From Hospital to Home - PowerPoint PPT Presentation
1 / 16
Title:
From Hospital to Home
Description:
Discharge Planning Empowering Older Adult towards improved self-care. ... (Complete checklist make referral if appropriate within 24 hours) ... – PowerPoint PPT presentation
Number of Views:146
Avg rating:3.0/5.0
Title: From Hospital to Home
1
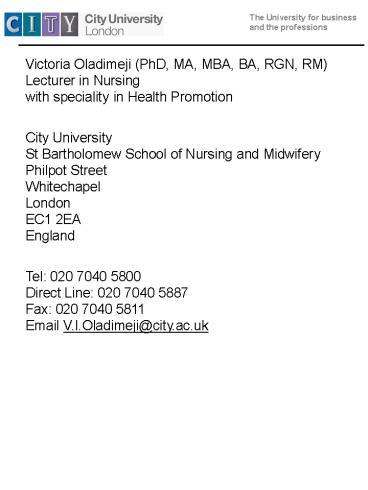
Victoria Oladimeji (PhD, MA, MBA, BA, RGN,
RM)Lecturer in Nursing with speciality in
Health Promotion City UniversitySt Bartholomew
School of Nursing and MidwiferyPhilpot
StreetWhitechapelLondonEC1 2EAEngland Tel
020 7040 5800Direct Line 020 7040 5887Fax 020
7040 5811Email V.I.Oladimeji_at_city.ac.uk
2
Discharge Planning Empowering Older Adult
towards improved self-care.
Introduction Every year more than five million
people in Britain experience life as hospital
in-patients (Chiva and Stears 2001Henwood 2004)
For the vast majority of these people the
episode will be relatively straightforward.
However, the discharge process and outcomes are
not always positive.
3
Admission to and discharge from hospital can be a
distressing time for individuals, their families
and friends. For most people, however,
treatment will be successful and they will return
to their usual way of life very quickly through
the provision of an accurate diagnosis, treatment
and rehabilitative service.
4
Some people will need additional help to enable
them to do so over and above their medical
treatment. These needs can be many and varied and
cannot be met by the NHSalone.
5
Aim of study
- To review current practices in discharge
planning in hospital settings and to critically
evaluate some of the government strategies for
improving the discharge process and the
transition from hospital to home for older adults.
6
Global View
- Studies suggest patients journey from hospital
to the community is not always a smooth
transition. - Grimmer and Moss (2000) (Australia) Magilvy and
Congdon (2000) (USA). - Grimmer and Moss found that community services in
the first week post-discharge was low suggesting
that carers and patients carried the majority of
the burden immediately after discharge. This is
consistent with most of the studies done in UK
(Waters et al 2001)
7
The key principles underpinning effective
discharge and transfer of care policy are
- The avoidance of unnecessary hospital admission,
good clinical outcomes and effective discharge
planning is facilitated by a whole system
approach to the commissioning and delivery of
services. - Characteristics of whole system working?
- Responsive ,, clear vision, no gaps in services,
Partnerships enhanced. Organisations should work
proactively, and together to review and improve
performance and find solutions. (DOH 2003)
8
Figure 1. A virtuous circle of services.
Source Audit Commission (2002).
9
Aims of Good Discharge PracticeLocal Policy
- Maintaining a safe home environment Physical,
Social, Psychosocial - Maximising Independence
- Preventing Readmission
- Planning and and coordination of services and
resources. - (Discharge policy statement 1999)
10
Discharge Planning Process
Assess Evaluate Plan Implement
11
Flow Chart of Assessment Process
Admitting nurse Checklist, referral (within 24
hours). Social Work Response (within 2 working
days)Various Assessments (Single Assessment to
avoid duplication).Contact with Local Community
Services.Provision of Care Plan (within 7
working days).Referral to all Local Community
Services.
12
Flow chart of Assessment Process in an NHA
hospital in England
- Admitting Nurse
- (Complete checklist make referral if
appropriate within 24 hours) - ?
- Social Work Response (within 2 working days)
- ?
- Complex Assessment
- (Multidisciplinary, multi-agency specialist
- assessments, involving medical, OT, physio, etc)
- ?Contact with Local Community Services
- (for simple social care needs)
- ?
- Provisional Care Plan Development (within 7
working days)Case ConferenceMultidisciplinary
with clients and carers and representatives from
purchasing in Social Services - Referral to all local Community Services, e.g.
Social Services, District Nurses, Health
Authority etc
13
Intermediate Care
- Intermediate Care was heavily emphasised in the
National Service Framework (NSF) for older people
(DOH 2001).According to the DOH, - Intermediate care should meet these four
criteria - Targeted at people who would otherwise face
unnecessary long hospital/residential/ stays. - Services provided should be based on thorough
assessment (single assessment framework with one
set of professional records and shared ways of
working). - Planning should maximise independence.
- Services should be time - orientated- maximum 6
weeks, minimum 1-2 weeks.
14
The emphasis lies on the need to provide
integrated services to promote faster recovery
from illness, prevent unnecessary acute hospital
admission, support timely discharge and maximise
independence.
15
Conclusion
- Transition from hospital to home should
involve - Minimum stress
- Careful assessment, planning, implementation
and evaluation with full involvement of patients
and carers/relatives and particular with - attention to vulnerable patient.
- A collaborative, and well coordinated approach
with multiple professional/agencies approach. - More intermediate care beds in line with the NSF
- Education and training for nurses in Health
promotion and advocacy.
16
References
- . Audit Commission (2002) Integrating services
for older people. London The Stationery Office. - Audit Commission (2000) The way to go home.
Oxford Audit Commission Chiva A. and Stears D.
(2001) Promoting the Health of Older People.
Buckingham, Open University. - DOH (2001) National Service Framework for Older
Adults. London HMSO - DOH (2003) Discharge Handbook. London HMSO.
- Grimmer K. Hedges G. Moss J. Staff perceptions
of discharge planning a challenge for quality
improvement. Journal Article, Tables/Charts
Australian Health Review. 1999 22(3) 95-109.
(18 ref) - Henwood M. (2004) Hospital Discharge
Integrating Health and Social Care Health and
Social Care in the Community. London HMSO. - Magilvy J. and Congdon J (2000) . The Crisis
Nature of Health Care Transitions for rural Older
Adults Public Health Nursing Vol. 17(5)Sept.
Oct. - Tower Hamlets PCT 2004 Discharge policy
statement - Waters K. (2001) Sources of support for older
people after discharge from hospital 10 years
on, Journal of Advanced Nursing Vol 33 (5) March.