Hands of patient with Rheumatoid Arthritis at autopsy - PowerPoint PPT Presentation
1 / 97
Title:
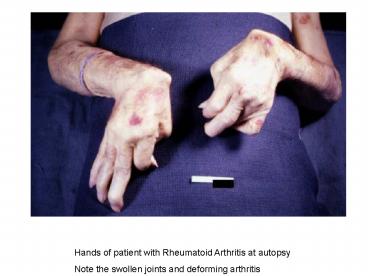
Hands of patient with Rheumatoid Arthritis at autopsy
Description:
... with Amyloid Demonstrates the cells that make up the tissue: resemble plasma cells and are the malignant cell of multiple myeloma Vertebral column at autopsy 1: ... – PowerPoint PPT presentation
Number of Views:113
Avg rating:3.0/5.0
Title: Hands of patient with Rheumatoid Arthritis at autopsy
1
Hands of patient with Rheumatoid Arthritis at
autopsy Note the swollen joints and deforming
arthritis
2
Joint capsule surrounding metacarpal joints of
patient with Rheumatoid Arthritis Note the
thickening of the capsule and the focal
accumulation of inflammatory cells surrounding a
central area of fibrinoid necrosis (arrow)
3
Joint capsule with another granuloma surrounding
a central area of fibrinoid necrosis (arrow)
4
Foot of same RA patient Note the subcutaneous
nodule on the medial aspect of the foot (arrow)
5
Micrograph of the subcutaneous nodule from this
RA patient
6
Subcutaneous nodule from RA patient Granulomatous
lesion with a necrotic center and a peripheral
rim of macrophages, fibroblasts, and occasional
lymphocytes. In the necrotic center of the
granuloma there is some mineralization
(basophilic material).
7
Subcutaneous nodule Demonstrates necrotic center
and peripheral rim of macrophages, fibroblasts,
and occasional lymphocytes. There are focal
accumulations of hyaline material (fibrinoid
material) within the granuloma.
8
Illustrates the palisading nuclei of the
monocytes which are located at the periphery of
the central necrotic region (1)
9
Mononuclear cells surrounding the central
necrotic area The focal accumulations of
fibrinoid material are clearly visible.
Lymphocytes are present in the extreme right.
10
Another region with macrophages (right),
fibrocytes (left), and occasional lymphocytes
throughout the lesion
11
Thyroid gland from patient with Graves Disease.
Note the gland is enlarged and dark red. A
normal thyroid weighs 25 g, this one weighed 45 g.
12
Thyroid gland from patient with Graves Very
cellular and very little colloid
13
Thyroid gland from patient with Graves Note the
cellularity of the tissue with marked infolding
of the epithelial tissue.
14
Thyroid gland from patient with nodular goiter
15
Closer view of cut surface of thyroid from
patient with nodular goiter Note the multilobular
appearance of the tissue.
16
Thyroid gland of patient with Hashimotos
Thyroiditis, picture taken at autopsy Only
slightly enlarged, very firm texture
17
Thyroid gland from this case More cellular than
expected. There does not appear to be normal
colloid-filled blue spaces in this gland.
18
Note the large number of blue-staining
inflammatory cells in this tissue. These cells
appear to be forming germinal centers. Some
residual thyroid gland tissue can be seen in this
section (arrows).
19
Inflammatory cells forming germinal centers
20
Inflammatory cells and residual thyroid tissue
21
Inflammatory cells infiltrating into residual
thyroid tissue (arrows)
22
Lymphocytes and plasma cells surrounding the
thyroid gland epithelium
23
Lymphocytes and plasma cells surrounding the
thyroid gland epithelium. Large, eosinophilic,
degenerating thyroid gland cells (Hurthle cells)
can be seen in this section (arrows).
24
Angiogram of abdominal viscera demonstrating
numerous aneurysms throughout the mesenteric
circulation (arrows)
25
Angiogram of the liver demonstrating numerous
aneurysms throughout the hepatic circulation
(arrows)
26
Angiogram of the kidneys demonstrating numerous
aneurysmal dilations in the renal circulation
(arrows)
27
A mesenteric vessel from this case of
polyarteritis nodosa (arrow) The vessel is
completely occluded by thrombotic material and
the vessel wall is infiltrated with inflammatory
cells.
28
Mesenteric vessel Note the thrombotic material
occluding the vessel (arrows) and the
inflammatory cell infiltrate in the wall of the
vessel and in the surrounding adventitia.
29
Mesenteric Artery Marked inflammatory cell
response 1 Fresh hemorrhage 2 Thrombotic
material
30
Vessel wall There is hemorrhage and infiltration
with inflammatory cells, primarily neutrophils
(arrows).
31
Small vessel with a rim of fibrinoid necrosis
(arrow)
32
There is an area of necrosis in the adrenal gland
(1) and an affected vessel adjacent to the gland
(2).
33
Affected vessel from previous image The vessel
wall is infiltrated with inflammatory cells and
the vessel lumen is completely occluded (arrow).
34
Heart with areas of fibrosis in the myocardium
(arrows) Note that the large epicardial coronary
artery is normal.
35
Affected vessels in the heart (arrows) There are
areas of fibrosis (old infarcts) in the
myocardium adjacent to these affected vessels.
36
Affected vessel in the heart The lumen is
completely occluded.
37
Cut section of lungs from patient with
scleroderma Note extensive fibrosis of the lung
parenchyma.
38
Cut section of one lung from patient with
scleroderma Note extensive fibrosis of the lower
lobe (arrows).
39
Cut section of one lung from patient with
scleroderma Note extensive fibrosis and the
severe emphysematous changes.
40
Cut section of one lung from patient with
scleroderma Note extensive fibrosis and the
severe emphysematous changes.
41
Heart from this case There is thickening of the
left ventricular wall and some thickening of the
right ventricle as well.
42
Lung Apical lesion representing an old healed
lesion from Mycobacterium tuberculosis infection
43
Lung tissue with multiple circumscribed nodules-
granulomas (arrows)
44
Tb granuloma Note the eosinophilic material in
the center (caseous necrosis) and the epothelioid
macrophages and giant cells around the periphery.
45
Tb granuloma Caseous necrosis is on the left-hand
side of the image. There are multinucleated
giant cells and epithelioid macrophages
throughout the remainder of this tissue.
46
Acid-fast stain Mycobacterium tuberculosis
bacilli stain red.
47
Saggital section of end stage chronic
glomerulonephritis (GN) Note the marked thinning
of the cortex (arrow).
48
Hyalinized glomeruli (arrows) and glomeruli with
thick basement membranes
49
1 Hyalinized glomeruli 2 Glomeruli with
thickened basement membranes
50
Interstitial and vascular lesions in end stage
renal disease
51
Granular membranous immunofloursecence (immune
complex disease) The antibody used was specific
for IgG.
52
Electron micrograph of subepithelial electron
dense deposits (arrows) which correspond to the
granular immunofloursecence in the previous image.
53
Acute poststreptococcal glomerulonephritis In
this case the immune complex glomerular disease
is ongoing with necrosis and accumulation of
neutrophils in the glomerulus.
54
Immunoflourescent pictomicrograph of a glomerulus
from a case of acute poststreptococcal
glomerulonephritis shows a granular
immunoflourescence pattern consistent with immune
complex disease The antibody used was specific
for IgG, but antibody for complement would show a
similar pattern.
55
Electron micrograph demonstrating scattered
subepithelial dense deposits (arrows) and a
polymorphonuclear leukocyte in the lumen.
56
Immunoflourescent pictomicrograph of a glomerulus
from a patient with Goodpastures syndrome The
linear immunoflourescene (arrows) is
characteristic of Goodpastures.
57
Acute rejection Note the kidney is swollen (edema
and inflammation) and there are areas of
hemorrhage throughout the kidney.
58
Acute rejection Kidney Focal accumulations of
cells diffuse cellular infiltrate (blue dots)
throughout the parenchyma
59
Acute rejection Kidney Note cellular infiltrates
60
Cellular infiltrates in kidney undergoing acute
rejection Note that in addition to the diffuse
cellularity, the focal accumulations of cells
seemed to be focused around blood vessels.
61
Kidney undergoing acute rejection Cellular
infiltrate within the interstitium and around the
small blood vessel in the center of the image
62
Kidney undergoing acute rejection Cellular
infiltrate within the interstitium There is some
degeneration (coagulative necrosis) of tubules
and glomeruli.
63
Cellular infiltrate within the interstitium and
in the wall of the blood vessel on the left Acute
Rejection Kidney
64
1 Cellular infiltrate within the interstitium
2 In the wall of the blood vessel Acute
Rejection Kidney
65
Cells infiltrating the wall of the blood
vessel Acute Rejection Kidney
66
Cellular infiltrate within the interstitium and
cells within the renal tubules Acute Rejection
Kidney
67
Chronic Rejection Kidney Note the focal areas of
hemorrhage and inflammatory cell infiltrate
68
Chronic Rejection Kidney Kidney containing a
section of blood vessel that demonstrates a
marked neointimal proliferative response (1). In
this case the lumen is obliterated. Also note
the cellular infiltrate in the interstitium of
the kidney (2) and the paucity of the tubules.
69
Chronic Rejection Kidney Kidney with a focal
area of hemorrhage around a small blood vessel
(left) and congestion of the glomeruli. Note
that there is a marked loss of renal tubules
throughout this section with replacement by
fibrous connective tissue. Also note the
cellularity of the glomeruli.
70
1 Fibrosis 2 Focus of inflammatory cells
indicating that despite the chronic nature of
this lesion, there is still ongoing acute
rejection and renal damage Note the loss of renal
tubules throughout the section.
71
Chronic Rejection Kidney 1 Congestion 2
Glomerulus that is almost completely obliterated
or sclerosed Note the increased cellularity of
the glomeruli with mesangial expansion
72
Rejected kidney with a focus of cellular
infiltrate (left) and a small artery with
neointimal proliferation and stenosis (arrow)
73
Chronic Rejection Kidney Glomerulus with a mild
cellular infiltrate (left) There is extensive
interstitial fibrosis (1), loss of renal tubules,
and the remaining tubules contain protein (2)
indicating severe damage.
74
Chronic Rejection Kidney Renal cortex with
cellular infiltrate and few remaining renal
tubules The cellular infiltrate comprises
macrophages, activated (large) lymphocytes, and a
few neutrophils and plasma cells.
75
Chronic Rejection Kidney Damaged glomerulus Note
the loss of normal capillary structure, the
mesangial expansion, and the infiltration of
large mononuclear cells.
76
Extensive damage to the kidney due to chronic
rejection (loss of tubules and glomerular
lesions) In addition, this kidney was removed
during an episode of acute rejection. The marked
cellular infiltrate indicates acute rejection in
a case of chronic transplant rejection.
77
Acute rejection in a case of chronic rejection
Kidney Cellular infiltrate is composed of
lymphocytes, macrophages, plasma cells, and a few
neutrophils.
78
Acute rejection in a case of chronic rejection
Kidney Note the cellular infiltrate around a
small blood vessel (right) and neutrophils within
renal tubules (arrow).
79
Mediastinal mass encapsulated and contains
cellular areas (blue) and areas of pale red
material Multiple Myeloma with Amyloid
80
Junction between an amorphous hylaine-appearing
area (amyloid) on the right and cellular areas
(plasmacytoid cells) on the left Multiple Myeloma
with Amyloid
81
Demonstrates the cells that make up the tissue
resemble plasma cells and are the malignant cell
of multiple myeloma
82
Vertebral column at autopsy 1 Collapsed
vertebra 2 Multiple variably-sized nodules
within the bone marrow these are accumulations
of malignant plasma cells in this case of
multiple myeloma
83
Liver with amyloidosis Note the pale, swollen
appearance of the liver.
84
Liver with amyloidosis Cut surface The liver
tissue is firm and has a waxy appearance.
Arrows The pale waxy material can be seen within
hepatic tissue.
85
Liver with amyloidosis Eosinophilic hyaline
material (1) present within and between hepatic
tissue (2) There is marked distortion of the
lobular architecture by the amyloid.
86
Amyloid deposits (1) between hepatocytes (2)
87
Liver with amyloidosis Congo red stain reacts
with amyloid, giving it an orange color (arrows).
88
Liver with amyloidosis Congo red stain The orange
amyloid tissue is clearly seen between liver
parenchymal cells.
89
Liver with amyloidosis Congo red stain, partially
polarized light Congo red stained amyloid viewed
through polarized light should give off a classic
apple green birefringence (arrows). Not
demonstrated well here.
90
Kidney with amyloidosis Note the pale yellow
material within the cortex (arrows). This is
indicative of amyloid within the cortex and the
glomeruli. Also note there are multiple red
spots in the cortex. They represent congested
glomeruli due to the vascular compromise produced
by the amyloid.
91
Amyloid deposits within glomeruli (arrows)
92
Tongue with extensive amyloid deposits (1)
separating the skeletal muscle fibers of the
tongue. In many cases the amyloid encircles the
muscle fibers (2) and these muscle fibers are
atrophied.
93
Heart Senile Amyloidosis This tissue was firm
and had a waxy texture. If you use your
imagination, you can see pale yellow areas within
this tissue which represent the amyloid deposits.
94
Heart Senile Amyloidosis At this magnification
the structure looks relatively normal.
95
Heart Senile Amyloidosis 1 Amyloid deposition
throughout the myocardium 2 Deposition in the
wall of the blood vessel
96
Heart Senile Amyloidosis 1 Extracellular
amyloid 2 Deposition in the vessel wall
97
Heart Senile Amyloidosis Special stain for
amyloid, demonstrating the amyloid (1) and
fibrosis (2) in the myocardium. The amyloid is
darker purple/magenta and tends to be more
amorphous. The fibrosis is pink and more
fibrillar.