROJECT
1
MENTAL HEALTH INTEGRATION PROJECT
- ENHANCING MENTAL HEALTH PRACTICE
- IN PRIMARY CARE
- through improved education and communication.
Dr. Ken Casimir MD Affinity Medical
Group Dr. Mark Marnocha PhD UW-SMPH Family
Medicine Dr. John Mielke MD Appleton
Cardiology/Community Foundation Dr. Doug Moard
MD Thedacare Family Medicine Dr. Mark Rovick
DO Fox Valley Childrens Psychiatric/MCW
2
Setting
- Fox Valley region Third largest urban
population area in Wisconsin - Larger Cities Oshkosh, Neenah, Menasha,
Appleton. Green Bay - Smaller Towns Chilton, New London, Shawano,
Hortonvlle, Kimberly, Kaukauna, Little Chute,
Freedom. - Limited Scope contiguous communities, and those
with linkage via health systems x 2. - Region/Community/Practice driven rather than
state-level or discipline-specific.
3
Weaknesses/Threats
- Serious shortage of Pediatric Psychiatry
- Inadequate Adult Psychiatry Access
- Nation-wide shortage of psychiatry
- Strong Family Medicine practices, though majority
not full-scope. (no inpatient medicine or Ob) - Family Medicine forced to assume wider scope of
MH practice.
4
Strengths/Opportunities
- Community interests in compassion, education,
health-care, and youth services. - Community Foundation w/physician voice.
- Connections with MCW and UW-SMPH Medical
residency and consultation programs. - Involved psychiatrists with community, primary
care, and youth expertise. - Community aim to improve MH access, align
pediatric MH resources, and upgrade MH
prevention.
5
Relevant Literature
- Diverse studies of upgrading MH care skills among
primary care physicians. - No clear gold standard as far as methods with
well-documented and replicated results. - Recent statewide initiatives to bolster primary
care MH care skills, notably New York,
Massachusetts, Nebraska. - Pediatric MH concerns increasing, eg, ADHD
overdiagnosis, proper use of atypicals, suicide
prevention, emerging drug use, cyber issues.
6
MHIP Task Force
- 630 am meetings begun in 2011
- Coffee stat and prn
- Prior history of diverse connections among MHIP
group members. - Ongoing alignments with health systems, community
initiatives, educational resources. - Initial literature review.
- Questions about regional needs physician
interest? - Development of mixed Quantitative/ Qualititative
semi-structured interview format.
7
Interview Format
- 11 Likert or other numeric items.
- 5 yes-no or other forced choice items.
- 4 open-ended questions.
- Comments solicited after all items.
- Interview responses transcribed by interviewers.
- Numeric and content summaries by 1st author.
8
Physician Survey InformationMHIP
- 21 semi-structured face-to-face interviews
- 12 female / 9 male regional physicians
- Snowball/Convenience Sample
- MD/DO mix
- Most Early-Middle career (3-20 years post
residency) - 17 Family Medicine, 3 Pediatrics, 1 Internal
Medicine - 8 Affinity 7 Thedacare 2 Kaukauna Clinic 1
each FCCHC, PCA, UW, Independent - From Appleton, Chilton, Greenville, Kaukauna, New
London, Oshkosh, Shawano, Waupaca
9
General Numerical Findings
- 57 do not feel proficient caring for MH
problems. - 67 do not feel counseling is sufficiently
accessible. - Only 29 identify an MD partner w/special
interests in MH care. - Only 20 find MH care reimbursement to be a
problem.
10
Physician Views about MH Changes
- BAD NEWS
More Psychiatrists is most needed change,
but least practical. - GOOD NEWS
More PCP training is 2nd most needed change,
and the most practical. - More Counseling is moderate in need and
practicality. - Reimbursement Change is least needed, and
2nd least practical.
11
Need for MH Changes
- 5 change areas rated from 4 Great Need to 1
Minimal Need
12
Practicality of MH Changes
- 5 change areas rated from 4 Highly to 1
Minimally Practical
13
Physician Interest in MH Training
- 95 indicated they are either Very amenable -
Sign me up or else Interested-Have some
questions. - Only 1 MD (later career) not interested!
- Only 24 (5 Physicians) said they need any
compensation for such training. - EXTENSIVE ideas from physicians for training
content, AND for in-depth group training
face-to-face with primary care peers and
psychiatry / MH resource people.
14
Interview Content Summaries
- Mental Health Care Concerns Lack of
communication w/psychiatry poor access to
general MH resources access to psychiatry
resources unfamiliarity. - Suggested Training Areas Refractory depression
Younger children Bipolar Schizophrenia
Suicide ADHD Managing meds Algorithms for
treatment, diagnosis Listening/counseling.
15
Initial MHIP Conclusions
- Additional psychiatric training is clearly
identified by PCPs as both necessary and
practical - 95 of surveyed PCPs were either interested or
very interested in structured psychiatry CME
training - Only 24 of surveyed PCPs identified a need for
reimbursement for CME time
16
Conclusions (continued)
- PCPs identify their relationships with
psychiatrists as less than satisfactory - Communication regarding available mental health
resources is inadequate - Improvement of MD-MD relationships, along with
readily accessible network re available
resources is essential
17
Current status of project
- Community Funding
- Initial curriculum per ASCP, with augmentation
prn - 9 monthly evening sessions
- Emphasis on complex cases, minimal basic review,
and current evidence/practice updates - 2.5 hours with dinner
- 50 registrants including NPs and
students/residents. Future iterations may
include office staff involved in MH case
management - Session eval forms pretest and posttest
assessment of comfort with aspects of complex OP
MH care.