Conditions of the Lymph System - PowerPoint PPT Presentation
1 / 47
Title:
Conditions of the Lymph System
Description:
Lymphedema does not respond significantly to overnight elevation, whereas edema secondary to central organ failure or venous insufficiency does. – PowerPoint PPT presentation
Number of Views:363
Avg rating:3.0/5.0
Title: Conditions of the Lymph System
1
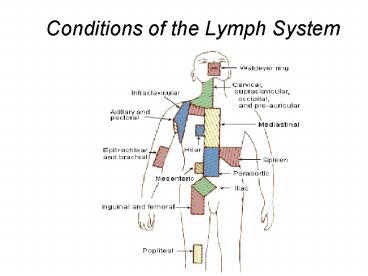
Conditions of the Lymph System
2
Anatomy of head neck lymph nodes
3
Anatomy of axillary lymph nodes
4
Anatomy of inguinal lymph nodes
5
- Generalized adenopathy has been defined as
- involvement of three or more
noncontiguous lymph node areas.
6
CAUSES OF LYMPHADENOPATHY
- Infection
- Bacterial (e.g., all pyogenic bacteria,
cat-scratch disease, syphilis) - Mycobacterial (e.g., tuberculosis, leprosy)
- Fungal (e.g., histoplasmosis )
- Chlamydial (e.g., lymphogranuloma venereum)
- Parasitic (e.g., toxoplasmosis, filariasis)
- Viral (e.g., Epstein-Barr virus, cytomegalovirus,
rubella, HIV) - Benign disorders of the immune system (e.g.,
rheumatoid arthritis, SLE) - Malignant disorders of the immune system (e.g.,
chronic and acute myeloid and lymphoid leukemia,
non-Hodgkin's lymphoma, Hodgkin's disease,
angioimmunoblastic-like T-cell lymphoma, multiple
myeloma with amyloidosis, malignant
histiocytosis) - Other malignancies (e.g., breast carcinoma, lung
carcinoma, melanoma, head and neck cancer,
gastrointestinal malignancies, germ cell tumors,
Kaposi's sarcoma) - Storage diseases (e.g., Gaucher's disease)
7
Acute lymphadenitis
- It is painful
- Localizing symptoms suggest infection in
specific site( primary focus ) - Constitutional symptoms may be present e.g.
Fever, malaise - Treatment is directed to the cause ,antibiotics,
derange if abscess occur
8
Chronic non specific lymphadenitis
- Mild recurrent lymphadenitis
- Common sites are upper deep cervical LN and
inguinal - Chronic enlargement of affected LN, which is firm
slightly tender and mobile - Primary focus is there
- Treatment is directed to the cause
9
Specific lymphadenitis
- Bacterial (cat-scratch disease, syphilis)
- Mycobacterial (e.g., tuberculosis, leprosy)
- Fungal (e.g., histoplasmosis, coccidioidomycosis)
- Chlamydial (e.g., lymphogranuloma venereum)
- Parasitic (e.g., toxoplasmosis, filariasis)
- Viral (e.g., Epstein-Barr virus, cytomegalovirus,
HIV)
10
HIV- related.Persistent Generalized
Lymphadenopathy (PGL)
- Lymph nodes larger than 1.5 cm in diameter in 2
or more extrainguinal sites of 3 or more months
duration - Nodes are non-tender, symmetrical, and often
involve the posterior cervical, axillary,
occipital, and epitrochlear nodes - Develops in up to 50 of HIV-infected individuals
- Up to one-third do not have any other symptom on
presentation (stage 1) - In HIV-positive patients, PGL is a clinical
diagnosis. - PGL may slowly regress during the course of HIV
infection and may disappear before the onset of
AIDS
11
Tuberculosis lymphadenopathy
- Cervical nodes most commonly involved
- Organism
- Root lymph Vs blood
- Predisposing factors are immunocompromised
patients - Usual course of lymph born disease is as
follows - Firm, discrete nodes?Matted together and adherent
to the surrounding ?Fluctuant nodes , non tender
abscesses, chronic sinuses ( with dusky red skin
over and undermined edge ) - Anorexia ,night fever, night sweating, loss
of weight - Fluctuant cervical nodes that develop over
weeks to months without significant inflammation
or tenderness suggest infection with M.
tuberculosis, atypical mycobacterium, or scratch
disease - Blood born usually occur in adult with more
than one group of LN which are firm, mobile and
discrete - CBC,CXR and positive smears for acid-fast bacilli
- PCR
- Fine-needle aspiration of the involved lymph node
spiral - In smear-negative pulmonary TB, it is
worthwhile aspirating extra-thoracic lymph nodes
to confirm diagnosis of TB (80 positive) - Treatment
- Anti tuberclus drugs, good diet, correct immune
deficiency - Aspiration of abscess
12
syphilis
- Clinical Symptoms may evolve
- Generalized painless lymphadenopathy
- Maculo-papular, papular, or pustular rash on
entire body, especially on palms and soles - Highly infectious lesions on mucous membranes
(lips, mouth, pharynx, vulva, glans penis) which
are silvery grey superficial erosions with a red
halo and not painful unless there is a secondary
infection. - 40 of these patients will have CNS involvement
with headache and meningismus - 1-2 will develop acute aseptic meningitis
- benzathine penicillin 2.4 million units IM single
dose
13
Lymphoma
- Lymphoma is a malignant disease that affects
blood cells called lymphocytes immune cells
that normally protect you from illness. - Damage to genes in these cells can sometimes lead
to abnormal cell behavior which makes the cells
immortal unable to die when they should or
causes sustained rapid cell division.. - These malignant cells then may accumulate to form
tumors that enlarge the lymph nodes or spread to
other areas of the lymphatic system, such as the
spleen or bone marrow, or outside the lymphatic
system to the skin, or mucosal linings of the
stomach. - They arise as the result of abnormal
proliferation of the lymphoid system, and hence
occur at any site where lymphoid tissue is found.
Most commonly they are manifest by the
development of lymphadenopathy at single or
multiple sites, although primary extranodal
presentations account for up to 20 of
non-Hodgkin's lymphoma. - The prognosis is determined by the specific
subtype of lymphoma and the anatomical extent of
disease and its bulk, the clinical course ranging
from months to years. - Lymphomas are currently classified on the basis
of histological appearance into - Hodgkin's
lymphoma - non-Hodgkin's
lymphoma. - The two types not only have different morphologic
characteristics but differ also in their clinical
behavior and their response to various
therapeutic regimens.
14
(No Transcript)
15
HODGKIN'S LYMPHOMA (HL)
- Aetiology
- There is epidemiological evidence linking
previous infective mononucleosis with HL and up
to 40 of patients with HL have increased EBV
antibody titres at the time of diagnosis and
several years prior to the clinical development
of HL. - Other environmental and occupational exposure to
pathogens have been postulated. - ?? Chronic infection,?? Depressed immunity,??
Chemical exposure pesticides,cancer therapies,
herbicides ,?? Viral exposures - Pathology
- The hallmark of HL is the Reed-Sternberg cell)
which is usually derived from germinal centre B
cells or, rarely, peripheral T cells. - Pathological classification of Hodgkin's lymphoma
- Nodular lymphocyte-predominant Hodgkin's
lymphoma - Classical Hodgkin's lymphoma
- Nodular sclerosis HL(young females,
involving particularly lymph nodes in the
mediastinum and neck ). - Lymphocyte-rich HL(It often occurs in
peripheral lymph nodes. It is often an indolent
disease(. - Mixed cellularity HL) more common in
men and is associated with B symptoms ( - Lymphocyte-depleted HL) It is seen in
HL associated with HIV (
16
Clinical features
- Lymph node enlargement, most often of the
cervical nodes (other causes are shown in, these
are usually painless and with a rubbery
consistency. - Enlargement of the spleen/liver.
- 'B' symptoms fever, (25) drenching night
sweats, weight loss of gt 10 bodyweight - Other constitutional symptoms, such as pruritus,
fatigue, anorexia and, occasionally,
alcohol-induced pain at the site of enlarged
lymph nodes. - Symptoms due to involvement of other organs (e.g.
lung - cough and breathlessness (
17
Investigations
- Blood count may be normal, or there can be a
normochromic, normocytic anaemia. Lymphopenia and
occasionally eosinophilia are present. - Erythrocyte sedimentation rate )ESR) is usually
raised and is an indicator of disease activity. - Liver biochemistry is often abnormal, with or
without liver involvement. - Serum lactate dehydrogenase raised level is
adverse prognostic factor. - Chest X-ray may show mediastinal widening, with
or without lung involvement. - CT scans show involvement of intrathoracic nodes
in 70 of cases. Abdominal or pelvic lymph nodes
are also found. It is the investigation of choice
for staging although PET scanning is increasingly
being used. - Lymph node biopsy is required for a definitive
diagnosis
18
Cotswolds modification of Ann Arbor staging
classification
- Stage I Involvement of a single lymph-node region
or lymphoid structure (e.g. spleen, thymus,
Waldeyer's ring) or involvement of a single
extralymphatic site - Stage II Involvement of two or more lymph-node
regions on the same side of the diaphragm (hilar
nodes, when involved on both sides, constitute
stage II disease) localized contiguous
involvement of only one extranodal organ or site
and lymph-node region(s) on the same side of the
diaphragm (IIE). The number of anatomic regions
involved should be indicated by a subscript (e.g.
II3) - Stage III Involvement of lymph-node regions on
both sides of the diaphragm (III), which may also
be accompanied by involvement of the spleen
(IIIS) or by localized involvement of only one
extranodal organ site (IIIE) or both
(IIISE)III1With or without involvement of
splenic, hilar, coeliac, or portal nodesIII2With
involvement of para-aortic, iliac, and mesenteric
nodes - Stage IV Diffuse or disseminated involvement of
one or more extranodal organs or tissues, with or
without associated lymph-node involvement - Designations applicable to any disease state
- A No symptoms
- B Fever (temperature gt 38C), drenching
night sweats, unexplained loss of more than 10
of body weight within the previous 6 months - X Bulky disease (a widening of the
mediastinum by more than one-third of the
presence of a nodal mass with a maximal dimension
greater than 10 cm) - E Involvement of a single extranodal site
that is contiguous or proximal to the known nodal
site
19
Treatment
- Specific treatment is based otherwise on the
anatomical distribution of disease, its 'bulk'
and the presence or absence of 'B' symptoms - 'Early stage' (IA, IIA no bulk) The treatment
of choice now is brief chemotherapy followed by
involved field irradiation. - Advanced disease Cyclical combination
chemotherapy with or without irradiation to sites
of 'bulk' disease is the treatment of choice for
all these patients.
20
NON-HODGKIN'S LYMPHOMA (NHL)
- These are malignant tumours of the lymphoid
system classified separately from Hodgkin's
lymphoma. Most (70) are of B cell origin
although T cell tumours are increasingly being
recognized. - NHL is associated with the EBV virus (Burkitt's
lymphoma) and the human T cell lymphotropic virus
which is prevalent in Japan, Africa, South
America and the Caribbean. Herpes virus 8 is
associated with primary effusion lymphomas and
Castleman's disease there is an increase in
lymphoma in patients with AIDS. Helicobacter
pylori is an aetiological factor in gastric
lymphoma. - Lymphomas also occur in congenital
immunodeficiency, post-transplantation and in
autosomal family cancer syndromes . - Other causes, e.g. occupation, dietary and
exposure to chemicals, have been linked to the
increasing incidence but the evidence is
unconfirmed
21
Types
- Follicular
- Lymphoplasmacytict
- Mantle cell
- Diffuse large B cell
- Burkitts
- Anaplastic
- MALT (mucosal associated lymphoid tissue)
22
WHO classification of lymphoid neoplasms
- B cell lymphomas
- Precursor B cell lymphoma Precursor B
lymphoblastic lymphoma/leukaemia (highly
(aggressive) - Mature B cell lymphoma
- Chronic lymphocytic leukaemia/small
lymphocytic lymphomaLymphoplasmacytic
lymphomaSplenic marginal zone lymphomaExtranodal
marginal zone B cell lymphoma of
mucosa-associated lymphoid tissue
(MALT-lymphom)Nodal marginal zone B cell
lymphomaFollicular lymphoma((aggressive)Mantle
cell lymphomaDiffuse large B cell lymphoma)
aggressiv)Mediastinal (thymic) large B cell
lymphomaIntravascular large B cell
lymphomaPrimary effusion lymphomaBurkitt's
lymphoma/leukaemia (highly aggressive) - T/NK cell lymphomas
- Precursor T cell lymphoma
- Precursor T cell lymphoblastic
leukaemia/lymphoma(highly aggressive) - Blastic NK cell lymphoma
- Mature T/NK cell lymphoma
- Adult T cell leukaemia/lymphoma(very
aggressive(Extranodal NK/T cell lymphoma, nasal
typeEnteropathy-type T cell lymphomaHepatospleni
c T cell lymphomaSubcutaneous panniculitis-like
T cell lymphomaMycosis fungoidesSézary
syndromePrimary cutaneous anaplastic large cell
lymphomaPeripheral T cell lymphoma, unspecified
(aggressive)Angioimmunoblastic T cell
lymphomaAnaplastic large cell lymphoma
(aggressive)
23
Treatment options
- Aggressive combination chemotherapy gives high
complete remission rates and molecular remission.
- Antibody therapy. The monoclonal antibody
rituximab induces remission (partial) in 30-70
of patients, almost without toxicity. Molecular
remissions are observed. Complications include
the cytokine release syndrome, with fever,
vomiting and allergic reactions (angio-oedema,
bronchospasm and dyspnoea). - Rituximab/chemotherapy combination. These have
now been reported to improve the complete
remission rate (with disappearance of Bcl-2
positive cells from the bone marrow in 100 of
patients), freedom from progression and
event-free survival, even though there is (as
yet) no effect on overall survival. This may
become the standard therapy for CD20 positive
lymphoma. - Antibody-targeted irradiation.
24
Clinical approach
- A careful history
- , -Age of the patient.
- -The occurrence of fever, sweats, or
weight loss - Site of infection, a particular medication, a
travel history, or a previous malignancy. - physical examination
- localized or generalized
- size of nodes
- Texture
- Mobility
- presence or absence of nodal tenderness
- signs of inflammation over the node
- skin lesions
- splenomegaly
- Imaging
- Chest radiography
- Ultrasonography
- Computed tomography
- Magnetic resonance imaging
- Positron emission tomography
25
The Lymphatics
26
Lymphedema
- Lymphedema is the result of an inability of the
existing lymphatic system to accommodate the
protein and fluid entering the interstitial
compartment at the tissue level. In the first
stage of lymphedema, impaired lymphatic drainage
results in protein-rich fluid accumulation in the
interstitial compartment. Clinically, this
manifests as soft pitting edema. - In the second stage of lymphedema, the clinical
condition is further exacerbated by accumulation
of fibroblasts, adipocytes, and, perhaps most
importantly, macrophages in the affected tissues,
which culminate in a local inflammatory response.
This results in important structural changes from
the deposition of connective tissue and adipose
elements at the skin and subcutaneous level. In
the second stage of lymphedema, tissue edema is
more pronounced, is nonpitting, and has a spongy
consistency. - In the third and most advanced stage of
lymphedema, the affected tissues sustain further
injury as a result of both the local inflammatory
response as well as recurrent infectious episodes
that typically result from minimal subclinical
skin breaks in the skin. Such repeated episodes
injure the incompetent, remaining lymphatic
channels, progressively worsening the underlying
insufficiency of the lymphatic system. This
eventually results in excessive subcutaneous
fibrosis and scarring with associated severe skin
changes characteristic of lymphostatic
elephantiasis
27
Clinical picture
- The edematous limb has a firm and hardened
consistency. - There is loss of the normal perimalleolar shape,
resulting in a tree trunk pattern. - The dorsum of the foot is characteristically
swollen, resulting in the appearance of the
buffalo hump, and the toes become thick and
squared . - In advanced lymphedema, the skin undergoes
characteristic changes, such as lichenification,
development of peau dorange, and
hyperkeratosis.Additionally, the patients give a
history of recurrent episodes of cellulitis and
lymphangitis after trivial trauma and frequently
present with fungal infections affecting the
forefoot and toes. - Patients with isolated lymphedema usually do not
have the hyperpigmentation or ulceration one
typically sees in patients with chronic venous
insufficiency. - Lymphedema does not respond significantly to
overnight elevation, whereas edema secondary to
central organ failure or venous insufficiency
does.
28
Differential Diagnosis
- The most common causes of bilateral extremity
edema are of systemic origin. The most common
etiology is cardiac failure, followed by renal
failure. Hypoproteinemia secondary to cirrhosis,
nephrotic syndrome, and malnutrition can also
produce bilateral lower extremity edema. - Another important cause to consider with
bilateral leg enlargement is lipedema. Lipedema
is not true edema but rather excessive
subcutaneous fat found in obese women. It is
bilateral, nonpitting, and greatest at the ankle
and legs, with characteristic sparing of the
feet. There are no skin changes,and the
enlargement is not affected by elevation. The
history usually indicates that this has been a
lifelong problem that runs in the family. - Once the systemic causes of edema are excluded,
in the patient with unilateral extremity
involvement, edema secondary to venous and
lymphatic pathology should be entertained. The
edema responds promptly to overnight leg
elevation. In the later stages, the skin is
atrophic with brawny pigmentation. Ulceration
associated with venous insufficiency occurs above
or posterior and beneath the malleoli.
29
CLASSIFICATION of lymph- edema
- Lymphedema is generally classified as primary
when there is no known etiology and secondary
when its cause is a known disease or disorder. - Primary lymphedema has generally been classified
on the basis of the age at onset and presence of
familial clustering. - Primary lymphedema with onset before the first
year of life is called congenital. The familial
version of congenital lymphedema is known as
Milroys disease and is inherited as a dominant
trait. - Primary lymphedema with onset between the ages of
1 and 35 years is called lymphedema praecox. The
familial version of lymphedema praecox is known
as Meiges disease. - Finally, primary lymphedema with onset after the
age of 35 is called lymphedema tarda. - Worldwide the most common cause of secondary
lymphedema is infestation of the lymph nodes by
the parasite Wuchereria bancrofti in the disease
state called filariasis. In the developed
countries the most common causes of secondary
lymphedema involve resection or ablation of
regional lymph nodes by surgery, radiation
therapy, tumor invasion, direct trauma, or, less
commonly, an infectious process.
30
Investigation
- The diagnosis of lymphedema is relatively easy in
the patient who presents in the second and third
stages of the disease. It can however, be a
difficult diagnosis to make in the first stage,
particularly when the edema is mild, pitting, and
relieved with simple maneuvers such as elevation.
For patients with suspected secondary forms of
lymphedema, computed tomography (CT) and magnetic
resonance imaging (MRI) are valuable and indeed
essential for exclusion of underlying oncologic
disease - In patients with known lymph node excision and
radiation treatment as the underlying problem of
their lymphedema, additional diagnostic studies
are rarely needed except as these studies relate
to follow-up of an underlying malignancy. - For patients with edema of unknown etiology and a
suspicion for lymphedema, lymphoscintigraphy is
the diagnostic test of choice. - When lymphoscintigraphy confirms that lymphatic
drainage is delayed, the diagnosis of primary
lymphedema should never be made until neoplasia
involving the regional and central lymphatic
drainage of the limb has been excluded through CT
or MRI. - If a more detailed diagnostic interpretation of
lymphatic channels is needed for operative
planning, then contrast lymphangiography may be
considered.
31
THERAPY
- The large majority of lymphedema patients can be
treated with a combination of limb elevation, a
high-quality compression garment, complex
decongestive physical therapy, and compression
pump therapy. - Operative treatment may be considered for
patients with advanced complicated lymphedema
that fail management with nonoperative means.
32
Neck lump
33
pleomorphic adenomaof parroted gland
34
(No Transcript)
35
Multiple cervical metastases visible in the nodal
basins that drain the site of the primary
malignancy
36
Ludwigs angina
37
Ranula
38
Virchows lymph node
39
Branchial cyst
40
Thyroglossal cyst
41
Cystic Hygroma
42
(No Transcript)
43
(No Transcript)
44
Neck lumpThyroid, lymph node ,carotid ,salivary
gland , sternomastoid muscle
- Goitre.
- Neoplasm
- Thyroid neoplasms
- Metastatic carcinoma.
- Primary lymphoma.
- Salivary gland tumour.
- Sternocleidomastoid tumour.
- Carotid body tumour.
- Inflammatory
- Acute infective adenopathy.
- Collar stud abscess.
- Parotitis.,submandibular sialadinitis
- Congenital
- Thyroglossal duct cyst.
- Cystic hygroma.
- Branchial cyst.
- Dermoid cyst.
- Torticollis.
- Vascular
- .Caroted body tumors
- Subclavian aneurysm.
- Subclavian ectasia.
45
Children
- Congenital and inflammatory lesions are common.
- Cystic hygroma in infants, base of the neck,
brilliant transillumination. - Thyroglossal or dermoid cyst midline,
discrete, elevates with - tongue protrusion.
- Torticollis rock-hard mass, more prominent
with head flexed, - associated with fixed rotation (a fibrous mass in
the sternocleidomastoid muscle). - Branchial cyst anterior to the upper third of
the sternocleidomastoid. - Viral/bacterial adenitis usually affects
jugular nodes, multiple, - tender masses.
- Neoplasms (lymphoma most common).
46
Young adults
- Inflammatory neck masses and thyroid malignancy
are common. - Viral (e.g. infectious mononucleosis) or
bacterial (tonsillitis/pharyngitis) adenitis. - Papillary thyroid cancer isolated, non-tender,
thyroid mass, possible lymphadenopathy.
47
Older age group
- Neck lumps are malignant until proven otherwise.
- Metastatic lymphadenopathy multiple, hard,
nontender, tendency to be fixed. - 75 in primary head and neck (thyroid,
nasopharynx, tonsils, larynx, pharynx), 25 from
infraclavicular primary (stomach, pancreas,
lung). - Primary lymphadenopathy (thyroid, lymphoma)
fleshy,rubbery, large size. - Primary neoplasm (thyroid, salivary tumour)
firm, nontender, fixed to tissue of origin.