Evidence-Based Practice - PowerPoint PPT Presentation
1 / 33
Title:
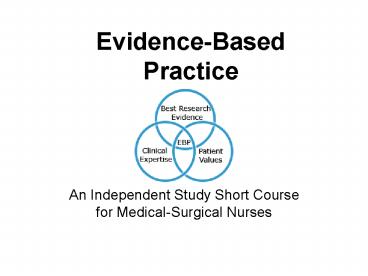
Evidence-Based Practice
Description:
Evidence-Based Practice An Independent Study Short Course for Medical-Surgical Nurses This module was developed by the Clinical Practice Committee of the Academy of ... – PowerPoint PPT presentation
Number of Views:434
Avg rating:3.0/5.0
Title: Evidence-Based Practice
1
Evidence-Based Practice
- An Independent Study Short Course for
Medical-Surgical Nurses
2
- This module was developed by the Clinical
Practice Committee of the Academy of
Medical-Surgical Nurses, - in accordance with
- the 2006-2010 strategic plan.
3
Why is evidence-based practice important and why
now?
- Changing patient demographics require new
approaches to care. - The evidence base for practice is rapidly
expanding and growing in complexity for nursing
and other disciplines.
4
Why is evidence-based practice important and why
now?
- How to search, evaluate, and apply evidence in
practice is unknown by many or inconsistently
used. - There continues to be a mismatch between what we
know to be quality care and the quality of care
that is delivered.
5
Why is evidence-based practice important and why
now?
- Quality problems occur even in the hands of
dedicated, conscientious professionals. - The burden of harm from the underuse, misuse, and
overuse - of care is staggering.
6
Why is evidence-based practice important and why
now?
- The 2003 report by the Institute of Medicine
(Health Professions Education A Bridge to
Quality) recommends that all health care
professionals possess certain skills and
competencies in order to enhance patient care
quality and safety. - All health professionals should be educated to
deliver patient-centered care as members of an
interdisciplinary team, emphasizing
evidence-based practice, quality improvement
approaches, and informatics. - (Institute of Medicine, 2003)
7
Purpose of Module
- To provide an overview of evidence-based practice
(EBP), one of the five competencies that all
health care professionals should possess
(Institute of Medicine, 2003). - Where and how to find the best possible sources
of evidence for your practice. - How to formulate clear clinical questions.
- How to search for relevant answers to the
questions. - Determine when and how to integrate these new
findings into practice.
8
Objectives
- At the end of this module, you will be able to
- Recognize evidence-based practice (EBP) as one of
five core competencies all health professionals
should possess regardless of their title or
discipline (Institute of Medicine, 2003) for
crossing the quality chasm. - Define EBP.
9
Objectives
- Identify two characteristics differentiating
research utilization and EBP in nursing. - List three components of EBP.
- Provide two examples of how EBP benefits the
nurse. - Provide two examples of how EBP benefits the
patient.
10
Objectives
- Describe the 5 steps of the EBP process.
- Write a researchable clinical question.
- Identify resources for developing relevant
answers to the question. - Use clinical judgment and the 5-step process for
determining when and how to integrate findings
into practice.
11
Evidence-Based Practice
- is
- Knowing that what we do is the best practice.
12
How do we know in nursing?
- Tradition
- Authority
- Borrowing
- Trial and error
- Personal experience
- Role modeling and mentorship
- Intuition and reasoning
- Nursing research
13
Nursing Research
- Diligent, systematic inquiry to validate and
refine existing knowledge and generate new
knowledge that directly and indirectly influences
nursing practice. (Burns Grove, 2004)
14
Types of Nursing Research
- Describe
- Identify and understand phenomena, issues
- Explain
- Clarify relationships
- Predict
- Estimate the probability of outcome
- Control
- Manipulate the situation to get desired outcomes
15
- Much of what is known from research has not been
applied in practice. - This is known as
Research-Practice Gap
16
Research-Practice Gap
- During the 1980s and 1990s, nursing emphasized
bridging this research-practice gap through the
development of research utilization (RU)
projects.
17
Research-Practice Gap
- Steps of the process included
- Dissemination of knowledge.
- Synthesis of findings.
- Critique of studies.
- Application of findings.
- Development of research-based practice guidelines
(i.e., Agency for Health Care Policy and
Research/AHCPR practice guidelines Conduct and
Utilization of Research in Nursing/CURN practice
protocols).
18
Research-Practice Gap
- Even though guidelines and knowledge have been
disseminated, the overall effect on clinical
practice and patient outcomes is unclear.
19
Research-Practice Gap
- The problems of importance to medical-surgical
nursing (skin breakdown, pain, bowel function,
treatment adherence, nausea) and related
interventions are largely not collected in
medical record databases. - Nursing research studies are predominately
descriptive or qualitative in design, rather than
what is considered more rigorous and
quantitative.
20
EBP is
- Needed to help bridge the research-practice gap
by - Strengthening the evidence base so that we know
what works and what doesnt work in providing
patients with the best outcomes. - Standardizing evidence across fields to reach the
best outcome for the patient. - Housing evidence in online databases providing
reviews of the evidence base. - Translating and consolidating state of the
science into clinical recommendations. - (Stevens, 2004)
21
EBP is
- Conscientious, explicit, and judicious use of
theory-driven, research-based information in
making decisions about care delivery to
individuals or a group of patients, and in
consideration of individual needs and preferences
(Ingersoll, 2000).
22
EBP is
- Integration of best research evidence, clinical
expertise, and patient values in making decisions
about the care of individual patients (Institute
of Medicine, 2001).
23
Key Components of EBP
- Decisions about care are based on
- A. Research evidence.
- B. Clinical expertise, judicious use.
- C. Patient values and circumstances.
- (Institute of Medicine, 2003)
24
A. Research Evidence
- Randomized controlled trials
- Laboratory experiments
- Clinical trials
- Epidemiological research
- Outcomes research
- Qualitative research
- Expert practice knowledge, inductive reasoning
25
B. Clinical Expertise
- Knowledge gained from practice over time
- Inductive reasoning
26
C. Patient Values, Circumstances
- Unique preferences
- Concerns
- Expectations
- Financial resources
- Social supports
27
Benefits for Med-Surg Nurses
- Fewer Errors Reduced likelihood of making type
1 and type 2 errors in practice - Type 1 Acceptance of a practice that is
incorrect. Example Administration of a wrong
dose, using the wrong procedure, teaching
patients using the wrong information. - Type 2 Rejection of a practice that is correct.
Example Failing to screen patients for fall or
pressure ulcer risks failing to wash hands
before and after patient contact failing to
provide patients with smoking cessation
information. - (Aherns, 2005)
28
Benefits for Med-Surg Nurses
- Greater professional satisfaction from working
as part of a team and experiencing effective
practice.
29
Benefits for Med-Surg Nurses
- Better Care
- Less variation in care among caregivers where
knowledge for improvement is already available. - More predictable health outcomes.
- Less waste and inefficiency yielding fewer delays
in diagnosis and treatment and fewer
complications.
30
EBP Process
- There are 5 steps in judging the evidence and
determining the circumstances and patient values
for guiding application.
31
EBP Process
The EBP Process Steps are
- Assess practice (formulate question)
- What isnt working?
- What do you want to know about?
- Decide (evidence review)
- What resources are available and are they any
good? - What has worked in other places?
- How can you change your practice?
- Plan (develop a plan based on findings)
- Make a plan to change care based on relevant,
applicable information. - Let others help.
- Intervene (take action to review process or
change) - Implement revised caregiving protocol in
clinical unit. - Evaluate (care improved or modify and again
intervene) - How well is that working for you?
32
References
- Aherns, T. (2005). Evidence-based practice
Priorities and implementation strategies. AACN
Clinical Issues. 16(1), 36-42. - Burns, N. Grove, S. K. (2004) The Practice of
Nursing Research Conduct, Critique
Utilization, 2-3. - Fineout-Overholt, E., Melnyk, B.M., Schultz, A.
(2005). Transforming health care from the inside
out Advancing evidence-based practice in the
21st century. Journal of Professional Nursing,
21(6), 335-344. - French, B. (2005). Evaluating research for use in
practice what criteria do specialist nurses use?
Journal of Advanced Nursing, 50(3), 235-43 - Ingersoll, G. I. (2000). Evidence-based Nursing
What it is and what it isnt, Nursing Outlook,
48, 151-152 - Institute of Medicine,(US) Committee on Quality
Healthcare in America (2001). Crossing the
quality chasm A new health system for the 21st
Century, The National Academies Press, 145-163 - Institute of Medicine, (US)Greiner, A. Knebel,
E., (Eds.) (2003) Health Professions Education A
bridge to quality, The National Academies Press,
45-74 - Ledbetter, C. A, Stevens, K.R. (2000). Basics
of Evidence-Base Practice, Seminars in
Perioperative Nursing 9 (3) 91-97 - National Patient Safety Goals. (2006). The Joint
Commission (formerly JCAHO) - Stevens, K. R. (2004). ACE Star Model of EBP
Knowledge Transformation. Academic Center for
Evidence-based Practice. The University of Texas
Health Science Center at San Antonio.
www.acestar.uthscsa.edu
33
Additional Readings
- Cullen, L., Greiner, J., Greiner, J., Bombei, C.,
Comried, L. (2005). Excellence in
evidence-based practice Organizational and unit
exemplars. Critical Care Nursing Clinics of
North America, 17, 127-142. - Greiner, A., Knebel, E., (Eds.). (2003). Health
professions education A bridge to quality.
Washington, DC The National Academies Press. - Stevens, K.R., Staley, J.M. (2006). The
Quality Chasm reports, evidence-based practice,
and nursings response to improve healthcare.
Nursing Outlook, 54(2), 94-101. - Titler, M., Kleiber, C., Steelman, V., Goode, C.,
Rakel, B., Barry-Wlker, J., et. al. (1994).
Infusing research into practice to promote
quality care. Nursing Research, 43, 307-313. - Titler, M., Kleiber, C., Steelman, V., Rakel, B.,
Budreau, G., Everett, L., et. al. (2001). The
Iowa Model of evidence-based practice to promote
quality care. Critical Care Nursing Clinics of
North America, 13(4), 497-509.