EPILEPSY - PowerPoint PPT Presentation
1 / 34
Title:
EPILEPSY
Description:
EPILEPSY &THE DENTAL PATIENT Manifestations of Seizure Attack: Isolated, brief seizure - Tonic-clonic movement of trunk & extremities - Loss of consciousness ... – PowerPoint PPT presentation
Number of Views:270
Avg rating:3.0/5.0
Title: EPILEPSY
1
EPILEPSY THEDENTAL PATIENT
2
Manifestations of Seizure Attack
- Isolated, brief seizure
- - Tonic-clonic movement of trunk
extremities - - Loss of consciousness
- - Vomiting
- - Airway obstruction
- - Loss of urinary anal sphincter control
- Epilepsy Recurrent seizures attacks
- Repeated or sustained seizure (Status Epileptics)
3
Seizure vs Epilepsy
Seizures
Nonepileptic
Epilepsy (Recurrent Seizures)
Cardiovascular Drug related Syncope Metabolic
(glucose, Na, Ca, Mg) Toxic (drugs,
poisons) Infectious Febrile convulsions Pseudoseiz
ure Alcohol/drug withdrawal Psychiatric
disorders Sleep disorders (cataplexy)
Idiopathic (primary)
Symptomatic (secondary)
4
Epilepsy
- Definition a state of recurrent seizures, not
due to an identifiable metabolic cause - May be due to
- Underlying genetic or congenital factors
- Cerebral insult prenatally or later in life
- Background
- 1 2 of the general population has seizures
- Primary
- Idiopathic epilepsy onset ages 10-20
- Secondary
- Precipitated by one of the following
- Intracranial pathology
- Trauma, Mass, Abscess, Infarct
- Extracranial Pathology
- Toxic, metabolic, hypertensive, eclampsia
5
Causes of Epilepsy
6
Seizure Types
- Generalized Convulsive Seizures (Grand Mal)
- Tonic , clonic movements, () LOC, apnea,
incontinence and a post ictal state - Non Convulsive Seizures (Petit Mal)
- Brief lapse of consciousness that may last only a
few seconds. - Absence seizures blank staring spells
- Myoclonic brief contractions of selected muscle
groups - Partial Seizures
- Characterized by presence of hallucinations
- Simple somatic complaints no LOC
- Complex somatic complaints AMS or LOC
7
Types of Epilepsy
8
Epilepsy Precipitants
- What might cause an otherwise stable patient to
have a seizure? - Forgetting to take anticonvulsant
- Stress Emotional/Physical
- Sleep disturbance
- Hypoglycaemia
- Alcohol withdrawal
- Other medications
- Anticonvulsants withdrawal from esp.
benzodiazepines - Antidepressants
- Antipsychotics
- Antihistamines
- Antibiotics
- CNS stimulants
- Theophylline, caffeine, cocaine, amphetamine
- Nonsteroidal anti-inflammatory agents
- Opiates
9
Epilepsy Potential problems
- Precipitation of the attack.
- Problems of drugs taken
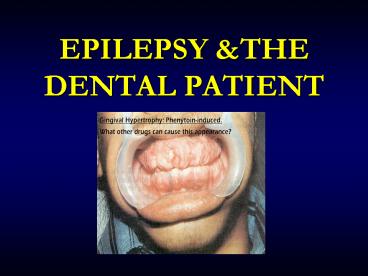
- Phenytoin------- Gingival hyperplasia
- Valproate------- Bleeding tendancy
- Most epileptic seizures are self-limited .
- If more than 1 seizureconsider the possibility
of underlying abnormalitye.g. electrolyte
disturbance, hypoglycaemia - Status Epilepticus Seizures that are
prolongedi.e. longer than 10 minutes or that
re-occur without the patient regaining normal
consciousness
10
Approach for Seizure
- Turn person on side with face turned toward
ground to keep airway clear, protect from nearby
hazards - DO NOT put any object in mouth or restrain
- As always ABCs First
- IV, O2, Monitor.
- Send blood for CBC, Chemistry, Tox screen as
appropriate - Anticonvulsant levels
- Prolactin levels / Lactate levels
- For seizures that are prolongedi.e. longer than
5 minutes or that re-occur without the patient
regaining normal consciousness Rx with
Lorazepam - Is patient still seizing? Post ictal?
Pseudoseizure? - Complete History and Physical Exam
- Including detailed Neuro Examination
- Repeat Neuro evaluations a must!
- Transfer to hospital needed for
- Multiple seizures or status epilepticus
- Person is pregnant, injured, diabetic
- New onset seizures
11
Medical Treatment of First Seizure(s)
- Whether to treat first seizure is controversial ?
- 16-62 will recur within 5 years
- Relapse rate for second seizure is reduced by
AEDs, - BUT long term prognosis of whether the patient
will have refractory epilepsy is not - Increased risk of relapse
- Abnormal imaging
- Abnormal neurological exam
- Abnormal EEG
- Family history of epilepsy
- Currently, most patients are not treated for the
first seizure unless there is an increased risk
for relapse
12
ANTIEPILEPTIC DRUGS
2nd Generation
1st Generation
- Gabapentin
- Lamotrigine
- Topiramate
- Tiagabine
- Oxcarbazepine
- Levetiracetam
- Zonisamide
- Pregabalin
- Phenytoin
- Carbamazepine
- Sodium Valproate
- Phenobarbital
- Primidone
13
After seizure attack
Patient Unconscious
Patient Conscious
- Place on side and suction airway
- Monitor vital signs
- Initiate BLS
- Administer O2
- Prepare to ER
- Suction airway
- Monitor vital signs
- Administer O2
- OBSERVE for at least 1hr and consult physician
If sustained
- Diazepam 5mg/min IV
- Midazolam 3mg/min IV or IM
- Phenytoin1015mg/kg IV
14
Dental treatment of the Epileptic patients AEDs
2. Adequate history -Nature of seizure
-Seizure control -Medication compliance
1. Patient handling -Chair position
-Patients head -False teeth
3. Treatment planning -Stressful situation
-Photic stimulation -Hypoglycemia
4. Education - dental staff
15
Prevention of Peri-operative Seizures
- Patients must take their anticonvulsant
medication - If general anaesthetic anaesthetist should be
aware of seizure tendency - Check patients pre-operative anticonvulsant
levels - Consult with patients neurologist or family
physician - Most stable epileptics, well-controlled on
medication, can undergo surgery without
difficulty or complication
16
Dental practice AED
1. Unexplained oral manifestations eg. mucosal
bleeding, sore tongue or mouth, ulcerations in
the mouth, Blood dyscrasias aplastic
anemia, Agranulocytosis, Thrmbocytopenia
17
Valproate Lamotrigine
18
Status Epilepticus
- ? Definition
- Operationally defined as seizure lasting greater
than 5-10 minutes OR two seizures between which
there is incomplete recovery of consciousness. - Recurrent seizures with failure to recover from
one seizure before next seizure begins
19
Status Epilepticus
- ? A medical emergency
- Adverse consequences can include hypoxia,
hypotension, acidosis and hyperthermia - Goal stop seizures as soon as possible
- Hypertension (early)
- Arrhythmias
- Neurogenic
- Hypotension (late)
- Aspiration
- Injury, burns etc
- Hypoxia
- Lactic acidosis
- Hypercarbia
- Rhabdomyolysis
- Hyperpyrexia
- Hypoglycaemia
20
Aetiology
- Tumour
- Cerebrovascular disease
- Head injury
- Infection
- Hypoxic encephalopathy
- Drug abuse / overdose / withdrawal
- Metabolic
- Primary epilepsy
- Pseudoepilepsy
21
Treatment
- ABC oxygen IV access
- Glucose if indicated or unsure (50mls/D50
- Diazepam or lorazepam IV (or PR)
- Phenytoin (to terminate SE or prevent further
fits) - Monitor ECG and BP
- Investigate monitor (EEG)
- Persistent
- gt Further phenytoin
- gt Phenobarbitone
- gt Thiopentone
- Propofol
22
Prognosis
- Depends on
- Aetiology
- Age
- Duration of status
- Systemic complications (anoxia)
- Treatment given
- Mortality 3 35
23
- Responding to a Patient Experiencing a Convulsion
24
After seizure attack
Patient unconscious
Patient conscious
- Place on side and suction airway
- Monitor vital signs
- Initiate BLS
- Administer O2
- Prepare to ER
- Suction airway
- Monitor vital signs
- Administer O2
- OBS for at least 1hr and consult physician
If sustained
- Diazepam 5mg/min IV
- Dormicum 3mg/min IV or IM
- Dialantin 1015mg/kg IV
25
Seizures vs Epilepsy
Seizures Epilepsy
- Definition the clinical manifestation of an
abnormal and excessive excitation of a population
of cortical neurons - Incidence approximately 80/100,000 per year
- Lifetime prevalence 9 (1/3 benign febrile
convulsions)
Definition a tendency toward recurrent seizures
unprovoked by systemic or neurologic
insults Incidence approximately 45/100,000 per
year Point prevalence
0.5-1 14 years or younger 13 15 to 64
years 63 65 years and older 24
Cumulative risk of epilepsy through 74 years
old 1.3 - 3.1
26
STROKE and TIA
- Cerebrovascular disease is the most common cause
of neurologic disability in Western countries - Major types of cerebrovascular disease
- Cerebral insufficiency
- Infarction
- Haemorrhage
- Arteriovenous malformation
- Stroke Ischaemic lesions
- TIA transient ischaemic attack
- Focal neurologic abnormalities of sudden onset
and brief duration (usually minutes, never more
than a few hours) that reflect dysfunction in the
distribution of either the internal
carotid-middle cerebral or the vertebral-basilar
arterial system
27
Stroke
- 80 involve the carotid system
- 3rd leading cause of death in US and Canada
- Major cause of disability
- Most stroke survivors die of myocardial disease
28
Stroke Unmodifiable Risks
- Age majority occur in individuals gt65
- Male gender
- Race higher incidence in African Americans
- Heredity
29
Stroke Modifiable Risks
- Hypertension
- Diabetes mellitus
- Cigarette smoking
- Alcohol
- Obesity
- Hyperlipidaemia
- Cardiac disease esp. previous myocardial
infarction and atrial fibrillation - Haematologic factors e.g. hyperhomocystinaemia
30
Treatment of Acute Stroke
- In a non-post-operative patient, tPA (tissue
plasminogen activator) can be given intravenously
within 3 hours of onset of stroke symptoms and
intra-arterially within 6 hours - The best treatment is prevention
31
Stroke Prevention
- Risk factor modification
- Aspirin
- Dose between 81 and 325 mg/day
- Ticlopidine (Ticlid)
- Clopidogrel (Plavix)
- ASA/persantine (Aggrenox)
- Warfarin
32
Stroke and Surgery
- For elective surgery delay for 2-3 months
post-event - Do not stop ASA or antiplatelet agent
- Remember high incidence of ischaemic coronary
artery disease in patients with TIA or stroke - Surgical trauma associated catecholamine release
leads to platelet activation - Platelet activation promotes platelet aggregation
and hypercoagulability - Aspirin is not routinely started in the immediate
peri-operative period - Even in high risk patients already taking
aspirin, it is generally discontinued a week
prior to elective surgery to improve
intra-operative hemostasis
33
Stroke and Surgery
- The risk-to-benefit ratios of administering vs
withholding aspirin in the immediate
peri-operative period have never been assessed
and compared - There are no large randomized controlled trials
available to guide us - WHAT DOES THE LITERATURE SAY?
- Gaspar et al. Department of Oral and
Maxillofacial Surgery, Rambam Medical Center,
Haifa - CONCLUSION discontinuing low-dose aspirin prior
to elective oral surgery is not justified - Harefuah 1999 136108-10
- Sonksen et al. Dept. of Anaesthesia, City
Hospital, Birmingham, UK - Conclusion in healthy volunteers the defect in
haemostasis has largely disappeared 48 hours
after the last dose - British Journal of Anaesthesia 1999 82360-5
34
Aspirin and Surgery
- Bartlett Department of Plastic, Reconstructive,
Hand and Maxillofacial Surgery, Middlemore
Hospital, Auckland, New Zeland - Conclusion it is unnecessary to stop aspirin
before minor dermatologic plastic surgery - British Journal of Plastic Surgery 1999 52214-6
- Ardekian et al. Department of Oral and
Maxillofacial Surgery, Rambam Medical Center,
Haifa, Israel - Conclusion low-dose aspirin should not be
stopped before oral surgery - Journal of the American Dental Association 2000
131 1398, 1401-2