PROBLEM ? - PowerPoint PPT Presentation
Title:
PROBLEM ?
Description:
Title: IRON DEFICIENCY ANAEMIA Last modified by: Azhar Mubarik Created Date: 5/28/1995 4:12:40 PM Document presentation format: On-screen Show (4:3) – PowerPoint PPT presentation
Number of Views:138
Avg rating:3.0/5.0
Title: PROBLEM ?
1
PROBLEM ?
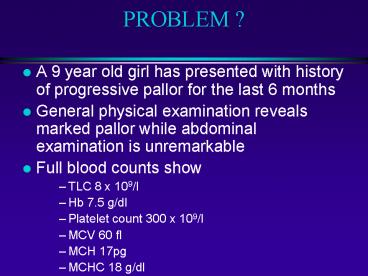
- A 9 year old girl has presented with history of
progressive pallor for the last 6 months - General physical examination reveals marked
pallor while abdominal examination is
unremarkable - Full blood counts show
- TLC 8 x 109/l
- Hb 7.5 g/dl
- Platelet count 300 x 109/l
- MCV 60 fl
- MCH 17pg
- MCHC 18 g/dl
2
PROBLEM ?
- What is the most likely diagnosis ?
- What investigations you will carry out to confirm
the diagnosis ? - Out line management.
3
IRON DEFICIENCY ANAEMIA
Iron deficiency anaemia is the most common of
all the anaemias encountered in clinical
practice. Yet it is most often mismanaged.
4
HYPOCHROMIC MICROCYTIC ANAEMIA
- Iron deficiency anaemia
- Thalassaemia trait
- Anaemia of chronic disorder
- Sideroblastic anaemia
5
IRON BALANCE
Iron is the most abundant metal in human body,
about 3.5 gm in an adult man yet the body
rigorously conserves it like a trace element.
6
IRON CYCLE
Hb synthesis Erythropoiesis
Intestinal absorption 1 mg/day
RBC 2.3 gm
Plasma iron 13-32 umol/l
Loss 1 mg/day
Stores 1 gm
RBC destruction Hb catabolism
7
TOTAL BODY IRON
- Adult male (50 mg/kg) 3.5 gm
- Adult female (35 mg/kg) 2.5 gm
- Hb 2.3 gm
- Stores 1.0 gm
- Mb 0.14 gm
- Enzymes 0.06 6m
8
IRON BALANCE
- Daily loss 1-2 mg
- Average daily in-take 10-15 mg
- Normally absorbed (10) 1-2 mg
- Enhancement in deficiency 3-5 mg
(20-25 0f in-take)
9
IRON ABSORPTION - 1
Cells regulate iron acquisition through
post- transcriptional control of
apoferritin and transferrin receptor
synthesis. mRNA of both proteins contain iron
responsive elements (IRE) capable of binding iron
regulatory proteins (IRP) 1 2. Binding of
these proteins has opposing effects on two
mRNAs.
10
IRON ABSORPTION - 2
Transferrin receptor synthesis is directly
influenced by the rate of erythropoiesis and
indirectly by amount of storage iron (ferritin)
11
IRON ABSORPTION - 3
- Rate of erythropoiesis/amount of ferritin
- Transferrin receptor synthesis
- Transferrin synthesis/secretion in bile
- Apoferritin and transferrin/mobilferrin in
intestinal cell
12
IRON DEFICIENCY
For an individual to become iron deficient, a
prolonged period (approximately 6 years), of
negative iron balance is required.
13
IRON DEFICIENCY - STAGES
A. Pre - latent iron deficiency Reduction in
iron stores without reduction in plasma iron.
Serum ferritin bone marrow iron are
reduced. B. Latent iron deficiency Exhaustion
of iron stores without reduction in Hb
concentration. Plasma iron decreases,
TIBC increases and transferrin saturation
decreases. C. Iron deficiency anaemia Hb
concentration starts declining. Early stage is
discovered by chance. Late stage (Hb 8.0 gm) is
symptomatic.
14
IRON DEFICIENCY ANEMIA PATHOGENESIS - 1
Continued negative iron balance Depletion of
iron stores Reduction in plasma iron Reduction
in Hb synthesis (Increase in free erythrocyte
protoporphyrin, hypochromia, microcytosis) Anaem
ia
15
IRON DEFICIENCY ANAEMIAPATHOGENESIS - 2
- Negative iron balance results from
- Increases requirements (females) or slow
- and steady loss (occult blood loss)
- Decreased in-take (poverty, habits)
- Combination of the two (most common)
- exceeding the physiological limits of absorption
- adjustment
16
IRON DEFICIENCY ANAEMIAPATHOGENESIS - 3
Takes about eight years to develop
iron deficiency It takes another 2-3 years
to become symptomatic Patients with rapidly
developing anaemia seldom become iron
deficient as iron is replaced by way of red
cell transfusions administered to treat it.
17
DIAGNOSTIC METHODS - 1
- A. Assessment of Iron stores
- a. Serum ferritin
- b. Bone marrow iron
- B. Plasma Iron studies
- a. Plasma iron
- b. Serum transferrin (TIBC)
- c. Transferrin saturation
18
DIAGNOSTIC METHODS - 2
C. Serum Transferrin receptors D. Red Cell
Parameters Early stage a. Red cell free
protoporphyrin b. Red cell indices Late
stage a. Definite anaemia b. More marked
changes in red cell indices and morphology
19
MANAGEMENT
The most important component of effective
management for IDA is to find out the cause of
chronic negative iron balance and to treat
it. Replacement therapy alone will not be able
to induce sustained remission.
20
CAUSES OF IRON DEFICIENCY-1
Increased requirements Decreased in-take
Impaired absorption Increased loss (blood
loss, 1 ml 0.5 mg iron )
21
CAUSES OF IRON DEFICIENCY-3
INFANCY AND CHILD HOOD Prematurity (reduced
transfer ) Low birth weight (reduced iron
store) Inadequate in-take Increased
requirement (with growth) Uncommon vascular
anomalies Milk allergy
22
CAUSES OF IRON DEFICIENCY-4
REPRODUCTIVE FEMALES Menstural
disturbances Frequent pregnancies Dietary
habits / Pica Hiatus hernia
23
CAUSES OF IRON DEFICIENCY-5
Hook worms (AD 0.2 ml, NA 0.05 ml / worm /
day) Schistosomiasis Ulcerative lesions of
GIT Chronic Aspirin ingestion (1-4 ml / day with
02 Tab) Haemorrhoids Neoplasms Runners anaemia
(50 of joggers and runners) Nosocomial (ITC 42
ml / day)
24
INVESTIGATIONS TO DETERMINE THE CAUSE
Careful history Thorough physical
examination Urine for Hb, haemosidrin,
ova Faeces for ova, parasites, occult
blood Radiological, Endoscopic
examinations Others
25
CAUSES OF IRON DEFICIENCY-2
Age Sex Socio-economic factors Occupation
26
REPLACEMENT THERAPY-1
Oral administration is best
approach Addition of other elements has no
advantage Enteric coating and sustained release
reduce absorption Modification of dietary
habits greatly improve absorption
27
RESPONSE
Optimal response with 200 mg elemental iron /
day For children 1.5-2 mg / kg / day elemental
iron Peak reticulocyte (5-10) between 5th
- 10th day Hb at 03 weeks 60 to normal, normal
in 2 months Indices normal in 6 months.
28
INDICATIONS FOR PARENTAL THERAPY
Anatomical lesions of upper GIT Functional
lesions of upper GIT Rapid loss Extreme
intolerance Consistent non-compliance Haemodialy
sis
29
CALCULATION OF REQUIREMENT
Requirement (mg ) ( 15 - pt Hb g / dl )x BW
(kg)x 3 Either 2 mg I/M daily Or Total dose I/V
30
REPLACEMENT THERAPY-2
Gain in patient acceptance is more
important than the reduced absorption of
iron
31
CAUSES OF FAILURE
Incorrect diagnosis Complicating
illness Inadequate prescription Continuing loss
/ malabsorption Non compliance
32
PREVENTION
Premature infants 02 mg / kg / day at 02
months Infants 01 mg / kg / day at 04
months Pregnancy 60 mg ( one Tab of 300 mg )
daily Others According to loss
33
IN THE NAME OF ALLAH THE BENEFICENT AND THE
MERCIFUL
34
IRON DEFICIENCY ANAEMIA
Maj Gen Muhammad Ayyub MBBS (Pesh), Ph.D
(London), FRC Path (UK), Consultant Haematologist
Commandant Army Medical College, Rawalpindi
35
ß THALASSAEMIA TRAIT
- Heterozygous state of ß thalassaemia
- Usually asymptomatic
- Significance of diagnosis
- Prenatal counselling
- Prenatal diagnosis
- Un necessary iron replacement therapy?
36
LABORATORY INVESTIGATIONS
- Blood complete picture
- Haemoglobin
- Mild anaemia as compared to iron deficiency
- Red cell indices
- Hypochromic microcytic
- Platelet count
- Normal
- RDW
- Normal
37
LABORATORY INVESTIGATIONS
- RBC morphology
- Hypochromic microcytic blood picture with mild
poikilocytosis and target cells - Definite diagnosis
- Haemoglobin electrophoresis
- Hb A2 gt 3.5
38
SIDEROBLASTIC ANAEMIA
- Refractory anaemia due to defect in haem
synthesis - Defined by presence of gt 15 ring sideroblasts in
bone marrow out of marrow erythroblasts - Ring sideroblast?
39
CLASSIFICATION
- Hereditary
- X linked
- Mitochondrial
- Autosomal
- Acquired
- Primary
- Myelodysplasia
- Secondary
- Alcohol, lead, Anti TB, megaloblastic anaemia etc
40
MANAGEMENT
- Blood transfusion
- Pyridoxine
- Thiamine
- Folic acid
41
DIFFERENTIAL DIAGNOSIS - 1
IDA THAL TR CHR DIS SIDERO Hb.
(gm/dl) 8.0 12.0 10.0 6.0 MCV
(fl) 74 68 86 77 MCHC (gm/dl) 28 31 32 25 Ani
so/Poikilo 1-3 1-3 Basophilic
stippling 0 2 0 2 Target cells 5 2 Di
morphism 0 3
42
DIFFERENTIAL DIAGNOSIS - 2
IDA THAL TR CHR DIS SIDERO Serum iron
N N Transferrin N Saturation
N Ferritin N Transferrin
N N N receptors
43
- A 42 years old female presented with
- h/o pallor and generalized weakness and numbness
- lower limbs for one year.
- General physical exam revealed marked pallor,
red beffy tongue. Abdominal exam is unremarkable.
- FBC TLC 3.0 x 109/l
- HB 6.5 g/dl
- Platelet 100 x 109/l
- MCV 112 fl
- MCH 30 pg
44
INTRODUCTION
- Megaloblastic anaemias are a group of disorders
characterised by the presence of distinctive
morphological appearance (megaloblastic) of
erythroid cells in the bone marrow. - Majority of the cases have vitamin B12 or folate
dificiency
45
CAUSES
- Vitamin B12 deficiency
- Folale deficiency
- Defective Vitamin B12 or folate metabolism
- Transcobalamin II deficiency
- Antifolate drugs
- Defects of DNA synthesis
- Congenital orotic aciduria
- Acquired alcohol, hydroxyurea
46
MACROCYTOSIS
- Megaloblastic
- Vitamin B12 deficiency
- Folate deficiency
- Non megaloblastic
- Physiological
- Pregnancy
- Infants
- Pathological
- Alcohol
- Liver disease
- Myeloma
- MDS
- Myxodema
- Reticulocytosis
47
MACROCYTOSIS, A PRACTICAL APPROACH
- Check history for alcohol and liver disease
- Check complete blood counts for evidence of
marrow disease - Check B12 and folate levels
- Check LFTs and S TSH
- Check reticulocyte count
48
PATHOPHYSIOLOGY
Methyl tetrahydrofolate
homocysteine
B12
Methionine
Tetrahydrofolate
DHF polyglutamate
Tetrahydrofolate polyglutamate
5,10 methylene THF polyglutamate
DNA
49
(No Transcript)
50
CLINICAL FEATURES
- Anaemia
- Jaundice (lemon yellow tint)
- Glossitis, angular stomatitis
- Peripheral neuropathy
- Cardiovascula effects
- Features due to thrombocytopenia
51
VITAMIN B12 DEFICIENCY
- CAUSES
- Nutritional
- Malabsorption
- Gastric pernicious anaemia, intrinsic factor def
- Intestinal intestinal stagnant loop syndrome,
ileal resection, fish tape worm
52
(No Transcript)
53
VITAMIN B12 TRANSPORT ABSORPTION
Dietary cobalamin
Haptocorrins
(saliva)
Intrinsic factor
(Gastric parietal cells)
(Ileum)
Cubilin receptors
(plasma)
Transcobalamin II
Bone marrow and other tissues
54
VITAMIN B12 NUTRITIONAL ASPECTS
- Normal daily intake 7-30 ug
- Source Animal origin only
- Daily requirement 1-2 ug
- Body stores 2-3 mg
- Maximum absorption 2-3 ug /day
- Enterohepatic circulation 5-10 ug/day
- Plasma transport transcobalamin II
- Therapeutic form hydroxycobalamin
55
FOLIC ACID DEFICIENCY
- CAUSES
- Nutritional
- Malabsorption
- Excess utilization
- Physiological pregnancy, lactation
- Pathological
- Haematological diaeases
- Malignant diseases
- Inflammatory diseases
- Miscellaneous
- liver disease, drugs, intensive care
56
FOLIC ACID ABSORPTION TRANSPORT
Dietary folate
Methyl THF
Duodenum jejunum
(Absorption)
Plasma
Bound
Unbound
57
FOLIC ACID NUTRITIONAL ASPECTS
- Daily intake 200-250 ug
- Source Animal and plant origin
- Daily requirment 100-150 ug
- Body stores 10-12 mg
- Maimum aborption 50-80 of dietary intake
- Enterohepatic 90ug/day
- Therapeutic form folic acid
58
LABORATORY DIAGNOSIS
- Mporphology
- macrocytosis with macro ovalocytes
hypersegmented neutrophils - Anisopoikilocytosis
- NRBCs
- Basophilic stippling
- Howell jolly bodies
59
LABORATORY DIAGNOSIS
- Unconjugated bilirubin increased
- Serum LDH increased
- Serum hydroxybutyrate increased
- Serum methylmalonate increased
- Serum Homocysteine increased
60
LABORATORY DIAGNOSIS
VITAMIN B12 AND FOLATE LEVELS
B12 deficiency Folate deficiency
S vitamin B12 Low normal
S folate Raised low
Red cell folate Low low
61
LABORATORY DIAGNOSIS
- BONE MARROW EXAMINATION
- Megaloblastic heperplastic erythropoiesis
- Myelopoiesis shows giant myelocytes
metamyelocytes - Increased iron
62
BONE MARROW APPEARANCE
63
LABORATORY DIAGNOSIS
- Investigations for cause of megaloblastic anaemia
- Anti intrinsic factor antibodies
- Antiparietal cell antibodies
- Antigliadin antibodies
- Duodenal biopsy
- Endoscopy
- Barium studies
- Schilling test
- DICOPAC test
64
THANK YOU