Laparoscopic Radical Prostatectomy: Oncological and Functional Outcomes - PowerPoint PPT Presentation
1 / 1
Title:
Laparoscopic Radical Prostatectomy: Oncological and Functional Outcomes
Description:
Laparoscopic Radical Prostatectomy: Oncological and Functional Outcomes Following Fellowship Training. T.R.J. Gianduzzo*, C. Chabert , L. Osgood . – PowerPoint PPT presentation
Number of Views:215
Avg rating:3.0/5.0
Title: Laparoscopic Radical Prostatectomy: Oncological and Functional Outcomes
1
Laparoscopic Radical Prostatectomy Oncological
and Functional Outcomes Following Fellowship
Training.
T.R.J. Gianduzzo, C. Chabert, L. Osgood. The
Wesley Hospital, Brisbane, Qld John Flynn
Hospital, Tugun, Qld Lismore Base Hospital,
Lismore, NSW.
No. 091
Introduction Radical Prostatectomy (RP) is a
technically demanding procedure that has a
significant learning curve irrespective of
whether it is performed open, laparoscopically or
robotically. Fellowship training aims to reduce
that curve and improve operative outcomes. We
present the initial series of laparoscopic
radical prostatectomy (LRP) by 2
fellowship-trained surgeons TRJG and CC.
Preoperative Gleason grades were Gleason 6 (13),
Gleason 7 (74) and Gleason 8-10 (13).
Nerve-sparing surgery was performed in a total of
72 of patients. This was unilateral in 32 and
bilateral in 68. Final pathological stage was
pT2 (58), pT3 (42). The positive margin rates
for pT2 disease was 1.1 and for pT3 disease was
32.8. Five patients received planned adjuvant
radiotherapy for high volume pT3 disease. There
was 1 PSA failure.
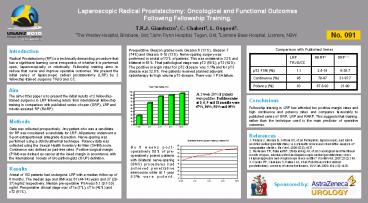
Comparison with Published Series
LRP TRJG/CC RARP3 ORP1,2
pT2 PSM () 1.1 2.5-18 6-36.7
Continence () 95 70-97 31-97.7
Potency () 83 67.8-93 21-90
Aim The aim of this paper is to present the
initial results of 2 fellowship-trained surgeons
in LRP following return from international
fellowship training in comparison with published
series of open (ORP), LRP and robotic-assisted RP
(RARP).
At 1 week 28 of patients were pad free. Pad free
rates at 3, 6, 9 and 12 months were 67, 86, 91
and 95.
Conclusions Fellowship training in LRP has
afforded low positive margin rates and high
continence and potency rates and compares
favourably to published series of ORP, LRP and
RARP. This suggests that training, rather than
the technique used is the main predictor of
operative outcomes.
Methods Data was collected prospectively. Any
patient who was a candidate for RP was considered
a candidate for LRP. All patients underwent a
5-port extraperitoneal antegrade dissection.
Nerve-sparing was performed using a strictly
athermal technique. Potency data was collected
using the Sexual Health Inventory for Men (SHIM)
score. Continence was defined as pad-free rates.
Positive surgical margin (PSM) was defined as
cancer at the inked margin in accordance with the
International Society of Uro-pathologists (ISUP)
definition.
References 1. Ficarra V, Novara G, Artibani W, et
al Retropubic, laparoscopic, and robot-assisted
radical prostatectomy a systematic review and
cumulative analysis of comparative studies. Eur
Urol. 200955(5)1037. 2. Herrmann TR, Rabenalt
R, Stolzenburg JU, et al Oncological and
functional results of open, robot-assisted and
laparoscopic radical prostatectomy does surgical
approach and surgical experience matter?
WorldJUrol. 200725(2)149. 3. Coelho RF, Chauhan
S, Palmer KJ, et al Robotic-assisted radical
prostatectomy a review of current outcomes. BJU
Int. 2009104 (10)1428.
By 6 weeks post-operatively 50 of
pre-operatively potent patients with bilateral
nerve-sparing (BNS) procedures had achieved
penetrative intercourse while at 1 year 83 were
potent.
Results A total of 152 patients had undergone LRP
with a median follow-up of 6 months. The median
age and BMI was 61 (44-74) years and 27 (20-37)
kg/m2 respectively. Median pre-operative PSA was
6.1 (0.7-30) ng/ml. Preoperative clinical stage
was cT1a (7), cT1c (42) and cT2 (51).
Sponsored by