Flexibility - PowerPoint PPT Presentation
Title: Flexibility
1
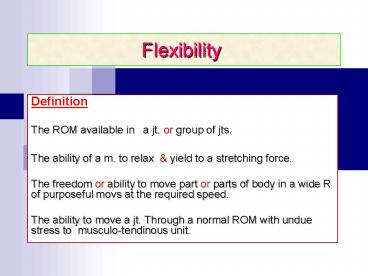
Flexibility
- Definition
- The ROM available in a jt. or group of jts.
- The ability of a m. to relax yield to a
stretching force. - The freedom or ability to move part or parts of
body in a wide R of purposeful movs at the
required speed. - The ability to move a jt. Through a normal ROM
with undue stress to musculo-tendinous unit.
2
- Flexibility
- Extensibility of periarticular tissues to allow
normal motion of a joint. or a limb. - Hypermobility
- The ROM in excess of the accepted normal in most
of joints. (may be normal) - Laxity
- Excessive jt. instability abnormal motion of a
given joint. (pathological)
3
Types of Flexibility
- Ballistic Flexibility
- Normal ROM associated with bouncing rhythmic
movements. - Dynamic Functional Flexibility
- Activities that need certain angle to certain
joints. particular patterns (usual
activities).
4
Factors Affecting Flexibility
- Wrong habits ? flexibility sitting for a long
period (in school, watching TV, computer work,
sedentary games)
- Good habits ? ? flexibility.
- Genetic factors females gt males.
- Hormonal factors females gt males.
- Body build proportion ? height ? ? flexibility
. - Body wt. ? ? ? flexibility
- Age flexibility changes during a certain age
? 2 - 6 y ? 6 - 12 y
? 18 - 22
y
? 35 - up - Skills sport activities ? ? flexibility.
5
Contractile Non-contractile Tissue
- Contractile
- Ms
- Non-contractile
- Skin
- CT
- Ligaments
- Tendons
- Capsules
- Synovial Membrane
6
N.B.
- Soft tissues that can restrict joint motion are
- Skin
- CT, tendons, ligaments
- Ms
- Each one has unique qualities affecting its
extensibility (ability to elongate). - Factors affecting soft tissues lengthening
- Velocity of stretch force
- Intensity of stretch force
- Duration of stretch force
- Mechanical properties of contractile
non-contractile tissues - Neuro-physiological properties of contractile
tissues
7
When soft tissue is stretched, either elastic or
plastic changes occur
- Elasticity
- Ability of soft tissue to return to its
resting length after passive stretching. - Plasticity
- Tendency of soft tissue to assume new
greater length after the stretch force has been
removed. - Both contractile non-contractile tissues have
elastic plastic properties.
8
Degrees of Deformity
- 1st degree (grade I) can be corrected actively
(shortness). - 2nd degree (grade II) can be corrected
passively (shortness). - 3rd degree (grade III) cant be corrected
neither
actively nor passively (contractures).
9
Indications of Stretching
- Limited ROM due to adhesions scar tissues
formation leading to shortening of Muscles, CT
Skin. - Prevention of structural (neglected soft tissue ?
shortening ? structural limitations ?skeletal
deformities - (prophylactic intervention)
- When contractures interfere with every day
functional activities or nursing care. - When theres muscle weakness opposing tissue
tightness. - Tight muscle must be elongated before
weak m. can be effectively strengthened.
10
Goals of Stretching
- 1. To regain or re-establish normal joint. ROM
mobility of soft tissue surrounding a jt.. - 2. To prevent irreversible contractures.
- To ? general flexibility of a part of the body
prior to vigorous strengthening excerises. - 4. To prevent or minimize risk of
musculo-tendinous injuries related to specific
physical activities sports.
11
Precautions to Stretching
- Dont passively stretch (force) a joint beyond
its normal ROM - (Remember that normal ROM varies among
normal individuals). - Newly united should be protected by
stabilization between site the joint where
motion takes place. - Extra caution in pts. with known or suspected
osteoporosis due to - Disease b. Prolonged bed rest
- c. Aging d. Prolonged use of
steroids (cortisone) - Avoid vigorous stretching of muscles CT that
have been immobilized over a long period of time.
CT (tendons ligaments) lose their tensile
strength after prolonged immobilization.
12
Precautions to Stretching
- High intensity, short duration procedures ?
traumas ? soft tissue weakness - Stretching should be low intensity for long
duration stretch. - Strengthening excerises should be added to
stretching program at some point,
so patient will be able to develop
appropriate balance between flexibility
strength.
13
Contraindications to Stretching
- Acute infections.
- Signs of inflammation.
- Pain at the site to be stretched.
- Osteomyelites (acute stage).
- Bone tumors.
- Advanced osteoporosis.
- 7. Severe spasticity.
- 8. Pain that isnt yet evaluated by the PT or
physician.
- Joint laxity (hypermobility).
- 10. Joint subluxation.
- 11. Joint dislocation.
- 12. Joint fusion.
- 13. Joint deformity.
- 14. Tissue adhesions (contractures).
- 15. Acute Traumas
14
Principles of Stretching
- Consider the best stretching type to ? ROM.
- Explain goals of stretching to the pt.
- Position the pt. in a comfortable relaxed pos. ?
allow the best plane of motion to conduct
stretching. - Free the area from restrictive clothing, bandage,
splints. - Apply superficial heating to the soft tissues to
be stretched. - It will ? possibility of injury.
- Stretch direction is done opposite to tightness.
- 7. The pt. must be completely relaxed
throughout stretching ,employ relaxation
techniques before stretching.
15
- Stretching movs. or exs. are performed at least 3
times/week to maintain
flexibility. Progress to daily stretching
routines. - 1-3 repetitions of each stretch must be done. The
No. of repetitions can be ? if the goal is to ?
ROM. - 10. Degree of stretch can be ? or ? depending
on time of stretch
external force applied. - 11. Tension produced shouldnt cause pain, the
pt should only feel
a slight tension, which ? with stretching. (due
to adaptation) - 12. Stretch ? gradually, building to a max. as
the tissues release. - 13. Stretch should be removed gradually to
prevent rebouncing or
tightening of the ms.
16
Stretching depends on
- Type of stretching force.
- Intensity.
- Duration
- Velocity.
17
Types A. Passive Stretching
- PT applies an external force controls stretch
- 1direction, 2speed, 3intensity 4duration to
the tight m.. - Dont confuse between
- Passive stretching ? elongation of soft tissues
beyond full R of restriction. - Passive ROM exs.
? applied
within the unrestricted (available) ROM. - Pt. must be completely relaxed during passive
stretching. - Time of stretch force is usually 15 30 sec
repeated several times during ex. session.
18
1. Manual Passive Stretching
- Usually considered a short-duration stretch.
- No specific No. of secs. are determined to be the
most effective duration.
- In a study to stretch hip abd. of healthy
subjects 15, 45 sec 2 min at the same speed ?
no difference. - Intensity duration of stretch depend on
- Pts tolerance
- PT strength endurance
- Low intensity, long duration manual stretch is
more comfortable tolerated by pt.
19
Maintained versus Ballistic Stretch
- MANUAL PASSIVE STRETCH
- HIGH INTENSITY STRETCH
Inhibit stretch reflex ? Muscle tension
Facilitate muscle contraction ? tension
20
2. Prolonged Mechanical Stretch
- Low intensity external force (5-15 lb) (2 6 kg)
applied to shortened tissues over a prolonged
period by mech. equipments. - Stretch force is applied through positioning with
weighted traction, pulley system, dynamic splint
serial casts. - Prolonged stretch may be maintained for 20-30
min. or longer ? effective stretch ? ROM - (low intensity mechanical stretch).
- Comparing long-duration mech. stretch manual
passive stretch (
the latter is rather short theres transient
temporary achievement of ROM).
21
Examples
- Bohannon evaluated the effectiveness of an 8 min
mechanical hamstring stretch compared to a 20 min
or longer using overhead pulley system. The 8 min
stretch resulted in a small ? in hamstring
flexibility, which was lost in 24 hrs. - It was suggested that 20 min or longer
stretch is more effective to ? ROM has a more
permanent basis. - Use of tilt table-wedge board standing for 30
min/daily ? ? dorsiflexion in neurological pts. - Dynasplint (dynamic splint) ? prolonged low
intensity stretch of elbow, wrist, knee
ankle ? ? ROM. - Low intensity prolonged stretch of 5-12 lb
applied for 1 hr/daily
has been found to be more effective than manual
passive stretch over a 4-week period with pts
with bilateral knee flexion contractures. It is
more comfortable
22
Permanent lengthening
- (Plastic changes in contractile non-contractile
tissues)
has been reported with long duration
stretch. - The term Permanent lengthening means that the
length is maintained after the stretching force
is removed.
23
3. Cyclic Mechanical Stretching
- It is passive stretching using a mechanical
devices as an Autorange using a 20-sec high
intensity (up to the patients pain tolerance). - Intensity of stretch,
- Length of each cycle,
- No. of stretch cycles/min Can be adjusted with
the unit. - It is similar may be used as a useful
alternative to manual passive stretching.
24
B. Active Inhibition
- Is a tech. in which the patient reflexively
relaxes muscles to be elongated prior to
stretching maneuver.
When the patyent is relaxed ? minimal R to
elongate the m. - It relaxes only the
- Contractile structures,
- Not the CT. - The m. must be
Normally
innervated and Under voluntary control. - It Cant be used with pts having
1.
Weakness,
2. Spasticity
3. Paralysis (From a neuromuscular
disease). - It Can be used in
Post-operative patient. (to avoid tightness).
25
Active Inhibition Techniques.
- Contract-relax (hold-relax)
- Pt performs an isometric contraction of tight
muscle before it is - passively stretched (lengthened).
- M. will relax as a result of autogenic
inhibition (Golgi tendon
organ may fire at ? tension). - Contract-relax-contract (hold-relax-contract).
- 1st a contraction of tight muscle.
- 2nd relaxation of tight muscle. (autogenic
inhibition). - 3rd concentric contraction of opposite muscle
(reciprocal - inhibition of tight m.).
- In a study, the contract-relax-contract produced
a greater ? in ankle dorsiflexion gt
contract-relax tech. (in short calf m ). - Both techs produce ? ROM gt manual
stretching.
26
3. Agonist Contraction
- Agonist muscle opposite to the tight muscle.
- Antagonist Tight muscle.
- Patient dynamically contracts (shortens)
the muscle opposite to the tight
muscle against resistance ? reciprocal inhibition
of tight muscle.
27
C. Self-Stretching
- Is a type of flexibility excerises. the patient
carries out by himself. - Pt. may passively stretch his tightness by
- His/her own body weight. ( gravity)
- Active inhibition.
- Manual passive stretch (using sound limb)
28
(No Transcript)
29
(No Transcript)
30
Peripheral joint mobilization
- Definition
- Peripheral joint mobilization (PJM) is the use
of skilled graded forces to mobilize joints
to improve motion
normalize joint function.
31
Mobilization Techniques are used to
- Improve jt. nutrition.
- Improve m. spasm tension
- Reduce pain.
- Reverse jt. hypomobility.
- Improve or restore motion.
- Treat jt. dysfunction as stiffness.
32
The PT should recognize
- When the mobilizing techniques are
indicated (at any ROM), or - If other stretching techniques are more
effective (stretching, stretching exs or CTM) - To regain the lost motion
33
A. Joint Mobilization
- Is a type of passive mov performed by the PT at a
speed slow enough that the pt. can stop the mov. - The tech. may be applied with
1. Oscillatory motion or
- 2. Sustained stretch
- to
- ?Pain or
- ?mobility.
- The tech. may use
- Physiologic or
- Accessory movs.
34
Mobilization Techniques
- Physiologic movements
- Movs. that the pt can
perform voluntarily as
flex, ext, abd,
add rot. - 2. Described as (Osteokinematic). i.e. mov of
bones in relation to each others
- Accessory movements
- Movs within the jt surrounding tissues that are
necessary for normal ROM, cant be done by pt. - 2. Described as a.
Component motions b.
joint play.
35
Accessory motions
- Accessory motions
- Motions that
accompany active mov, but - Arent under voluntary control
- Component mov is the often used term with
accessory mov. - As
upward rot. of scapula clavicle
occurring in sh. flex.
- B. Joint Play
- Motions that occur in jts
distensibility or give in of the jt
capsule,
which allow bones to move. - Are necessary for normal functioning through the
ROM. - Can be demonstrated passively,
- Cant be performed actively by the pt.
- Include
distraction, sliding, compression, rolling,
spinning of the jt surfaces. - Arthrokinematic
is used to describe these motions
of bone surfaces within the jt.
36
B. Manipulation
- Is a passive mov using
physiologic or accessory motions.
It may be applied
1. With a thrust , (cyropractic) or 2.
Under anesthesia
37
B. Manipulation
- THRUST
- A sudden mov performed
with a high velocity. - Without anaesthesia.
- Short amplitude motion, cant be
prevented by the pt. - Performed
At end of pathologic limit
(end of available ROM,
when theres
restriction). - Using
1. Physiologic, or
2. Accessory movs. - Effects
- 1. Snaps adhesions.
- 2. Stimulates jt receptors.
- MANIPULATION UNDER ANAESTHESIA
- Medical procedure used to
restore full ROM by
breaking adhesions surrounding jt. - With anaesthesia.
- Performed through
1. Rapid thrust, or
2. Passive stretch. - Using
1. Physiologic, or 2.
Accessory movs.
38
Factors Affecting Jt. Motion
- A. Jt. shape.
- B. Types of Motion.
- C. Other Accessory motions.
39
Factors Affecting Joint motion
- A. Joint Shape
- The type of motion is influenced
by jt. shape. - Ovoid one convex surface
one concave (as A). - Sellar (Saddle) one surface is concave
in one direction convex in the other,
with the opposing surface convex
concave (as a horse back
rider) (as B).
40
B. Types of Motion
- When a bony lever (bone) moves about an axis of
motion ? mov of bony surfaces on the
opposing bone surface within the jt. - i.e.
- Movement of bony lever
- Called swing as (flex, ext, add, abd
rot.) - - Measured in degrees.
- Called ROM. - 2. Motion of the bony surfaces
- Within jt is
a combination of rolling, sliding spinning. - - These accessory motions allow
greater angulation of bone as it
swings. - - This needs adequate capsule
laxity or jt. play.
41
a. Roll
- One bone rolls on another. The surfaces are
incongruent. - New points on one surface meet new points on the
opposing surface. - Results in angular motion.
- Always rolling occur in the same direction of the
mov.,
whether the surface is convex or
concave. - Theres compression of the surface on the side to
which the bone is angulating separation on the
other side. - In normal functioning jts, pure rolling doesnt
occur alone, but in combination with sliding
spinning.
42
b. Slide
- One bone slides across another.
- For pure slide, the surface must be congruent
either flat or curved. - Theres no pure slide as jt surfaces arent
completely congruent. - Same point on one surface comes into contact with
new points on the opposing surface. - Direction of slides depends on whether the
surface is convex or concave.
43
- If the moving surface is convex
? Sliding is in the opposite
direction of angular mov. - If the moving surface is concave ?
Sliding is in the same direction
as the angular mov. - This mechanical relationship is known as
convex-concave rule. It determines the direction
of the mobilization force, when jt mobilization
gliding techniques are used.
44
c. Combined roll-sliding in a joint
- The more congruent the jt surface
? the more sliding of one bony partner on the
other with movs. - (e.g. metatarsals metacarpals)
- The more incongruent the jt surface ? the more
rolling movs. - (e.g. hip sh)
45
For Joint Mobilization Techniques
- Sliding
- Is used to
- ?
- Restore jt. play
- Reverse jt. Hypomobility
- Rolling
- Is not used, as
- ?
- Jt. Compression
- E.g. hip abd add
- sh abd add
46
- When PT passively moves the articulating surface
in the direction in which the
slide normally occurs
? Translatory glide (glide) - ?
- used to
- 1. Control pain or 2. Stretch
capsule - If applied gently If with
stretch force
47
d. Spin
- Rotation of one bony segment about a stationary
mechanical axis. - Spinning rarely occurs alone, but in combination
with rolling sliding. - 3 examples of spinning in the body jts
- Sh. with flex/ext.
- Hip with flex/ext.
- Radio-humeral with sup./pron.
- Knee ext either by closed or open chain
48
C. Other Accessory Motions that affect the Joint
- e. Compression.
- f. Traction (AB).
49
e. Compression
- Is the ? in jt space.
- Occurs in LL spinal jts with wt. bearing.
- Some compression occurs as m. cont ? provide
stability to jt. - As one bone rolls on the other, some compression
occurs on
the side to which the bone is
angulating. - Normal intermittent compression loads
? help in moving synovial
fluid
so ? maintain cartilage health. - Abnormal high compression loads
?
articular cartilage changes deterioration.
(friction ? erosion OA)
50
f. Traction
- Distraction or separation of jt surfaces.
- For distraction to occur, the surfaces must be
pulled apart. The mov isnt always the same. - Pulling on the long axis of one bone
(as pulling the shaft of humerus
? glide jt surface) (long axis traction). - Distraction of gleno-humeral jt requires a pull
at a 90 to the glenoid fossa ? distraction jt
traction or jt separation. - Distraction is used to
- Control or relieve pain If applied gently.
- Stretch the capsules If applied with stretching
force.
51
Effects of Joint Motion
- Skim. biologic activity by moving synovial fluid
? brings nutrients to the avascular articular
cartilage of jt surfaces intra-articular
fibrocartilage of the menisci. - Maintains extensibility strength of
articular
periarticular tissues (ligs, ms, tendons
capsules). - With immobilization
? fibrofatty prolifiration
? intra-articular
adhesions biochemical changes in tendons, ligs
jt capsule ? m.
contractures , jt stiffness lig. weakening. - Provide proprioceptive feedback (awareness of
pos. mov. sense) - Static pos. sense of speed of mov.
- Change of speed of mov.
- Sense of direction of mov.
- Regulation of m. tone.
52
Indications of Joint Mobilization
- Pain, m. guarding spasm
- All can be treated with gentle jt play tech
to stim.
neurophysiological mechanical effects. - Neurophysiological effect
Small amplitude oscillatory
mov ? stim mechanoreceptors
? ? transmission of nociceptive stimuli
at spinal cord brain stem levels. - Mechanical effects
- Small-amplitude distraction or gliding mov ?
synovial fluid motion ? bring
nutrients to the avascular portions of articular
cartilage.
(? pain of ischemia) - Gentle jt-play ? maintain nutrient exchange ?
prevent painful effects of stasis when a jt is
painful or swollen cant move through a ROM.
(but not in
acute or massive swelling)
53
Reversible Jt. Hypomobility
- Can be treated with
- 1. Progressive vigorous jt. play stretching
techs.
? elongate hypomobile structures. - 2. Sustained or oscillatory stretch forces
? mechanically distend shortened tissues.
54
- Progressive Limitations
- Diseases that progressively limit movement
can be treated by jt. play techs to - 1. Maintain available motion.
- 2. Retard progressive mechanical restrictions.
- 4. Functional Immobility (obligatory
bedriddeness) - In this case the aim is to
- 1. Maintain available jt. play.
- 2. Prevent degenerating.
- 3. Delay or reduce the effects of immobility.
55
N.B. Mobilization techniques
- Cant change the disease process of disorders as
- Rheumatoid arthritis.
- Inflammation.
- It only can
- Minimizes pain.
- Maintain available jt. Play.
- Reduces effects of mech. limitations.
56
Contra-indications
- Hypermobility AS PJM ?
- Potential necrosis of ligs. or capsules.
- (Hypermobile pts may benefit from jt. play tech.
if kept within the limits of motion).
57
- 2. Joint Effusion
- Never mobilize or stretch a swollen jt with
1.
mobilization or
2. passive
stretching.
The capsule is already stretched by the extra
fluid. Extra
fluid m. response to pain (spasm) ? limited
motion. - Gentle oscillating motions that dont stretch
capsule or stress it ? - Improve fluid flow.
- ? pain.
- Maintains available jt play.
- If pt response to jt play is ? pain or jt.
Irritability
The techs. were either - Too vigorous, or
- Dont suit the current state of pathology.
58
- 3. Inflammation
- Stretching in presence of inflammation ?
- ? Pain.
- ? muscle guarding.
- Greater tissue damage.
- Spreading the inflam. process infection.
59
Precautions
- In most cases jt mobilization is safer than
passive angular stretching. - But
- Sometimes Jt mobilization can be used with
extreme care in - Malignancy - spread growth.
- Excessive pain - m. guarding, prevent mov.
- Total jt. replacement
- disl. or
loosen int. fixation. - Bone disease (Osteoporosis, TB, Rickets).
- Unhealed (site stabilization)
- re-fracture. - Hypomobility (in associated jts m. weak)
-?
capsule laxity, lig. Weakness jt disl.
60
Procedure for Applying Jt Mobilization Techniques
61
3 Possibilities for pain
- !!!! While moving or mobilizing found!!!!
- Before tissue limitation
(after acute injury
or active stage of a disease),
use pain inhibiting jt. tech to
relieve pain maintain jt. play. - With tissue limitation
(as damaged tissue begins to heal) (subacute),
use
gradual gentle stretching tech to tight tissue,
but Dont exacerbate
pain by injuring the tissues. - After tissue limitations
(as
stretching a tight capsule or a peri-articular
tissue of ch. stiff jts),
use ? force of the stretching
techniques.
62
If the capsule is limiting the motion, theres
63
B. Grades of mov. (Dosage, Amplitude)
- 2 systems of techniques
- 1. Graded oscillation.
- 2. Sustained translatory jt. Play.
64
1. Graded Oscillation Tech. Dosage
Grade I Small amplitude rhythmic oscillations at the beginning of ROM.
Grade II Large amplitude rhythmic oscillations within the ROM, but not reaching the limitation.
Grade III Large amplitude rhythmic oscillations up to the limit of available motion stressed into tissue resistance.
Grade IV Small amplitude rhythmic oscillations, up to the limit of the available motion stressed into tissue resistance.
Grade V Small amplitude, high velocity, thrust tech.. Performed to break adhesions at the level of available motion (manipulation or chiropractic). (Stretch)
65
Graded oscillation technique
66
Techniques
- Oscillations may be done using
- 1- Physiologic (osteokinematic) motions.
- 2- Jt. play (arthrokinematic) techs.
67
Sustained Translatory jt. Play Technique
- Grade I (Loosen)
-
Small
amplitude distraction, applied where no stress is
placed on the capsule. - Equalizes cohesive force,
- 2. M. tension
- 3. Atmospheric pressure acting on the jt.
- Grade II (Till tightness)
- Distraction or glide applied to tightend
tissues around jt. - Grade III
- Distraction or glide with large enough
amplitude to place - a stretch on jt. capsule surrounding
peri-articular structures.
68
Sustained translatory joint-play technique
69
Uses
- Grade I Used with gliding motions to relieve
pain. - Grade II Used to determine how sensitive the jt
is. - Grade III
Used to stretch jt.
structures ? jt play. - Technique
- This grading system describes jt. play
techniques that separate or glide (slide) jt
surfaces.
70
N.B.
- The consistency between the dosage of the two
grading systems is grade I (no tension on the jt
capsule or surroundings). - Grade III (sustained stretch) IV (oscillation)
are similar in dosage as they are applied with a
stretch force at the limit of the motion. - Using oscillating or sustained tech., depends on
the pts response. - Pain management use oscillating tech.
- Loss of jt. play ? function use sustained
stretch. - To maintain available R.
Use
either grade II! oscillating or II sustained
technique.
71
C. Patient Position
- C. Patient Position The pt. treated extremity
should be carefully positioned relaxed. - 2. The jt. is positioned so that the capsule has
greatest laxity.
72
D. Stabilization
- Firm comfortable stabilization for proximal
parts by using - Belt.
- PT hand.
- External assistance.
73
E. Force
- Treatment force
(gentle or strong) is applied as close
to the opposing jt. surfaces as possible. - The larger the contact surface of PT hand
- ? the more comfortable procedure will be.
- e.g. use flat surface of the hand instead of
forcing with the thumb.
74
F. Direction of Movement
- Either parallel to, or perpendicular to ttt
plane. - Jt. traction
Perpendicular to ttt
plane. - The entire bone is moved ? jt surfaces are
separated. - Gliding tech.
Parallel to the ttt plane. - This is determined by using the
convex-concave rule. - - If the surface of moving bone is convex
-? opposite direction glide. - - If the surface of moving bone is concave ?
glide in the same direction. - The entire bone is moved, so theres gliding
of one jt. surface on the other. - No swing of the bone that causes rolling
compression of the jt. surfaces