Magnet Application - PowerPoint PPT Presentation
1 / 50
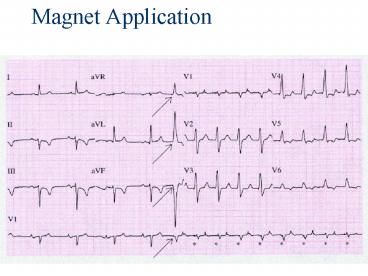
Title: Magnet Application
1
Magnet Application
2
Complications of Pacemaker Implantation
3
Complications of Pacemaker Implantation
- Venous access
- Infection
- Thrombophelbitis
- Pacemaker Syndrome
4
Venous Access
- Bleeding
- Pneumo / hemothorax
- Air embolism
5
Infection
- 2 for wound and pocket infection
- 1 for bacteremia with sepsis
- S. aureus and S. epidermidis
- If bacteremic start Vancomycin, remove system,
TV pacemaker and IV abx for 4-6 weeks, new system
6
Thrombophlebitis
- Incidence 30-50
- 1/3 have complete venous obstruction
- b/c of collateralization only 0.5-3.5 devp
symptoms - Swelling, pain, venous engorgement
- Heparin, lifetime warfarin
7
Pacemaker Syndrome
- Presents w/ worsening of original Sx post-implant
of single chamber pacer - AV asynchrony? retrograde VA conduction ? atrial
contraction against closed MV TV ? jugular
venous distention atrial dilation ? sx of CHF
and reflex vasodepressor effects - Dx of exclusion
- Tx w/ dual chamber pacer
8
Pacemaker syndrome
9
Pacemaker Malfunction
10
4 broad categories
- Failure to Output
- Failure to Capture
- Inappropriate sensing under or over
- Inappropriate pacemaker rate
11
Failure to Output
- absence of pacemaker spikes despite indication to
pace - dead battery
- fracture of pacemaker lead
- disconnection of lead from pulse generator unit
- Oversensing
- Cross-talk atrial output sensed by vent lead
12
No Output
- Pacemaker artifacts do not appear on the ECG
rate is less than the lower rate
Pacing output delivered no evidence of pacing
spike is seen
13
Failure to capture
- spikes not followed by a stimulus-induced complex
- change in endocardium ischemia, infarction,
hyperkalemia, class III antiarrhythmics
(amiodarone, bertylium)
14
Failure to sense or capture in VVI
15
A failure to capture atria in DDD
16
Inappropriate sensing Undersensing
- Pacemaker incorrectly misses an intrinsic
deoplarization ? paces despite intrinsic activity - Appearance of pacemaker spikes occurring earlier
than the programmed rate overpacing - may or may not be followed by paced complex
depends on timing with respect to refractory
period - AMI, progressive fibrosis, lead displacement,
fracture, poor contact with endocardium
17
Undersensing
- Pacemaker does not see the intrinsic beat, and
therefore does not respond appropriately
Scheduled pace delivered
Intrinsic beat not sensed
VVI / 60
18
Undersensing
- An intrinsic depolarization that is present, yet
not seen or sensed by the pacemaker
P-wavenot sensed
Atrial Undersensing
19
Inappropriate sensing Oversensing
- Detection of electrical activity not of cardiac
origin ? inhibition of pacing activity - underpacing
- pectoralis major myopotentials oversensed
- Electrocautery
- MRI alters pacemaker circuitry and results in
fixed-rate or asynchronous pacing - Cellular phone pacemaker inhibition,
asynchronous pacing
20
Oversensing
...though no activity is present
Marker channel shows intrinsic activity...
- An electrical signal other than the intended P or
R wave is detected
21
Inappropriate Pacemaker Rate
- Rare reentrant tachycardia seen w/ dual chamber
pacers - Premature atrial or vent contraction ? sensed by
atrial lead ? triggers vent contraction ?
retrograde VA conduction ? sensed by atrial lead
? triggers vent contraction ? etc etc etc - Tx Magnet application fixed rate, terminates
tachyarrthymia, - reprogram to decrease atrial sensing
22
Causes of Pacemaker Malfunction
- Circuitry or power source of pulse generator
- Pacemaker leads
- Interface between pacing electrode and myocardium
- Environmental factors interfering with normal
function
23
Pulse Generator
- Loose connections
- Similar to lead fracture
- Intermittent failure to sense or pace
- Migration
- Dissects along pectoral fascial plane
- Failure to pace
- Twiddlers syndrome
- Manipulation ? lead dislodgement
24
Twiddlers Syndrome
25
Twiddlers Syndrome
26
Leads
- Dislodgement or fracture (anytime)
- Incidence 2-3
- Failure to sense or pace
- Dx w/ CXR, lead impedance
- Insulation breaks
- Current leaks ? failure to capture
- Dx w/ measuring lead impedance (low)
27
Cardiac Perforation
- Early or late
- Usually well tolerated
- Asymptomatic ? incd pacing threshold, hiccups
- Dx P/E (hiccups, pericardial friction rub), CXR,
Echo
28
Environmental Factors Interfering with Sensing
- MRI
- Electrocautery
- Arc welding
- Lithotripsy
- Cell phones
- Microwaves
- Mypotentials from muscle
29
Management
30
Management History
- Most complications and malfunctions occur within
first few weeks or months - pacemaker identification card
- Syncope, near syncope, orthostatic dizziness,
lightheaded, dyspnea, palpitations - Pacemaker syndrome diagnosis of exclusion
31
Management Physical Exam
- Fever think pacemaker infection
- Cannon a waves AV asynchrony
- Bibasilar crackles if CHF
- Pericardial friction rub if perforation of RV
32
Management adjuncts
- CXR determine tip position
- ECG
33
Potential Problems Identifiable on an ECG Can
Generally Be Assigned to Five Categories
- Failure to output
- Failure to capture
- Undersensing
- Oversensing
- Pseudomalfunction
34
Pseudomalfunction Hysteresis
- Allows a lower rate between sensed events to
occur paced rate is higher
Hysteresis Rate 50 ppm
Lower Rate 70 ppm
35
Management ACLS
- Drug and Defibrillate as per ACLS guidelines
- However keep paddles gt10cm from pulse generator
- May transcutaneously pace
- Transvenous pacing may be inhibited by venous
thrombosis may need flouroscopic guidance
36
AMI Pacers
- Difficult Dx most sensitive indicator is ST-T
wave changes on serial ECG - If clinical presentation strongly suggestive then
should treat as AMI - Coarse VF may inhibit pacer (oversensing)
- Successful resuscitation may lead to failure to
capture (catecholamines, ischemia)
37
Disposition
38
Disposition
- Admit
- Pacemaker infections /unexplained fever or WBC
- Myocardial perforation
- Lead or dislodgement
- Wound dehiscence / extrusion or erosion
- Failure to pace, sense, or capture
- Ipsilateral venous thrombosis
- Unexplained syncope
- Twiddlers syndrome
39
Disposition
- Potentially fixable in ED w/ help
- Pacemaker syndrome
- Pacemaker-mediated tachycardia
- Cross-talk
- Oversensing
- Diaphragmatic pacing
- Myopotential inhibitors
40
Internal Cardiac Defibrillators
41
Internal Cardiac Defibrillators
- Device to treat tachydysrhythmias
- If ICD senses a vent rate gt programmed cut-off
rate of the ICD ? device performs
cardioversion/defibrillation - All ICDs are also vent pacemakers
- Required shock is approximately lt15 Joules
- Similar problems with implantation as pacemakers
42
Indications for ICD
- Cardiac arrest from VF or VT not due to
reversible etiology - Spontaneous sustained VT
- Syncope NYD inducible symptomatic VF or VT in
setting of poor drug tolerance or efficacy - Non-sustained VF or VT CAD, prior MI, LV
dysfunction and inducible VF or VT not responding
to Class I antiarrhythmic Tx
43
ICD Malfunction
- Inappropriate Cardioversion
- Ineffective Cardioversion
- Failure to Deliver Cardioversion
44
Inappropriate Cardioversion
- Most frequently associated problem
- Sensing malfunction SVT sensed as VT
- Shocks for nonsustained VT
- T waves detected as QRS complex and interpreted
as ? HR - h/r Could be ? incidence of VT, VF (hypoK,
hypoMg, ischemia /- infarction)
45
Ineffective Cardioversion
- Inadequate energy output
- Rise in defibrillation threshold ?
antiarrhythmics - MI at lead site
- Lead fracture
- Dislodgement of leads
46
Failure to Deliver Cardioversion
- Failure to sense
- Lead fracture
- Electromagnetic interference
- Inadvertent deactivation
47
ACLS Interventions
- ICD may not prevent sudden cardiac death
- Same approach as with pacemakers
- Person performing CPR may feel a mild shock if
ICD discharges during compressions - Can deactivate device with magnet during
resuscitation efforts
48
Disposition
- in almost all instances, admission to a
monitored setting with extended telemetric
observation will be necessary - Rosens
49
Thanks to
- Calgary Health Region Pacemaker nurses
- Karen and Sandra
50
References
- Brady et al. 1998. EM Clinics NA. 16(2) 361-388
- Xie et al. 1998. Em Clinics NA. 16(2) 419-462
- Shah et al. 1998 EM Clinics NA. 16(2) 463-487
- Harrigan and Brady. 2000. EMR 21(19) 205-216
- Rosen
- American College of Cardiology ECG of the Month
Feb 2001 http//www.acc.org/education/online/ecg
_month/0201/Feb01_02.htm - Pacemaker and Automatic Internal Cardiac
Defibrillator, Weinberger et. al
http//www.emedicine.com/emerg/topic805.htm - CorePace presentation 99912 by Medtronic Inc.
2000 available from Pacmaker Nurses at Foothills
Hospital, www.medtronic.com