Case - PowerPoint PPT Presentation
1 / 42
Title: Case
1
Case
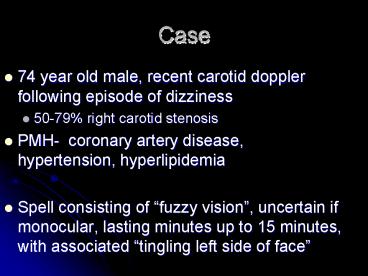
- 74 year old male, recent carotid doppler
following episode of dizziness - 50-79 right carotid stenosis
- PMH- coronary artery disease, hypertension,
hyperlipidemia - Spell consisting of fuzzy vision, uncertain if
monocular, lasting minutes up to 15 minutes, with
associated tingling left side of face
2
Questions
- Is this amaurosis fugax?
- What is this patients risk for stroke?
- Is carotid endarterectomy indicated in this case?
3
Amaurosis Fugax
- and the role of
- Carotid Endarterectomy
COL Beverly Rice Scott MD Neurology and
Neuro-ophthalmology Madigan Army Medical Center
4
Outline
- Definition and etiologies of transient visual
loss - Clinical features pathophysiology
- Evaluation of transient monocular blindness
- Amaurosis Fugax and Stroke Risk
- North American Symptomatic Carotid Endarterectomy
Trial (NASCET) - Spectrum of ocular ischemic syndromes and stroke
risk
5
Definition
- Painless unilateral transient loss of vision,
partial or complete, related to retinal arterial
microembolization or hypoperfusion - fleeting darkness or blindness
- Retinal transient ischemic attack (RTIA)
- transient monocular blindness (TMB)
- Accounts for 25 of anterior circulation
transient ischemic attacks (TIAs).
6
Transient visual loss
Monocular (TMB)
Binocular
Amaurosis Fugax
Cortical Migraine
Heart disease
Transient Visual Obscuration
Retinal Migraine
Arteritis
7
EtiologiesTransient visual loss
- Occlusive retinal artery disease
- Atheroembolic, cardioembolic, arteritic,
hematological disorders, congenital, orbital
tumor - Low retinal artery pressure
- Ocular ischemia syndrome, arteriovenous fistula,
congestive heart failure, anemia - Optic disc disease and anomalies
- Papilledema, Glaucoma, Drusen
- Vasospasm (ophthalmic migraine)
- Miscellaneous
- Uhthoffs phenomenon, classic migraine
8
Clinical FeaturesSymptoms
- Abrupt or gradual monocular visual loss,
progressing from peripheral toward center of
field - /- descending/ ascending shade, partial or
complete - looking through fog
- Visual disturbance Dark, foggy, gray, white
- Minutes (1-5 minutes, occasionally longer)
full resolution takes 10-20 minutes - Painless
- Stereotyped
- Usually occurs in isolation
- may be difficult to distinguish monocular from
binocular visual loss
9
Clinical FeaturesRetinal findings
- Transient retinal ischemia
- Often normal
- boxcar-ing (segmentation of blood columns
resulting from stasis) - Engorgement of veins
- Swelling of retina
- Retinal embolus
10
Clinical features Retinal findings
- Acute infarction
- Opaque and gray (early)
- bright plaques of cholesterol or other
microemboli may persist weeks to years - Cotton-wool spot
- Segmental arteriolar mural opacification
- Optic disc pallor, arteriolar narrowing (late)
11
Hollenhorst Plaque
Retina and Vitreous, Basic and Clinical Science
Course, AAO 1996
12
Cotton-wool Spot
Retina and Vitreous, Basic and Clinical Science
Course, AAO 1996
13
Pathophysiology
- Atheromatous degeneration and stenosis of the
cervical carotid arteries - Estimated 27 - 67 w/ amaurosis or retinal
strokes - Retinal emboli
- Cholesterol crystals
- Platelet aggregates
- Fibrin and blood cells
- Neutral fat
- Vasospasm
- Primary thrombosis of retinal arteries does not
occur
14
Pathophysiology
- Microemboli occludes retinal vessels, then
fragment and pass into retinal periphery - If disaggregation with reconstitution of blood
flow does not occur, ischemic damage to the inner
retinal layers may be irreversible
15
Branch Retinal Artery Occlusion
Retina and Vitreous, Basic and Clinical Science
Course, AAO 1996
16
Evaluation Transient Monocular Blindness
- Consider disorders with greatest morbidity and
most common disorders - Consider age, stereotypy of events
- Physical exam (blood pressure, carotid/cardiac
exam) - Ophthalmologic Exam
- Visual acuity, visual fields, relative afferent
pupil defect - dilated fundus exam (emboli, anomalous discs)
- Visual fields
- Electroretinogram diminished B-wave amplitude
17
Evaluation Transient Monocular Blindness
- Over age 40
- History for giant cell arteritis, polymyalgia,
coronary artery disease, stroke risk
factors - ESR, Creactive Protein if older than 50)
- Carotid Doppler
- Echocardiogram w/ bubble
- MRA , CT angiography
- Fluorescein angiogram
- Carotid angiography
- Under age 40
- Migraine history, family
- Echocardiogram w/ bubble
- CBC, ESR, ANA, antiphospholipid antibodies
- stop birth control pill
- stop smoking
18
Cerebrovascular disease
- A spectrum of signs, symptoms,
and stroke risks
Low risk
High risk
Asymptomatic w/ signs of atherosclerotic Cerebrova
scular disease
Symptomatic Atherosclerotic Cerebrovascular disea
se
Asymptomatic
19
Amaurosis Fugax and Stroke Risk
- Isnt if funny that I went blind
- in the wrong eye
- CM Fisher. Transient monocular blindness
associated with hemiplegia. Archives
Ophthalmology, 1952. - What is the relationship of AF and the other
ocular ischemic syndromes to the - carotid arteries?
20
Amaurosis Fugax (AF) Stroke Risk
- Early studies and reports uncontrolled
- Different populations
- Causes aggregated
- Best studied ocular ischemic syndrome
- Prognosis following AF considered more favorable
than TIA, unless severe stenosis - Prognosis altered by carotid endarterectomy?
- Stroke risk estimated 2-4 prior to NASCET
21
Carotid Endarterectomy (CEA)Historical
Perspective
- 1954 CEA introduced
- 1959-70 Joint Study of Extracranial Arterial
Occlusion - surgery 32 stroke risk
- medical 39 stroke risk
- operative MM of 11.4
- CEA benefit if 3 morbidity
- 1970 15,000 operations/yr
- 1980s 100,000 operations/yr
Practical Neurology, Vol 4, 2005.
22
NASCET 1987-1996
- North American Symptomatic Carotid Endarterectomy
Trial (NASCET) - 2885 patients enrolled TIA/stroke 120 days
- 1583 patients(54.9) -- TIA
- 1302 patients (45) nondisabling stroke
- carotid stenosis angio confirmed
- moderate (30-69) severe (70-99)
- Established CEA over medical RX in patients with
high grade stenosis (gt70)
23
NASCET
Cumulative risk for ipsilateral stroke in
symptomatic Carotid Endarterectomy trials at 2
years
lt 50 , CEA not better than ASA (aspirin)
24
NASCETAmaurosis Stroke Risk
- The Risk of Stroke in Patients With First-Ever
Retinal vs Hemispheric Transient Ischemic Attacks
and High-grade Carotid Stenosis. Archives of
Neurology. 1995. - Prognosis after Transient Monocular Blindness
Associated with Carotid-Artery Stenosis. NEJM.
2001
25
NASCET Medical Subgroup High grade stenosis
- 129 patients with first TIA
- 59 retinal TIAs (RTIAs)
- 70 with hemispheric TIAs (HTIAs)
- Characterize the features and course of subgroups
with high grade stenosis - Compare outcomes with RTIAs to HTIAs
- Average follow-up 19months
Arch Neurol. 1995 52
26
NASCET Medical SubgroupHigh Grade Stenosis
- HTIAs older, higher risk factors
- RTIAs higher risk for smoking
- Longer delay for medical treatment for RTIAs
(48 days vs 15.2 days ) - Estimates for stroke risk at 2 years
- RTIAs 16.6 /- 5.5
- HTIAs 43.5 /- 6.7
Arch Neurol. 1995 52
27
NASCET Medical Subgroup Risk Factors w/ High
Grade Stenosis
28
NASCET Medical Subgroup Outcomes w/ High Grade
Stenosis
Arch Neurol. 1995 52
29
NASCET Surgical Subgroup Outcomes
- 328 surgically treated patients
- 5.8 perioperative stroke
- 9 2 year stroke rate
- 54 surgical treated patients with RTIA
- 2 minor perioperative strokes (4)
- One stroke (2) 17 months post-op
- 6.8 stroke risk at 2 years
30
NASCETAmaurosis Stroke Risk
- The Risk of Stroke in Patients With First-Ever
Retinal vs Hemispheric Transient Ischemic Attacks
and High-grade Carotid Stenosis. Archives of
Neurology. 1995. - Prognosis after Transient Monocular Blindness
Associated with Carotid-Artery Stenosis. NEJM.
2001
31
NASCET SubgroupsPrognosis of TMB (transient
monocular blindness)
- Compared 397 patients with isolated TMB (medical
and surgical subgroups) to 829 patients with
hemispheric TIAs - Compared stroke risk for TMB and HTIAs in
patients with high grade stenosis with and
without collaterals - Identified risk factors for ipsilateral stroke in
patients with carotid stenosis gt 50 -
32
NASCET SubgroupsPrognosis of TMB
- HTIAs older, higher risk factors
- TMB higher risk for smoking, increased high
grade stenosis, higher incidence of collaterals - Medically treated TMB had 3 year ipsilateral
stroke risk approx ½ HTIA - Surgically treated TMB showed 30-day stroke rate
½ of HTIA (3.6 vs 7.4) - Stroke risk increased with degree of carotid
stenosis and specific stroke risk factors -
33
NASCET Med/Surg SubgroupsIsolated TMB vs TIA
NEJM. Vol 345,2001
34
NASCET Med/Surg SubgroupsIsolated TMB vs TIA
Collateral circulation filling of the ACA,
PComA, or ophthalmic artery
NEJM. Vol 345,2001
35
NASCET Med/Surg SubgroupsThree year stroke risk
36
NASCET Medical SubgroupsCollaterals 3 year
stroke risk
- TMB w/ collaterals (N25) 2.9
- HTIAs w/ collaterals (N30) 16.7
- TMB w/o collaterals (N44) 16.0
- HTIAs w/o collaterals (N69) 44.4
NEJM. Vol 345,2001
37
NASCET Med/surg Subgroup Isolated TMB (N397)
- Median of TMB episodes 3 (1-7)
- 5 had gt45 episodes
- Median duration 4 minutes (1-10min)
- 5 had episode gt 60min
- No correlation to carotid stenosis
- 3 year stroke risk (N 198, medical)
- 1 episode -- 10.4
- gt2 episodes-- 8.2
NEJM. Vol 345,2001
38
NASCET Medical Subgroup Stroke Risk Factors
- TMB with gt 50 stenosis
- Age gt 75
- Male sex
- h/o hemispheric TIA or stroke
- h/o intermittent claudication
- Ipsilateral stenosis 80-94
- No collaterals on angiography
NEJM. Vol 345,2001
39
Amaurosis Fugax Stroke RiskNASCET findings
- TMB has high stroke risk if high grade carotid
stenosis, though less than HTIAs - Higher collaterals improve prognosis
- Age, gender, h/o stroke/TIA, claudication may
alter stroke risk - CEA reduces stroke risk if surgeon has low
complication rate - Perioperative risk for stroke and death was lower
in patients with TMB
40
Spectrum of clinical stroke risk
Low risk
High risk
Amaurosis Fugax (2 -?6)
Minor Stroke (6.1)
Asymptomatic Stenosis (2)
BRAO
TIA (3.7)
Major Stroke (9)
Asymptomatic Bruit (2)
Asymptomatic retinal emboli
Acute Chronic Ocular Ischemic Syndrome
AION
Estimated Annual Stroke Rates
41
Conclusions
- Amaurosis Fugax is caused by ischemia to the
retina, often associated with carotid stenosis,
and is a risk factor for stroke - Prognosis is better for patients with amaurosis
fugax treated both medically and surgically
compared to patients with hemispheric TIAs. - Amaurosis Fugax should be recognized, with strong
consideration for carotid endarterectomy with
high grade carotid stenosis, vascular risk
factors present, and low complication rate of
procedure in your center
42
References
- Benavente, et al. Prognosis after Transient
Monocular Blindness Associated with Carotid
Artery Stenosis. NEJM, Vol 345(15), 2001. - Easton and Wilterdink. Carotid Endarterectomy
Trials and Tribulations. Ann Neurology. Vol
35.1994. - Glaser. Neuro-ophthalmology. 3rd ed. 1999
- Mizener, et al. Ocular Ischemic Syndrome.
Ophthalmology, Vol 104, 1997. - Rizzo. Neuroophthalmologic Disease of the Retina.
Neuro-ophthalmology.
43
References
- Sacco et al. Guidelines for Prevention of Stroke
in patients with ischemic stroke or transient
ischemic attack. Stroke. Feb 2006. - Streifler, et al. The Risk of Stroke in Patients
with First-Ever Retinal vs Hemispheric Transient
Ischemic Attacks and High-grade Carotid Stenosis.
Archives of Neurology, Vol 52(3), 1995. - Wilterdink and Easton. Vascular event rates in
patients with atherosclerotic cerebrovascular
disease. Arch Neurology. Vol 49. 1992