MODELING THE INTERNAL DATA
1 / 1
Title:
MODELING THE INTERNAL DATA
Description:
Quantitative Human Pharmacology Modeling to Accelerate SGLT2i Drug Development G Nucci, A Ghosh, N Haddish-Berhane, P DaSilva-Jardine, J Trimmer, M Reed^ and CJ Musante –
Number of Views:133
Avg rating:3.0/5.0
Title: MODELING THE INTERNAL DATA
1
Quantitative Human Pharmacology Modeling to
Accelerate SGLT2i Drug Development G Nucci, A
Ghosh, N Haddish-Berhane, P DaSilva-Jardine, J
Trimmer, M Reed and CJ Musante Pfizer Global
Research Development, Pfizer Inc, Groton CT
06340 Entelos inc. Foster City, CA 94404
INTRODUCTION The sodium-glucose cotransporter 2
(SGLT2) is responsible for the majority of the
glucose reabsorption by the kidney1 and has been
recognized as a novel therapeutic approach for
improving glucose control in type 2 diabetes
mellitus (T2DM). Several selective SGLT2
inhibitors (SGLT2i) are currently under
development2,3. SGLT2 inhibition results in
increased urinary glucose excretion (UGE) in both
healthy subjects (HS)4,5 and subjects with
T2DM6,7,8 leading to reduced plasma glucose and
glycosylated hemoglobin (A1c) levels with the
additional benefit of a negative caloric balance,
thereby combining glucose control with weight
loss9,10. UGE provides a mechanistic biomarker
for the clinical assessment of SGLT2 inhibition.
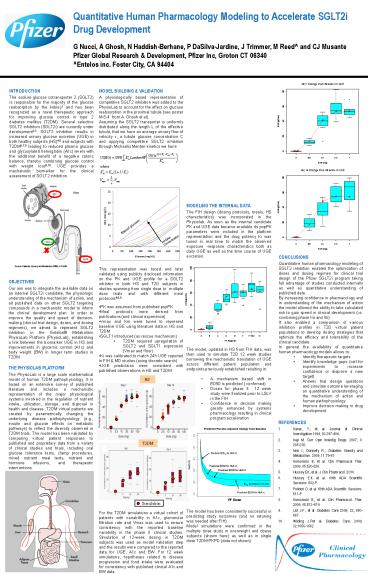
- MODEL BUILDING VALIDATION
- A physiologically based representation of
competitive SGLT2 inhibition was added to the
PhysioLab to account for the effect on glucose
reabsorption in the proximal tubule (see poster
M-5-4 from A. Ghosh et al). - Assuming the SGLT2 transporter is uniformly
distributed along the length L of the effective
tubule, that we have an average urinary flow of
velocity ?, a tubule glucose concentration C and
applying competitive SGLT2 inhibition through
Michaelis Menten kinetics we have
- MODELING THE INTERNAL DATA
- The FIH design (dosing protocols, meals, HS
characteristics) was incorporated in the
Physiolab. As soon as the internal candidate PK
and UGE data became available its popPK
parameters were included in the platform
representation and the drug potency Ki was tuned
in real time to match the observed exposure
-response characteristics both as daily UGE as
well as the time course of UGE excretion.
- CONCLUSIONS
- Quantitative human pharmacology modeling of SGLT2
inhibition enabled the optimization of doses and
dosing regimen for clinical trial design of the
Pfizer SGLT2i program taking full advantage of
studies conducted internally as well as
quantitative understanding of published data. - By increasing confidence in pharmacology and in
understanding of the mechanism of action the
model allowed the ability to take calculated risk
to gain speed in clinical development (i.e.
combining phase IIa and IIb) - It also enabled a comparison of various
inhibition profiles in T2D virtual patient
populations to develop dosing strategies that
optimize the efficacy and tolerability of the
clinical candidate. - In general the availability of quantitative human
pharmacology models allows to - Identify therapeutic targets
- Identify knowledge gaps (call for experiments to
increase confidence or disprove a new target) - Answer trial design questions and simulate
outcome leveraging on quantitative understanding
of the mechanism of action and human
pathophysiology - Improve decision making in drug development
OBJECTIVES Our aim was to integrate the available
data on an internal SGLT2i candidate, the
physiologic understanding of the mechanism of
action, and all published data on other SGLT2
targeting compounds in a mechanistic model to
inform the clinical development plan. In order to
improve the quality and speed of decision-making
(clinical trial design, doses, and dosing
regimens), we aimed to represent SGLT2 inhibition
in the Entelos Metabolism PhysioLab Platform
(PhysioLab), establishing a link between the
biomarker UGE in HS and improvements in glycemic
control (A1c) and body weight (BW) in longer term
studies in T2DM.
THE PHYSIOLAB PLATFORM The PhysioLab is a large
scale mathematical model of human T2DM
pathophysiology. It is based on an extensive
survey of published literature and includes a
mechanistic representation of the major
physiological systems involved in the regulation
of nutrient intake, utilization, storage, and
disposal in health and disease. T2DM virtual
patients are created by parametrically changing
the underlying disease pathophysiology (e.g.,
insulin and glucose effects on metabolic
pathways) to reflect the diversity observed in
T2DM trials. The model has been validated by
comparing virtual patient responses to published
and proprietary data from a variety of clinical
studies and trials, including oral glucose
tolerance tests, clamp procedures, mixed nutrient
meal tests, nutrient and hormone infusions, and
therapeutic interventions.
- REFERENCES
- Kanai, Y. et al. Journal of Clinical
Investigation 1994, 93397-404. - Isaji M. Curr Opin Investig Drugs. 2007 8
285-292. - Idris I. Donnelly R.. Diabetes Obesity and
Metabolism. 2009, 1179-88. - Komoroski B, et al. Clin Pharmacol Ther. 2009,
85520-526. - Hussey EK, et al. J Clin Pharmacol. 2010.
- Hussey E.K et al. 69th ADA Scientific Sessions.
582-P. - Polidori D. et al. 69th ADA Scientific Sessions.
511-P - Komoroski B., et al. Clin Pharmacol. Ther. 2009,
85513519 - List J.F. et al. Diabetes Care 2009, 32,
650-657. - Wilding J.Pet al. Diabetes Care. 2009,
321656-1662